Antifungals and Liver Safety: What You Need to Know About Drug Interactions and Risks
- Colin Hurd
- 5 December 2025
- 15 Comments
When you take an antifungal for a stubborn nail infection, a persistent yeast infection, or a life-threatening fungal illness, you’re not just fighting fungus-you’re putting your liver on the line. Many people assume these medications are safe because they’re prescribed by doctors. But the truth is, some antifungals carry serious risks of liver damage, and those risks don’t always show up until it’s too late.
Why Antifungals Can Hurt Your Liver
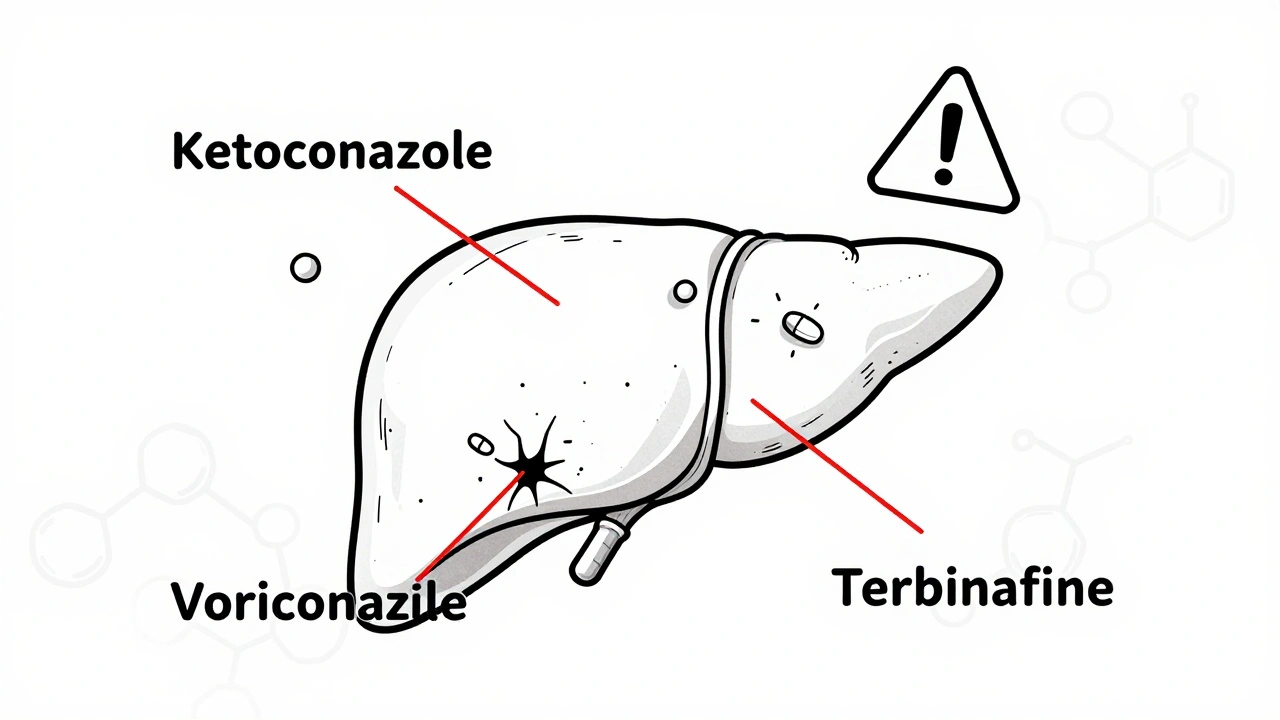
Antifungals don’t just target fungi. They also interfere with your body’s natural enzyme systems, especially those in the liver responsible for breaking down drugs. This interference can cause inflammation, cell death, or bile flow disruption-all leading to drug-induced liver injury (DILI). The risk isn’t the same across all antifungals. Some are far more dangerous than others.The azole class-like voriconazole, itraconazole, and ketoconazole-is the most notorious. Between 2004 and 2021, the FDA’s adverse event database recorded over 3,500 reports of liver injury linked to these drugs. Ketoconazole, once widely used for skin and nail fungus, was pulled from the market in Europe and restricted in the U.S. because it caused fatal liver damage in about 1 in 500 users. That’s not rare. That’s alarming.
Voriconazole and itraconazole aren’t far behind. A 2009 meta-analysis confirmed they’re significantly more likely to cause liver damage than fluconazole. Even fluconazole, often seen as the safest option, can cause problems if taken for more than two weeks, especially in older adults or those with existing liver conditions.
