Blood Thinners and NSAIDs: Why This Combination Can Cause Life-Threatening Bleeding
- Colin Hurd
- 18 January 2026
- 13 Comments
Blood Thinner and NSAID Risk Calculator
This tool calculates your relative bleeding risk when taking blood thinners with NSAIDs. Based on medical studies, the risk of internal bleeding can be significantly higher than taking blood thinners alone.
Risk Assessment
Safer Alternative: Acetaminophen (Tylenol) is the safest choice for pain relief when taking blood thinners.
If you're on a blood thinner like warfarin, Eliquis, or Xarelto, and you reach for ibuprofen or naproxen to ease a headache or sore knee, you're putting yourself at serious risk. This isn't a hypothetical warning - it's a well-documented, life-threatening combination that sends thousands to the emergency room every year. The truth is, blood thinners and NSAIDs don't just mix poorly; they amplify each other's dangers in ways most people don't understand.
How Blood Thinners and NSAIDs Work Together to Increase Bleeding Risk
Blood thinners - also called anticoagulants - don't actually thin your blood. They slow down the clotting process by interfering with proteins your body needs to form clots. This helps prevent strokes, heart attacks, and dangerous clots in the legs or lungs. Common ones include warfarin, rivaroxaban, apixaban, and dabigatran. NSAIDs - like ibuprofen, naproxen, diclofenac, and even aspirin - work differently. They block enzymes that cause inflammation and pain, but they also shut down platelets, the tiny blood cells that rush to seal cuts and scrapes. So while you're reducing swelling in your knee, you're also making it harder for your blood to stop bleeding. When you take both together, you're hitting your body's clotting system from two sides: one drug slows clot formation, the other disables the cells that start it. It's like turning off the brakes and cutting the steering wheel at the same time while driving downhill.The Numbers Don't Lie: How Much Higher Is the Risk?
A 2020 study tracking 200,000 patients over 10 years found that people taking NSAIDs along with blood thinners had more than double the risk of internal bleeding compared to those on blood thinners alone. The numbers vary by which NSAID you use:- Ibuprofen: 1.79 times higher risk
- Diclofenac: 3.3 times higher risk
- Naproxen: 4.1 times higher risk
- Gastrointestinal tract: 2.24 times higher risk
- Brain (intracranial hemorrhage): 3.22 times higher risk
- Lungs: 1.36 times higher risk
- Urinary tract: 1.57 times higher risk
Why This Interaction Is So Common - And So Dangerous
