Can vomiting during pregnancy affect your mood and mental health?
- Colin Hurd
- 18 November 2025
- 15 Comments
If you’re pregnant and throwing up multiple times a day, you’re not just dealing with physical discomfort-you might also be feeling drained, anxious, or even hopeless. It’s not just in your head. Severe nausea and vomiting during pregnancy, known as hyperemesis gravidarum, doesn’t just empty your stomach-it can empty your emotional reserves too.
How nausea connects to your mind
Your body and brain are wired together in ways you might not realize. When you’re vomiting constantly, your cortisol levels rise. Cortisol is your body’s main stress hormone. High cortisol over days or weeks doesn’t just make you feel tired-it can mess with your sleep, appetite, and even your ability to think clearly. A 2023 study from the University of Melbourne tracked 1,200 pregnant women with severe nausea and found that 68% reported increased anxiety, and 41% showed signs of depression by week 16-long before most people expect emotional changes in pregnancy.
It’s not about being "too sensitive." It’s biology. Your brain is reacting to constant physical distress. When your body is in survival mode, your prefrontal cortex-the part that handles rational thought and emotional regulation-gets suppressed. That’s why you might cry over small things, snap at your partner, or feel guilty for not being "happy" about the pregnancy. These aren’t character flaws. They’re physiological responses.
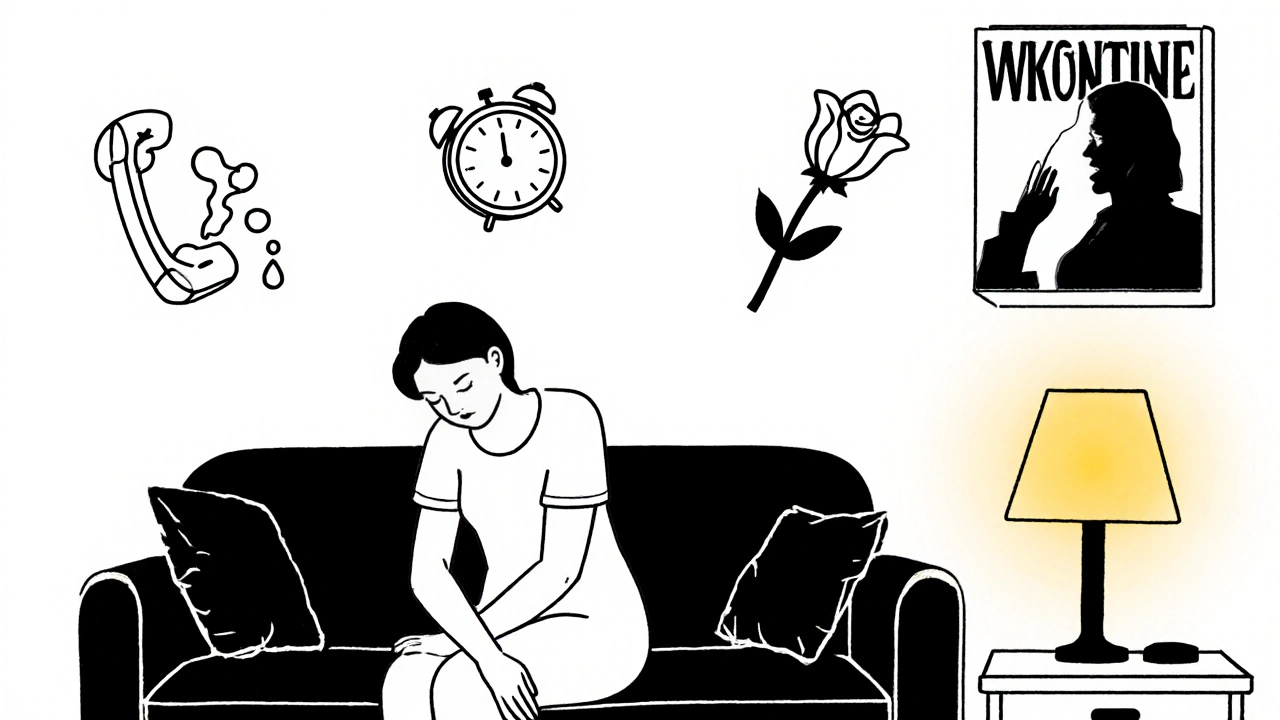
The cycle no one talks about
Here’s how it often plays out: you feel sick → you can’t eat → you feel weak → you can’t do daily tasks → you feel useless → you feel guilty → you feel more stressed → your nausea gets worse. It’s a loop, and it’s brutal.