Terbinafine, commonly used for toenail fungus, has a lower overall risk-around 0.1% of users-but it still carries a black box warning. Why? Because when it does damage the liver, it can lead to sudden, severe failure. One patient in a 2023 Healthline forum described jaundice and fatigue after just five weeks of treatment. Their bilirubin levels soared to 12.3 mg/dL (normal is under 1.2). They spent three weeks in the hospital.
Who’s at Highest Risk?
Not everyone who takes antifungals will have liver problems. But some people are far more vulnerable.- People over 65: Their livers process drugs slower. The risk of DILI jumps to nearly 18 cases per 10,000 patients per year in this group.
- Those with pre-existing liver disease: Even mild fatty liver or hepatitis increases the chance of serious injury.
- People on multiple medications: Antifungals interact with dozens of common drugs, including statins, blood thinners, and antidepressants. These interactions can overload the liver.
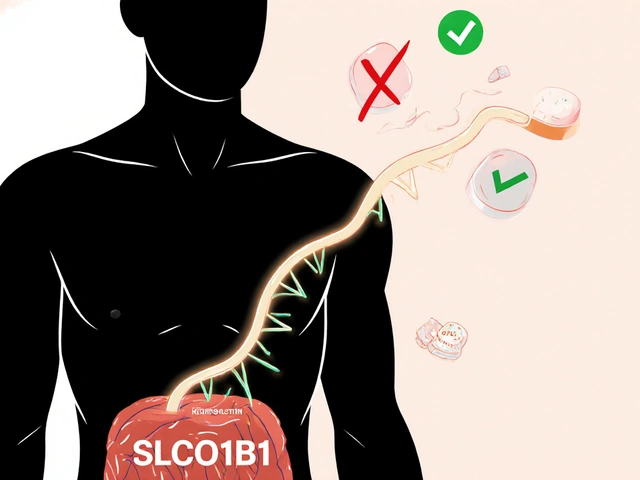
- People with CYP2C19 gene variants: A 2022 study found that certain genetic differences make voriconazole up to 3.7 times more likely to cause liver damage. This isn’t rare-it affects about 1 in 5 people of European descent.
Even healthy people aren’t immune. A 2020 study found that less than 40% of primary care doctors checked liver function tests before or during terbinafine treatment for nail fungus. That’s a dangerous gap. Many patients assume their doctor is monitoring them. They’re not always.
Drug Interactions You Can’t Ignore
Antifungals don’t just sit quietly in your system. They change how other drugs behave-often dangerously.Here’s what you need to watch for:
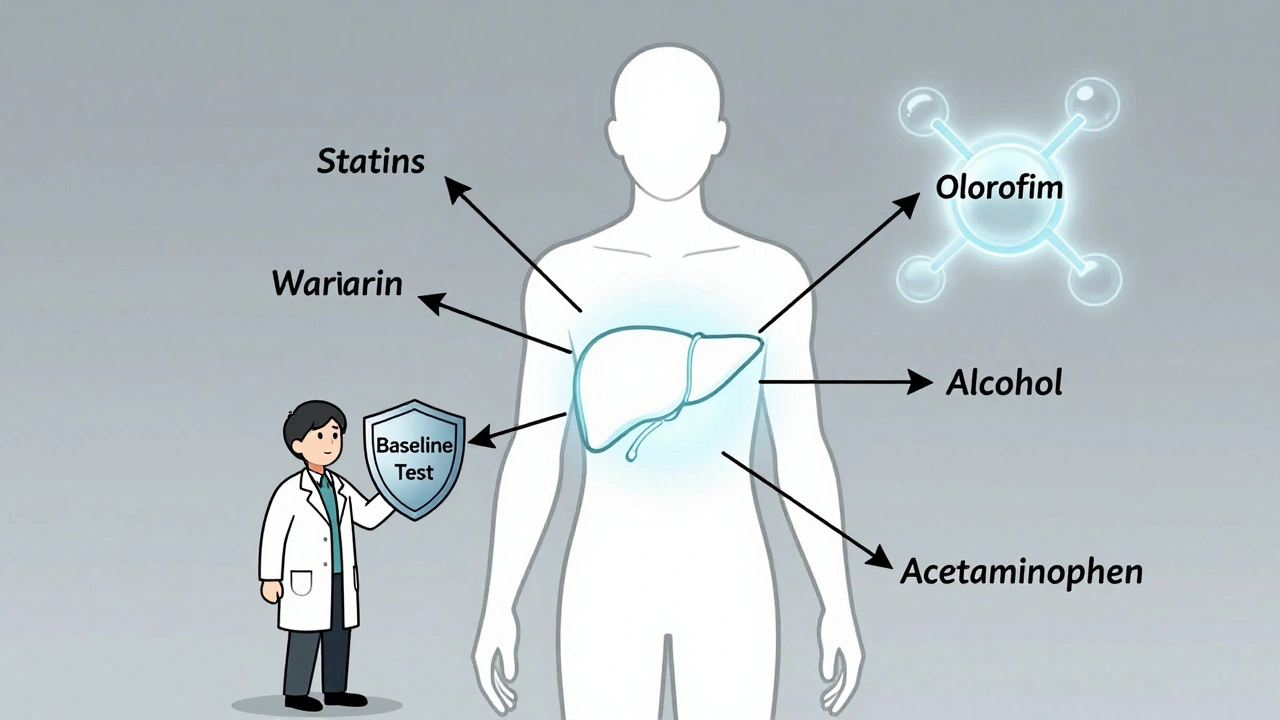
- Statins (like simvastatin or atorvastatin): Azoles can cause these cholesterol-lowering drugs to build up to toxic levels, leading to muscle breakdown and kidney failure.
- Blood thinners (warfarin): Voriconazole and itraconazole can increase warfarin levels, raising your risk of internal bleeding.
- Anti-seizure drugs (phenytoin, carbamazepine): These can lower antifungal levels, making them useless-or cause the antifungal to build up, increasing liver damage risk.
- Alcohol: Never mix antifungals with alcohol. It’s not just "avoid heavy drinking." Even one drink a day can worsen liver stress.
- Other liver-toxic drugs: NSAIDs like ibuprofen, acetaminophen (Tylenol), and some antibiotics can stack up with antifungals and push your liver into failure.
The FDA issued a formal warning in 2013: don’t combine ketoconazole with any other liver-damaging drug. That rule still applies to voriconazole and itraconazole-even if your doctor doesn’t mention it.