You’d think this would be obvious. But here’s the problem: millions of people are on blood thinners. In the U.S. alone, about 12 million take them daily. At the same time, 17 million people use NSAIDs every day - often without a prescription. Many take them for arthritis, back pain, or headaches, which are common in older adults - the very group most likely to be on blood thinners. Doctors know this. But they’re not always the ones who start the conversation. Patients often self-medicate. A 2022 JAMA study found only 43% of people on anticoagulants knew NSAIDs were risky. Two-thirds thought occasional use was safe. That’s a dangerous myth. Even more confusing: some people believe that because they’re taking a newer blood thinner like Eliquis, they’re immune to NSAID risks. They’re not. The interaction happens with every type - warfarin, rivaroxaban, apixaban, dabigatran, edoxaban. The mechanism is the same: platelet inhibition plus anticoagulation equals bleeding risk.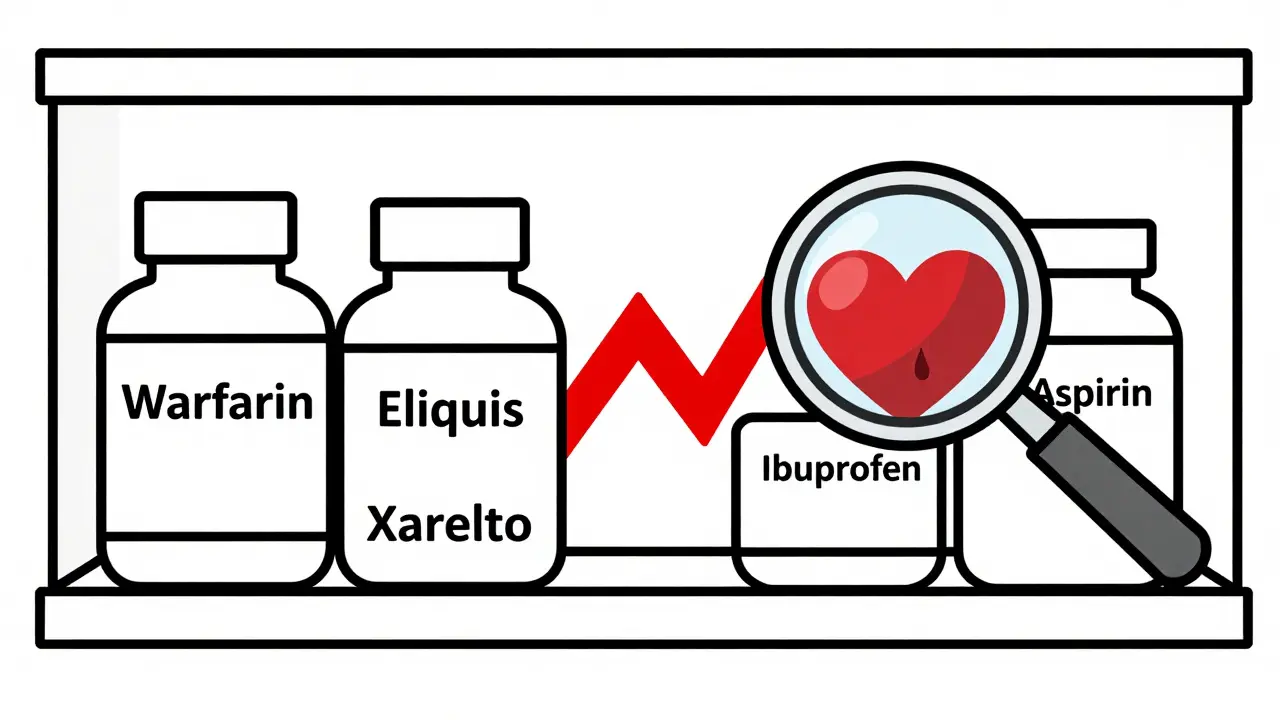
What to Do Instead: Safer Pain Relief Options
You don’t have to suffer in pain just because you’re on a blood thinner. There are safer choices.- Acetaminophen (Tylenol) is the top recommendation. It doesn’t affect platelets or clotting. But don’t overdo it - stick to 3,000 mg per day or less. Higher doses can harm your liver, especially if you drink alcohol or have other liver issues.
- Topical NSAIDs like diclofenac gel or ibuprofen cream may be safer. Since they’re absorbed through the skin, they don’t flood your bloodstream the same way pills do. Still, talk to your doctor - even topical forms carry some risk.
- Physical therapy, heat, ice, and stretching can reduce chronic pain without drugs. For arthritis or back pain, these are often more effective long-term than pills.
- Low-dose celecoxib (a COX-2 inhibitor) has shown slightly lower bleeding risk than traditional NSAIDs in recent studies. But it’s still not risk-free. The American College of Chest Physicians says it should only be used if absolutely necessary and under close supervision.
What If You’ve Already Taken Both Together?
If you took an NSAID once - say, for a bad headache - and you’re worried, don’t panic. One dose rarely causes serious bleeding. But watch for warning signs:- Bloody or black, tarry stools
- Vomiting blood or material that looks like coffee grounds
- Unexplained bruising or large bruises without injury
- Unusual bleeding from gums, nose, or cuts that won’t stop
- Sudden severe headache, dizziness, weakness, or confusion (possible brain bleed)
- Dark urine or pain when urinating (possible kidney or bladder bleed)
How to Stay Safe Long-Term
If you’re on a blood thinner, treat NSAIDs like you would alcohol or grapefruit juice - something you need to avoid unless your doctor says it’s okay. Here’s how to protect yourself:- Always tell every doctor, dentist, and pharmacist you’re on a blood thinner. Even if they don’t ask.
- Read OTC medicine labels. Many cold and flu remedies contain NSAIDs like ibuprofen or naproxen.
