Baclofen vs Alternatives: Comparison of Muscle Relaxants
- Colin Hurd
- 23 October 2025
- 13 Comments
Muscle Relaxant Decision Tool
Find Your Best Muscle Relaxant Match
Answer a few questions about your condition and preferences to get personalized recommendations for muscle relaxants.
Recommended Options
Important: This tool provides general guidance only. Always consult with your healthcare provider before making any medication changes.
Ever been prescribed Baclofen a central‑acting muscle relaxant used mainly for spasticity and wondered if there’s a better fit? You’re not alone. Many patients hit a wall with side effects, tolerance, or drug interactions and start scouting other options. This guide walks you through the most common alternatives, highlights where they shine or fall short, and gives you a clear decision‑making framework.
What is Baclofen?
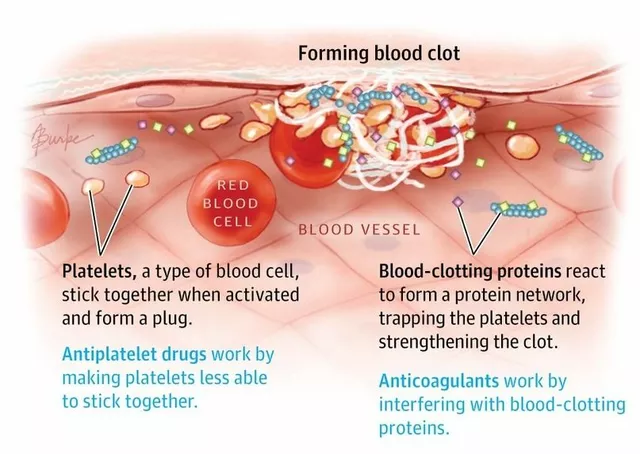
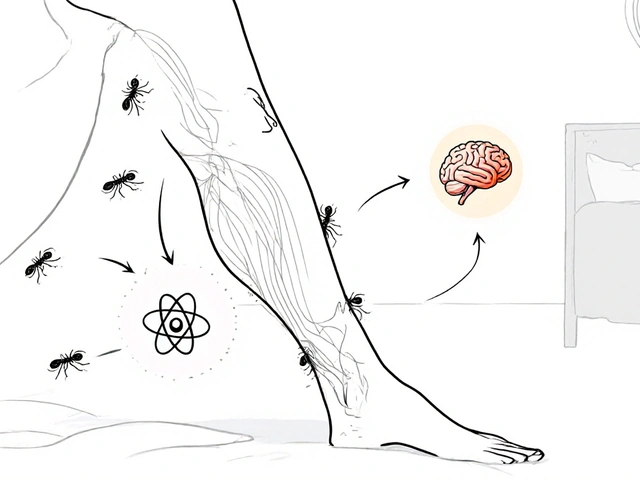
Baclofen works by mimicking the inhibitory neurotransmitter GABA gamma‑aminobutyric acid, which reduces nerve‑signal firing in the spinal cord. It’s FDA‑approved for treating muscle spasticity caused by multiple sclerosis, cerebral palsy, or spinal cord injury. Typical oral doses start at 5 mg three times daily and can be titrated up to 80 mg per day, while an intrathecal pump can deliver much higher concentrations directly to the spinal fluid.
Why Look at Alternatives?
Even though Baclofen is effective for many, several real‑world issues push patients to consider other drugs:
- Drowsiness or sedation that interferes with work or driving.
- Muscle weakness that makes daily activities harder.
- Withdrawal symptoms if the medication is stopped abruptly.
- Drug‑drug interactions, especially with other CNS depressants.
If you’ve experienced any of these, a switch might improve quality of life without sacrificing spasticity control.
Common Alternatives at a Glance
Here’s a quick snapshot of the most frequently prescribed substitutes.
- Tizanidine an alpha‑2 adrenergic agonist that reduces muscle tone by acting on spinal interneurons.
- Diazepam a benzodiazepine that enhances GABA‑A receptor activity, providing both muscle relaxation and anxiolysis.
- Cyclobenzaprine a tricyclic‑derived agent that works centrally to reduce muscle spasms.
- Methocarbamol a carbamate derivative that depresses central nervous system activity, often used for acute injuries.
- Gabapentin originally an anticonvulsant, it modulates calcium channels and can lessen neuropathic‑related spasticity.