Women who used to enjoy cooking now avoid the kitchen because the smell of food triggers vomiting. Those who loved going for walks now stay inside because the motion makes them sick. Social plans get canceled. Work becomes impossible. Friends don’t understand. Family says, "It’s just morning sickness-it’ll pass." But when it doesn’t pass, and you’re stuck in a cycle of sickness and shame, your mental health takes a hit.
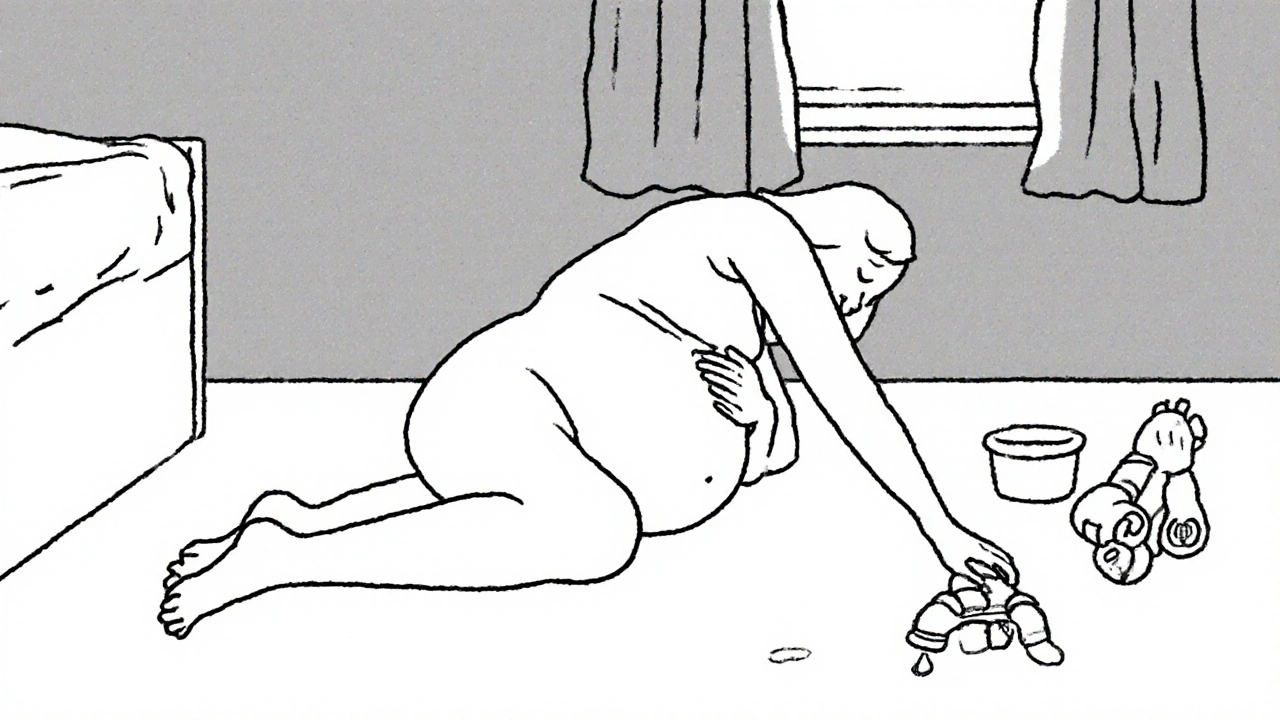
One woman in Perth, 32, told me she cried every morning because she couldn’t hold her toddler. "I used to be the one who picked him up, played with him, read to him. Now I’m the one lying on the floor, shaking, wondering if I’m failing as a mom before I’ve even met my baby." That’s not an exaggeration. That’s real.
What’s different about hyperemesis gravidarum?
Not all nausea is the same. Mild nausea that fades after 12 weeks? That’s common. But if you’re vomiting more than 3-4 times a day, losing weight, urinating less than usual, or feeling dizzy when you stand up-you’re likely dealing with hyperemesis gravidarum (HG). It affects about 1-3% of pregnancies, but its impact is far from rare.
Women with HG are three times more likely to develop anxiety disorders during pregnancy and twice as likely to experience postpartum depression. A 2024 review in the Journal of Obstetric Medicine found that HG was the strongest predictor of prenatal depression among all pregnancy symptoms-even stronger than a history of depression before pregnancy.
The key difference? HG doesn’t go away with time. For some, it lasts until delivery. And while your body is fighting to keep nutrients in, your mind is fighting to stay sane.