- Keep a list of all your medications - including supplements - and review it with your doctor every 6 months.
- If you need pain relief for more than a few days, ask about alternatives. Don’t assume NSAIDs are your only option.
- Know your INR if you’re on warfarin. High INR means your blood is taking longer to clot. NSAIDs can push it even higher.

What About Aspirin?
Aspirin is an NSAID - and it’s also a blood thinner. Even low-dose aspirin (81 mg) used for heart protection can increase bleeding risk when combined with other anticoagulants. Don’t assume it’s “safe” just because it’s low dose. If you’re on a blood thinner and taking aspirin, your doctor should have a clear reason for it - and you should be monitored closely.When NSAIDs Might Be Necessary - And How to Minimize Risk
Sometimes, there’s no alternative. A patient with severe arthritis might have no other way to move. In those rare cases, doctors may allow short-term NSAID use with strict safeguards:- Use the lowest effective dose for the shortest time possible
- Take it with food to reduce stomach irritation
- Use a proton pump inhibitor (like omeprazole) to protect the stomach lining
- Check INR more frequently if on warfarin
- Stop the NSAID at least 2 days before any surgery or dental work
Bottom Line: Don’t Guess. Ask.
This isn’t about being overly cautious. It’s about survival. The combination of blood thinners and NSAIDs isn’t just risky - it’s one of the most dangerous drug interactions in modern medicine. And it’s entirely preventable. You don’t need to suffer. You don’t need to risk bleeding in your stomach, brain, or lungs. There are safer options. But you have to be the one to ask for them. If you’re on a blood thinner and thinking of taking an NSAID - stop. Talk to your doctor. Or your pharmacist. Or call your anticoagulation clinic. Don’t assume it’s okay. Don’t rely on a label that says “over-the-counter.” Your life depends on knowing the truth.Can I take ibuprofen if I’m on Eliquis?
No. Ibuprofen increases your risk of bleeding by nearly 80% when taken with Eliquis or other direct oral anticoagulants. Even occasional use can lead to serious internal bleeding. Acetaminophen (Tylenol) is the safer choice for pain relief.
Is naproxen more dangerous than ibuprofen with blood thinners?
Yes. Naproxen carries a 4.1 times higher risk of bleeding compared to blood thinners alone - more than double the risk of ibuprofen. It also stays in your system longer, increasing the window of danger. Most guidelines recommend avoiding naproxen entirely if you’re on a blood thinner.
What’s the safest painkiller for someone on warfarin?
Acetaminophen (Tylenol) is the safest option, as it doesn’t interfere with blood clotting. Keep your daily dose under 3,000 mg to avoid liver damage. Avoid NSAIDs like aspirin, ibuprofen, and naproxen unless your doctor specifically approves it - and even then, only for a short time.
Can I use a topical NSAID cream instead of pills?
Topical NSAIDs like diclofenac gel carry less risk than oral pills because less of the drug enters your bloodstream. But they’re not risk-free. Some studies still show increased bleeding risk, especially with long-term use. Talk to your doctor before using them - and avoid applying them over large areas or broken skin.
How do I know if I’m bleeding internally from this combination?
Signs include black or bloody stools, vomiting blood, sudden severe headaches, unexplained bruising, dizziness, weakness, or dark urine. Bleeding can be silent at first. If you’re on a blood thinner and take an NSAID, and you feel unusually tired or weak, get checked immediately. Don’t wait for symptoms to get worse.
Do newer blood thinners like Xarelto have fewer interactions with NSAIDs?
No. All anticoagulants - whether warfarin, Xarelto, Eliquis, or Pradaxa - interact dangerously with NSAIDs. The mechanism is different than with warfarin, but the outcome is the same: increased bleeding risk. The danger isn’t tied to the type of blood thinner - it’s tied to the NSAID.
Should I stop NSAIDs before surgery if I’m on a blood thinner?
Yes. Stop ibuprofen at least 2 days before surgery, naproxen 2-3 days, and piroxicam 10 days. Your surgeon or doctor will give you specific instructions based on your medication and procedure. Never stop your blood thinner without medical advice - but NSAIDs should be paused.