Head‑to‑Head Comparison
| Drug | Mechanism | Typical Dose Range | Main Indications | Major Side Effects | Onset | Duration |
|---|---|---|---|---|---|---|
| Baclofen | GABA‑B receptor agonist | 5‑80 mg/day oral; up to 1000 µg/day intrathecal | Spasticity (MS, CP, SCI) | Drowsiness, weakness, constipation | 30‑60 min | 4‑6 h (oral), 24 h (intrathecal) |
| Tizanidine | Alpha‑2 adrenergic agonist | 2‑8 mg 3×/day | Spasticity, muscle spasms | Dry mouth, hypotension, liver enzyme elevation | 1‑2 h | 6‑8 h |
| Diazepam | Benzodiazepine (GABA‑A potentiation) | 2‑10 mg 2-4×/day | Spasticity, anxiety, seizures | Sedation, dependence, respiratory depression | 15‑30 min | 12‑24 h |
| Cyclobenzaprine | Central acting (similar to tricyclic antidepressants) | 5‑10 mg 3×/day | Acute muscle spasms | Dry mouth, drowsiness, cardiac arrhythmia | 30‑45 min | 12 h |
| Methocarbamol | Central nervous system depressant | 750‑1500 mg 4×/day | Acute musculoskeletal injuries | Dizziness, sedation, GI upset | 30‑60 min | 4‑6 h |
| Gabapentin | Calcium‑channel modulator | 300‑1200 mg 3×/day | Neuropathic pain, spasticity secondary to neuropathy | Weight gain, edema, ataxia | 1‑2 h | 5‑7 h |
How to Choose the Right Muscle Relaxant
Picking a medication isn’t a one‑size‑fits‑all decision. Use these five checkpoints to narrow down the choice:
- Underlying condition: If spasticity stems from central nervous system disease, Baclofen or Tizanidine often perform best. For short‑term injuries, Cyclobenzaprine or Methocarbamol may be more appropriate.
- Side‑effect tolerance: Patients who can’t handle sedation might favor Tizanidine (less drowsy) over Diazepam.
- Drug interactions: Tizanidine is metabolized by CYP1A2; avoid with fluvoxamine. Diazepam interacts with many CNS depressants. Check your current regimen.
- Renal/hepatic function: Gabapentin is renally cleared, while Tizanidine needs liver monitoring.
- Administration Preference: Oral Baclofen is convenient, but an intrathecal pump offers steady control for severe cases. If you dislike injections, stick to oral agents.
Write down your priorities, discuss them with a neurologist or physiatrist, and let the data guide the prescription.

Practical Tips for Switching Medications
Transitioning from Baclofen to another agent should be done under medical supervision. Here’s a safe roadmap:
- Taper Baclofen gradually over 1‑2 weeks to minimize withdrawal (e.g., reduce 10 mg every 2‑3 days).
- Start the new drug at a low dose and titrate upward while monitoring symptom control.
- Maintain a symptom diary - note spasm frequency, intensity, and any new side effects.
- Schedule follow‑up visits within 2‑4 weeks of the switch.
- Keep emergency contacts handy if severe rebound spasticity occurs.
Never attempt an abrupt stop; even a short gap can trigger worsening muscle tone.
Frequently Asked Questions
Can I take Baclofen and Tizanidine together?
Combining the two can lead to excessive muscle weakness and sedation. Doctors sometimes use a very low dose of each for refractory spasticity, but it must be done with close monitoring.
What’s the biggest advantage of Diazepam over Baclofen?
Diazepam works faster (within minutes) and also reduces anxiety, which can be helpful if spasticity is triggered by stress. The trade‑off is a higher risk of dependence.
Is an intrathecal Baclofen pump worth the surgery?
For severe, refractory spasticity that doesn’t respond to oral meds, the pump can provide smoother control and fewer systemic side effects. The decision hinges on overall health, infection risk, and willingness to maintain the pump.
Can I use over‑the‑counter supplements to replace Baclofen?
Supplements like magnesium or B‑complex may support muscle health but won’t substitute the strong GABA‑B activity Baclofen provides. Talk to a clinician before stopping any prescription.
How does the FDA categorize these muscle relaxants?
All listed drugs are FDA‑approved for specific indications. Baclofen, Tizanidine, and Diazepam have formal labeling for spasticity, while Cyclobenzaprine and Methocarbamol are approved for acute musculoskeletal conditions.
Armed with a clear comparison, you can have a productive conversation with your healthcare provider and find the muscle relaxant that fits your lifestyle best.

Comments
Celeste Flynn
If you're thinking about swapping out baclofen, the first thing to check is how your kidneys are handling drugs.
Many alternatives like gabapentin are cleared by the kidneys so a reduced eGFR can push you toward liver‑processed options.
On the liver side, tizanidine needs close monitoring of transaminases because it can raise them unexpectedly.
A good rule of thumb is to grab your latest lab panel before you even mention a switch to your neurologist.
Keep a notebook handy and write down every spasm, its intensity on a 1‑10 scale, and any side effects you notice each day.
This symptom diary becomes the evidence that guides dose titration and helps the doctor see what you need.
When you start a new med, begin at the bottom of the dosing range and increase slowly, watching for sedation or blood pressure changes.
For tizanidine, a 2 mg dose at night can be enough to smooth out morning stiffness without making you feel groggy.