Why mental health gets ignored
Doctors often focus on weight loss, electrolytes, and IV fluids. That’s important. But if your mental state isn’t checked, you’re left alone with the emotional fallout.
Many women don’t bring it up because they think: "I should be grateful I’m pregnant. Others have it worse." Or they fear being labeled "hysterical" or "overreacting." But mental health isn’t a luxury-it’s part of prenatal care. Just like you get blood tests and ultrasounds, you need emotional check-ins.
Ask your provider: "How is my mental health holding up with this nausea?" If they brush you off, find someone who won’t. A midwife, OB-GYN, or perinatal psychologist who understands HG is not a luxury. It’s necessary.
What helps-beyond anti-nausea meds
Medications like Diclegis or Zofran can help with vomiting, but they don’t fix the loneliness, guilt, or fear. Here’s what actually helps:
- Therapy tailored to pregnancy: CBT (cognitive behavioral therapy) works well for pregnancy-related anxiety. A therapist can help you reframe thoughts like "I’m failing" into "My body is under extreme stress, and that’s not my fault."
- Support groups: Online communities like the Hyperemesis Education and Research Foundation have thousands of women sharing real experiences. Reading "me too" messages can be healing.
- Low-pressure routines: Don’t force yourself to be productive. Rest is treatment. Even 20 minutes of quiet with a heating pad or calming music counts.
- Partner education: Show your partner this article. Let them know your mood swings aren’t about them-they’re about your body being overwhelmed.
Some women find relief with acupuncture or ginger supplements (625 mg, 4x daily), but only under medical supervision. Don’t try unproven remedies-your body is already under strain.

When to get help-right now
If you’re feeling:
- Hopeless, worthless, or like you don’t want to keep going
- Overwhelmed by guilt or shame about your pregnancy
- Unable to care for yourself or others
- Having thoughts of harming yourself
-call a crisis line immediately. In Australia, you can reach Lifeline at 13 11 14 or PANDA (Perinatal Anxiety & Depression Australia) at 1300 726 306. These services are free, confidential, and staffed by people who’ve worked with pregnant women in crisis.
You are not weak for needing help. You are human.
You’re not alone, even when it feels that way
There’s a quiet epidemic happening in homes across Australia: women suffering silently from nausea that’s stealing their joy. They’re not broken. They’re not failing. They’re fighting a physiological storm that no one talks about enough.
Your mental health matters as much as your physical health during pregnancy. If vomiting is keeping you from sleeping, eating, or feeling like yourself-it’s not just a symptom. It’s a signal. Listen to it. Ask for help. Reach out. You deserve care-not just for your baby, but for yourself.
Can vomiting during pregnancy cause depression?
Yes. Severe vomiting, especially hyperemesis gravidarum, is strongly linked to depression during pregnancy. Constant physical stress, sleep loss, isolation, and guilt can trigger depressive symptoms. Studies show women with severe nausea are up to twice as likely to develop depression compared to those with mild or no nausea.
Is it normal to feel guilty about being sick during pregnancy?
Yes, it’s common-but not rational. Many women feel guilty because society expects pregnancy to be joyful. But your body isn’t failing-it’s overwhelmed. Feeling guilty doesn’t mean you’re ungrateful. It means you’re under pressure. Acknowledge the feeling, then remind yourself: your worth isn’t tied to how well you’re "handling" sickness.
When should I see a doctor about my nausea and mood?
See a doctor if you’re vomiting more than 3-4 times daily, losing weight, feeling dizzy, or noticing changes in your mood-like crying often, losing interest in things you used to enjoy, or feeling hopeless. Don’t wait until it’s "bad enough." Early support makes a big difference in both physical and mental recovery.
Can therapy help with nausea-related anxiety?
Yes. Cognitive behavioral therapy (CBT) has been shown to reduce anxiety and depression in pregnant women with severe nausea. Therapy helps you challenge negative thoughts like "I’m a bad mom" or "This will never end," and replace them with facts: "My body is under stress, and that’s temporary. I’m doing my best."
Are there safe medications for nausea that won’t hurt my mental health?
Yes. Medications like Diclegis (doxylamine/pyridoxine) and Zofran (ondansetron) are approved for use in pregnancy and can reduce vomiting enough to improve sleep, eating, and mood. Reducing nausea often improves mental health-not because the meds "fix" your mood, but because they give your body space to recover. Always discuss options with your provider.
What to do next
Start small. Today, text one person: "I’ve been really sick and it’s affecting my mood. I need someone to talk to." That’s it. No grand gesture. Just one message.