Can I take baby aspirin with a blood thinner?
Only if your doctor specifically prescribes it. Baby aspirin is still an NSAID and a blood thinner. Taking it with another anticoagulant doubles your bleeding risk. Many people take it for heart protection, but if you’re already on a blood thinner, you likely don’t need it. Ask your doctor if it’s still necessary.




Comments
Josh Kenna
Just took ibuprofen for my back last week and didn’t think twice-now I’m sweating bullets reading this. Thanks for the wake-up call. I’m switching to Tylenol tomorrow.
January 18, 2026 AT 12:31
Erwin Kodiat
My grandpa’s on Xarelto and swears by his topical diclofenac gel. Said it’s the only thing that helps his knees without making him feel like he’s gonna bleed out. Still, I made him call his pharmacist before using it again-better safe than sorry.
January 19, 2026 AT 15:17
Christi Steinbeck
THIS. Every single person I know on blood thinners thinks NSAIDs are fine ‘once in a while.’ No. Just no. I’m a nurse and I’ve seen the ER reports. This isn’t a ‘maybe’-it’s a ‘call your doctor now.’
January 20, 2026 AT 09:09
sujit paul
Interesting how the pharmaceutical industry quietly pushes these lethal combos while selling you ‘safe’ alternatives like acetaminophen-whose liver toxicity is far more insidious. Who really benefits? The hospitals? The insurers? The system is rigged.
January 21, 2026 AT 00:14
Tracy Howard
Ugh. Americans and their OTC drug addiction. In Canada, you can’t even buy naproxen without a prescription anymore. We actually care about patient safety here. You people treat pharmacies like candy stores.
January 21, 2026 AT 21:56
Jake Rudin
It’s not just the pharmacology-it’s the epistemology. We’ve normalized risk. We’ve turned medical advice into a menu. ‘I’ll take the ibuprofen, hold the bleeding.’ We’ve forgotten that biology doesn’t negotiate. It responds. And it doesn’t care if you ‘only took one.’
January 23, 2026 AT 18:00
Lydia H.
I used to take naproxen for my arthritis until my dad had a GI bleed on warfarin. Now I do yoga, heat packs, and acupuncture. It’s slower, sure-but I’m still here. And I don’t have to wonder if I’m one pill away from a transfusion.
January 25, 2026 AT 14:22
Valerie DeLoach
For anyone reading this: if you’re on a blood thinner, make a list of all your meds-including supplements-and bring it to every appointment. I’ve seen patients forget fish oil, ginkgo, even high-dose vitamin E-all of which can amplify bleeding risk. Knowledge is armor.
January 25, 2026 AT 17:39
Lewis Yeaple
According to the 2020 JAMA study referenced, the relative risk increase for GI bleeding with concomitant NSAID use was 124% (95% CI: 1.17–1.31), not merely ‘2.24 times higher’ as stated. The latter is an absolute risk multiplier, which is misleading without baseline incidence data. Precision matters.
January 26, 2026 AT 09:51
Malikah Rajap
Can we talk about how doctors never tell you this? I was on Eliquis for AFib and took Advil for a migraine… and no one ever warned me. Not my cardiologist, not my PCP, not even the pharmacist who filled it. Why is this not on the label? Why?
January 27, 2026 AT 21:28
Aman Kumar
The real danger isn’t the NSAIDs-it’s the medical-industrial complex that profits from your ignorance. They sell you the blood thinner, then sell you the antacid to counter the bleed, then the transfusion, then the rehab. It’s a revenue loop disguised as healthcare.
January 27, 2026 AT 23:24
Astha Jain
lol i just took naproxen last night and im on xarelto… hope i dont die lol
January 28, 2026 AT 20:59
Jackson Doughart
Thank you for writing this with such clarity. I’ve been on warfarin for six years, and I’ve never once had a provider sit down and explain the NSAID risk in plain terms. I’ve since switched to acetaminophen and started physical therapy-my pain is manageable, and I sleep better knowing I’m not silently poisoning myself. Knowledge isn’t power-it’s survival.
January 29, 2026 AT 08:14