If dizziness shows up, you might need to split the dose or add a small snack high in protein.
Remember that abrupt stopping of baclofen can cause rebound spasticity, which can be severe enough to require emergency care.
That's why a taper schedule of dropping 10 mg every few days is recommended, but always do it under supervision.
Some patients find a short “bridge” with low‑dose diazepam smoothes the transition because it covers the gap while baclofen tapers.
The downside of diazepam is the risk of dependence, so keep it under a month if you can.
With methocarbamol, the main issue is drowsiness, so schedule it for times when you don't need to drive.
Lastly, keep an eye on any new medications you add; many CNS depressants will amplify the sedative effect of these muscle relaxants.
By staying organized, communicating openly, and moving gradually, you can find a regimen that eases spasticity without the trade‑offs that got you frustrated in the first place.
October 23, 2025 AT 12:24
Shan Reddy
I’ve been on baclofen for a couple of years and the drowsiness finally kicked my work schedule. Switching to tizanidine gave me a clearer head, though the dry mouth was a nuisance. Make sure you get liver labs before you jump in, the docs usually ask for them. Tapering baclofen over ten days worked fine for me, no rebound spikes. Overall, a slower titration with the new drug saves you a lot of hassle.
October 23, 2025 AT 20:44
CASEY PERRY
Pharmacokinetic considerations underscore the necessity of renal clearance evaluation when substituting baclofen with gabapentinoids.
Moreover, GABA‑B agonism versus calcium‑channel modulation yields divergent neuromodulatory profiles.
Dose optimization should reflect these mechanistic disparities.
October 24, 2025 AT 03:41
Naomi Shimberg
One could argue that the presumption of superiority of any single muscle relaxant is scientifically untenable.
Clinical heterogeneity oftentimes renders comparative efficacy data moot.
While baclofen remains a mainstay, its adverse effect burden cannot be dismissed lightly.
The literature also indicates that patient-reported outcomes favor agents with minimal sedation.
Thus, a blanket recommendation fails to account for individual pharmacodynamic variability.
October 24, 2025 AT 13:24
kenny lastimosa
From a broader perspective, each medication choice reflects an underlying trade‑off between control and quality of life.
Patients navigate this balance daily, often without full awareness of the biochemical underpinnings.
The passive acceptance of side effects can inadvertently reinforce suboptimal therapeutic patterns.
Encouraging reflective dialogue between clinician and patient may subtly shift this dynamic.
October 24, 2025 AT 20:38
Dante Russello
When you’re charting a path away from baclofen, remember to involve your whole care team,-the neurologist, the pharmacist, even a physical therapist-because each perspective adds value.
Documenting your daily spasm score, your sleep quality, and any new meds, will give the team concrete data to work with.
Don’t forget to ask about potential drug–drug interactions, especially if you’re on antidepressants or antihypertensives, as these can amplify sedation.
A proactive approach, with clear communication and meticulous record‑keeping, often leads to smoother transitions.
October 25, 2025 AT 05:14
James Gray
I switched from baclofen to tizanidine last fall and honestly felt more awake at work, dont you think that’s great?
Just start low, go slow, and trust the process, its totally doable.
Your doc will probably monitor your liver enzymes, so keep that in mind.
Overall it’s a win‑win if you manage the dose right.
October 25, 2025 AT 13:01
Scott Ring
I hear you on the point about individual variability, and that’s something we all deal with.
It’s frustrating when a drug works for some and not for others, but sharing experiences helps us all navigate better.
Keeping an open mind, while staying critical, can lead to a personalized plan that actually works.
October 25, 2025 AT 21:54
Shubhi Sahni
Absolutely, the key is a gradual taper-10 mg every three days is a sensible schedule, and you should keep a symptom log, noting any increase in tone or discomfort, as this will inform any necessary adjustments, and never hesitate to call your provider if you notice a sudden spike.
Also, integrating gentle stretching routines can complement the pharmacologic changes, providing additional relief, and reinforcing the overall therapeutic strategy.
October 26, 2025 AT 03:34
Danielle St. Marie
Honestly, if you’re still hanging onto baclofen without trying any alternatives, you’re missing out on better options 🙄.
Doctors in our country push for modern therapy, and you should too 🚀.
Don’t be stuck in the past, move forward!
October 26, 2025 AT 11:54
keerthi yeligay
Check ur kidney funciton before you pick gabapentin it cant be cleared well if eGFR low.
Also watch out for swelling, it can be a sign of retension water.
October 26, 2025 AT 19:08
Peter Richmond
A thorough review of hepatic enzymes is indispensable prior to initiating tizanidine.
Subsequent dose titration should be guided by both efficacy and tolerability metrics.
October 27, 2025 AT 04:34
Bonnie Lin
Keep a daily spasm diary.
October 27, 2025 AT 12:54