What Liver Monitoring Actually Looks Like
If you’re prescribed a high-risk antifungal, you need blood tests-not just once, but regularly. Here’s what experts recommend:- Baseline test: Before starting any systemic antifungal, get ALT, AST, bilirubin, and alkaline phosphatase checked.
- Weekly for the first month: Especially for voriconazole, itraconazole, and ketoconazole. Liver damage can happen fast-sometimes in under two weeks.
- Biweekly after that: Continue monitoring for the entire treatment period.
- For terbinafine: Test at week 4-6, then again if you’re on it longer than 8 weeks.
When do you stop? If your ALT or AST levels go above 3 times the upper limit of normal and you have symptoms like nausea, dark urine, or abdominal pain-stop the drug immediately. If levels hit 5 times the upper limit even without symptoms, stop anyway. Don’t wait for jaundice. By then, it’s often too late.
Many patients don’t realize these symptoms are warning signs. Fatigue? "Just tired." Nausea? "Stomach bug." Right upper quadrant pain? "Muscle strain." These are not normal. They’re red flags.
What’s Safer Today?
The good news? There are safer options now.Echinocandins like micafungin and anidulafungin are now first-line for serious fungal infections like candidemia. They’re given intravenously in hospitals and are generally gentler on the liver. But don’t be fooled-some data shows anidulafungin has the highest death rate among DILI cases. Why? Because it’s often used in patients who are already critically ill and have existing liver failure. It’s not the drug-it’s the patient’s condition.
Micafungin stands out as the safest echinocandin for liver function. Studies show lower rates of enzyme spikes than anidulafungin or caspofungin.
Fluconazole remains the go-to for many yeast infections because it’s cheap, effective, and low-risk-if used short-term. For nail fungus, terbinafine is still preferred over older azoles, but only if liver tests are done.
And here’s the future: new antifungals like olorofim and ibrexafungerp are in development with liver safety built into their design. Early trials show 78% fewer liver enzyme elevations than older azoles. They won’t be widely available until 2026, but they’re a sign that the medical community is finally taking this seriously.
What You Should Do Now
If you’re taking or about to start an antifungal, here’s your action plan:- Ask your doctor: "Which antifungal are you prescribing, and why? Is it the safest option for my liver?" Don’t accept "it’s the usual choice" as an answer.
- Get a baseline blood test before you start. Keep a copy.