If you’re a partner, friend, or family member-don’t say "it’ll pass." Say: "I see how hard this is. What do you need right now?" Presence matters more than solutions.
You’re not alone. You’re not weak. And you’re not failing. Your body is doing something extraordinary-and it’s okay if it’s breaking you down a little while it does.




Comments
Ronald Stenger
This is just another liberal scare tactic to get women to take more pills and see more therapists. Back in my day, women just sucked it up and didn’t whine about every little stomach ache. Pregnancy isn’t a disability. Get over it.
November 18, 2025 AT 22:11
Samkelo Bodwana
Look, I get that this is a tough topic, but I think the real issue here is how we’ve medicalized every single emotional response in pregnancy. I’ve seen women in rural South Africa go through labor with no painkillers, no doctors, and still bond with their babies just fine. Maybe the problem isn’t the vomiting-it’s the expectation that you need to feel ‘joyful’ every second. Let people feel what they feel without turning it into a clinical diagnosis.
November 20, 2025 AT 03:52
Emily Entwistle
OMG YES THIS. 🥺 I had HG with both kids and no one told me it would make me cry over spilled water. I thought I was just being dramatic until I found a support group. You’re not broken-you’re just in a biological hurricane. Also, ginger chews are life. 🍊✨
November 21, 2025 AT 00:54
deepak kumar
As someone from India where this is rarely discussed, I’m glad someone finally put this out there. In my village, women are told to ‘drink warm water and pray.’ But the truth? Many suffer silently. I had a cousin who lost 15kg and was told she was ‘too emotional.’ She didn’t get help until she nearly collapsed. Please, if you’re reading this and feeling this-reach out. You’re not alone.
November 21, 2025 AT 13:11
Dave Pritchard
This is such an important perspective. I’ve seen friends go through this and it’s heartbreaking to watch someone you love feel guilty for being sick. The key takeaway? Mental health isn’t optional in pregnancy. It’s part of the treatment plan. If your provider doesn’t ask about your mood, ask them why.
November 21, 2025 AT 15:43
kim pu
Okay but has anyone considered that this is just Big Pharma’s way of selling Zofran to pregnant women? They’re not trying to help-they’re trying to make you dependent. Also, why is no one talking about how the ‘support groups’ are just echo chambers for over-medicalized anxiety? Wake up. This is all manufactured. 🤔
November 22, 2025 AT 00:56
malik recoba
i read this and just cried. not because i’m pregnant, but because my sister went through this and no one got it. she felt like a failure. just wanted to say… you’re not. you’re surviving. that’s enough. 💙
November 22, 2025 AT 17:30
Sarbjit Singh
Bro, I’m a dad and I had no idea this was so bad. My wife had HG and I thought she was just being moody. I didn’t know her brain was literally being rewired by stress. I’m so sorry I didn’t get it. Now I bring her ginger tea every morning. Small things matter.
November 23, 2025 AT 00:58
Angela J
Wait… are you telling me that vomiting during pregnancy is linked to depression? Hmm… I wonder if this is all connected to the 5G towers in maternity wards… or maybe the vaccines? I mean, why now? Why is this only being talked about since 2023? Coincidence? I think not. 🕵️♀️
November 24, 2025 AT 13:13
Sameer Tawde
You got this. One text. One breath. One day at a time. You’re not failing. You’re fighting. And that’s courage.
November 25, 2025 AT 20:46
Alex Czartoryski
So let me get this straight-you’re saying vomiting for months is a mental health crisis? Bro. I once threw up after eating a burrito and I didn’t need a therapist. This is why America’s falling apart. Everyone’s a victim now. Just toughen up.
November 27, 2025 AT 08:25
Victoria Malloy
I read this while lying on the couch, too nauseous to move. It felt like someone finally whispered the truth I was too tired to say out loud. Thank you.
November 29, 2025 AT 00:39
Gizela Cardoso
I didn’t know how to explain it to my partner until I sent him this. He finally understood why I couldn’t cook dinner. It’s not laziness. It’s survival. Thank you for writing this.
November 30, 2025 AT 08:46
Andrea Johnston
Oh my god, I’m not the only one? I cried when my cat sneezed. I canceled my sister’s baby shower because I thought the smell of cake would kill me. I thought I was broken. Turns out I was just… human.
December 1, 2025 AT 14:42
Scott Macfadyen
My wife had HG. She didn’t cry. She just… went quiet. We thought she was okay. Turns out she was just too exhausted to talk. This article? It’s the missing piece. We’re getting her a therapist next week. Thanks for saying what no one else did.
December 1, 2025 AT 15:54