- Know your meds: Make a list of every pill, supplement, and OTC drug you take. Bring it to your appointment.
- Watch for symptoms: Fatigue, loss of appetite, dark urine, yellow eyes, or pain under your right ribs? Call your doctor immediately.
- Don’t skip follow-up blood tests. Even if you feel fine.
- Never drink alcohol while on these drugs.
If you’re on terbinafine for nail fungus and your doctor didn’t order a blood test, ask for one. It’s not optional. It’s essential.
Why This Matters More Than You Think
Antifungal-induced liver injury isn’t common-but when it happens, it can be deadly. The global antifungal market is worth over $14 billion, and azoles still make up nearly half of it. But the tide is turning. Hospitals have cut ketoconazole use by over 90% since 2013. Guidelines have changed. New drugs are coming.But you can’t wait for the system to fix itself. You have to protect yourself. Your liver doesn’t have a voice. It can’t tell you it’s in trouble until it’s almost too late. You have to be the one who asks the questions, demands the tests, and speaks up when something feels wrong.
Antifungals save lives. But they can also end them-if you don’t know the risks.
Can antifungals cause permanent liver damage?
Yes, in rare cases. While most liver injuries from antifungals reverse after stopping the drug, some patients develop acute liver failure requiring a transplant. Ketoconazole and voriconazole have been linked to cases where liver damage was irreversible, even after discontinuation. Early detection and stopping the drug quickly are the best ways to prevent permanent harm.
Is terbinafine safe for long-term use?
Terbinafine is generally safe for the standard 6-12 week course for nail fungus, but long-term use increases liver risk. Studies show elevated liver enzymes are more common after 8 weeks. If you need longer treatment, your doctor should check your liver function every 4-6 weeks. Never take it for months without monitoring.
Can I take acetaminophen (Tylenol) while on antifungals?
Avoid it unless absolutely necessary. Acetaminophen is processed by the same liver enzymes as many antifungals. Combining them increases the risk of liver overload. If you need pain relief, ask your doctor about alternatives like gabapentin or low-dose NSAIDs (if kidney function is normal). Never exceed 2,000 mg of acetaminophen per day if you must use it.
Why is ketoconazole no longer used for skin infections?
Because it caused severe, sometimes fatal, liver injury in 1 out of every 500 users. The FDA restricted its use in 2013, and the European Medicines Agency withdrew it entirely in 2013. It’s now only allowed as a last-resort treatment for serious fungal infections when no other options exist. Topical ketoconazole shampoo is still available, but oral tablets are nearly obsolete.
Do I need genetic testing before taking voriconazole?
Not yet standard, but it should be. A 2022 study found that people with certain CYP2C19 gene variants have a 3.7 times higher risk of liver damage from voriconazole. If you’re on long-term voriconazole (like for invasive aspergillosis), ask your doctor about genetic testing. It’s available and could prevent serious injury.
How do I know if my liver is being monitored properly?
Ask for copies of your liver function test results before and during treatment. You should get tests at baseline, weekly for the first month, then every two weeks. If you’re on terbinafine, get tested at week 4-6. If your doctor doesn’t mention testing, bring it up. You have the right to know your numbers.
What Comes Next
The future of antifungal therapy is moving toward smarter, safer choices. AI systems are being trained to spot liver injury signals in real time. Genetic screening is becoming more accessible. New drugs are being designed to avoid liver toxicity altogether.But until then, your best defense is knowledge. Know your drug. Know your risks. Know your numbers. Don’t assume safety because a pill is prescribed. Your liver can’t speak-but you can. And you should.



Comments
Shayne Smith
I took terbinafine for athlete’s foot last year and felt like a zombie for six weeks. No one warned me. My doctor just handed me the script and said "take it daily." I didn’t even know my liver was a thing you had to check.
Now I’m paranoid about every pill I take.
December 6, 2025 AT 13:23
Max Manoles
The data on azole-induced DILI is robust, but the clinical implementation remains abysmal. A 2021 JAMA Internal Medicine analysis found that only 23% of primary care providers in the U.S. adhered to AASLD guidelines for baseline LFTs before prescribing systemic antifungals.
It’s not negligence-it’s systemic under-resourcing. We’re treating fungal infections like acne while ignoring hepatotoxicity risks that rival those of acetaminophen overdose.
Until labs are automated into EHR alerts and providers are financially incentivized to monitor, patients will keep falling through the cracks.
December 7, 2025 AT 06:02
Rashmi Gupta
Everyone’s scared of antifungals but no one talks about how often doctors prescribe them for things that don’t even need treatment.
How many nail fungus cases are just dry skin or psoriasis? We’re overmedicating because it’s easier than diagnosing properly.
December 8, 2025 AT 10:23
Kumar Shubhranshu
Ketoconazole was banned because it killed people but fluconazole is fine? That’s like saying heroin is bad but cocaine is safe because it doesn’t kill as fast
December 10, 2025 AT 03:47
Karen Mitchell
It’s disgusting that pharmaceutical companies still profit off drugs with known hepatotoxicity. They don’t care about your liver-they care about your insurance copay.
Doctors who prescribe without testing are complicit.
You’re not a patient. You’re a revenue stream.
December 11, 2025 AT 19:24
olive ashley
Did you know the FDA got a tip from a pharmacist in Ohio who noticed 7 patients on voriconazole all had jaundice within 10 days?
They buried it for 18 months.
Big Pharma knows. Doctors know. You’re just supposed to trust them.
That’s not medicine. That’s gambling with your organs.
December 12, 2025 AT 00:58
Ibrahim Yakubu
In Nigeria, we don’t even have access to liver tests for most people. We give terbinafine because it’s cheap and the pharmacist says it works.
People die silently. No one keeps records. No one cares.
But you Americans worry about your ALT levels? How lucky you are to even have a doctor who checks.
December 12, 2025 AT 05:01
Gwyneth Agnes
Don’t drink alcohol. Ever. That’s it. That’s the whole post.
December 12, 2025 AT 05:23
Mansi Bansal
One must interrogate the epistemological foundations of pharmaceutical safety paradigms. The reductionist biomedical model, which privileges pharmacological intervention over holistic liver resilience, is fundamentally flawed.
When we treat the liver as a metabolic factory rather than a sentient organ of detoxification and embodiment, we create conditions for iatrogenic catastrophe.
Perhaps the solution lies not in more blood tests, but in re-attuning to ancestral wisdom: turmeric, milk thistle, and fasting.
December 13, 2025 AT 12:32
Kay Jolie
As someone who’s been on long-term antifungals for invasive candidiasis, I can tell you: the real issue isn’t the drug-it’s the CYP450 polymorphism landscape. We’re living in the era of precision pharmacology, yet we’re still prescribing like it’s 1998.
Genomic sequencing should be standard before any azole, not a luxury for the wealthy.
And yes, I paid $2,000 out of pocket for my pharmacogenomic panel. Worth every cent.
December 15, 2025 AT 09:17
pallavi khushwani
I think we forget that the body isn’t just a machine. It’s alive. When you give it something toxic, even if it’s a medicine, it screams in ways we ignore.
Maybe the real question isn’t how to monitor liver damage-but why we keep putting it in danger in the first place.
What if the fungus isn’t the enemy? What if our system is just too full of stress, sugar, and silence?
December 15, 2025 AT 21:35
Dan Cole
Let’s be clear: the FDA’s adverse event database is garbage. It’s passive reporting. Most cases go unreported. The 3,500 figures are the tip of the iceberg.
And fluconazole being "safer"? That’s like calling a .22 safer than a .45. Both can kill you if you point them at your liver.
Stop pretending there’s a safe option. There’s only a less dangerous one-and you still need to test.
December 17, 2025 AT 02:44
Billy Schimmel
My grandma took terbinafine for her toenails. She didn’t tell anyone she felt weird. Thought it was just getting old.
Turns out she was one liver enzyme spike away from a transplant.
She’s fine now. But she doesn’t take anything without asking me first.
Just… ask your doctor. Seriously. It’s not hard.
December 18, 2025 AT 06:46
Nigel ntini
Great post. Seriously. This is the kind of info that saves lives.
But here’s what I want to add: if your doctor refuses to order baseline labs, get a second opinion. Or go to a walk-in clinic. Pay for it yourself if you have to.
Your liver doesn’t care if you’re insured. It just wants you to pay attention.
You’re not being paranoid. You’re being responsible.
December 19, 2025 AT 00:46
Priya Ranjan
Everyone’s focused on the drugs-but what about the people who sell them? The reps who push azoles to doctors because they’re profitable?
And the labs that don’t flag elevated enzymes because they’re too busy processing 500 samples a day?
This isn’t medical negligence. It’s corporate negligence.
And you’re paying for it-with your organs.
December 20, 2025 AT 18:24