Effexor (Venlafaxine): Uses, Side Effects, and Real-Life Insights in 2025

- Colin Hurd
- 13 June 2025
- 16 Comments
Anyone who’s ever questioned whether life can get a bit more predictable after a doctor’s visit has probably never heard about feeling floored by an antidepressant name. 'Effexor' might sound more like a high-tech gadget than a prescription, right? Yet, here it is—in 2025, it’s still a staple for folks managing depression, anxiety, and a handful of other mood issues. Even on the footy field sidelines here in Perth, I hear mates swap stories about the ups, downs, and curveballs of this little capsule. It’s a name that pops up everywhere mental health is talked about—whether you’re a twenty-something student, someone muddling through the chaos of parenthood, or a retiree who just wants a brighter day.
What Exactly Is Effexor (Venlafaxine)?
Effexor, or by its less snappy name, venlafaxine, isn’t your run-of-the-mill mood lifter. It belongs to a group called SNRIs—serotonin-norepinephrine reuptake inhibitors. As mouthfuls go, that takes the cake. Basically, SNRIs tweak brain chemistry by boosting two of your major mood messengers: serotonin and norepinephrine. Why does that matter? Both those chemicals play a big part in how your brain processes stress, emotion, and your general 'get up and go.' So, instead of letting all that serotonin and norepinephrine go to waste, Effexor keeps them hanging around your brain just a little bit longer than usual.
Doctors typically prescribe Effexor to people battling major depressive disorder (that’s the heavy-hitting kind of depression—not just a bout of the blues), generalised anxiety disorder, and social anxiety disorder. It’s also been used for panic disorder. In Australia, the typical starting dose is 75 mg per day, taken with food—although some folks start even lower, especially if your doctor wants to ease you in gently or you’re a bit older. There’s even an extended-release version (Effexor XR), letting you take it once a day, which is handy if you struggle to remember your morning and night pills.
Fun fact: in the past year, about 1.2 million scripts for venlafaxine were filled across Australia. That’s a staggering number if you imagine every one as a story—a student trying to focus, a mum balancing work stress, someone in recovery after a loss. Here in Perth, GPs mention it almost as much as paracetamol for persistent mood concerns.
Effexor first hit pharmacy shelves in the 1990s. Since then, its generic has become so mainstream you’ll find it on almost every PBS-subsidised list at your local chemist. Even though it’s older than some of the other antidepressants (like Pristiq or Lexapro), it’s still chosen because it can work when others don’t. Some people who don’t respond to basic SSRIs give Effexor a go and find themselves finally getting out of mental quicksand.
How Effexor Works and What Makes It Different
Unlike medications that just fiddle with serotonin (we’re looking at you, Prozac and Zoloft), Effexor boosts both serotonin and norepinephrine. The science behind it is actually pretty cool. Your brain’s like a giant crowd at a music festival—moods and nerves get tossed around in all directions. Effexor blocks the reuptake of those two chemicals, meaning more 'good vibes' can float around your synapses, relaying happier and calmer messages.
That’s why it sometimes helps when other drugs flop. Some doctors lean on Effexor for public speaking anxiety, tough-to-treat depression, or cases with lots of physical symptoms (like headaches or aches that come along with sadness). Now, Effexor doesn’t work right away—it usually takes at least two weeks to notice any shifts, though a lot of folks don’t feel much until week four or five. It’s a slow burn, but that’s normal for this kind of medication.
Compare Effexor to SSRIs and you’ll spot some differences: the side effects can be stronger (more on that in a bit) but it may also deliver better results for stubborn cases. It can even tackle what doctors call 'treatment-resistant depression,' where other pills just don’t cut it. You can see why doctors keep it on their favourites list even in 2025.
And here’s a bit of data for anyone who loves numbers: Research from the National Prescribing Service (NPS) in Australia showed that Effexor’s effectiveness rates for major depression hover around 60-67%. That’s a solid edge above a placebo, and slightly above several common SSRIs. What’s more, the relapse rates tend to be lower if you stick with Effexor at the right dose. Of course, medication is rarely a one-size-fits-all deal, but those stats give a real-world boost to Effexor’s reputation.
In some cases, venlafaxine is also used 'off-label' for hot flashes in menopause and even for nerve pain. My sister-in-law’s GP suggested it for night sweats, which blew her mind since she’d always thought 'antidepressant' meant 'sad people only.'
Here’s a table just to break down the key differences between Effexor and some popular antidepressants:
| Name | Type | Main Uses | Common Side Effects | Unique Features |
|---|---|---|---|---|
| Effexor (Venlafaxine) | SNRI | Depression, Anxiety, Panic, Off-label: Hot flashes | Headache, nausea, sweating, withdrawal | Boosts BOTH serotonin and norepinephrine |
| Sertraline (Zoloft) | SSRI | Depression, Anxiety, PTSD, OCD | Nausea, sleep issues, sexual side effects | Often well-tolerated; widely prescribed |
| Paroxetine (Aropax) | SSRI | Depression, OCD, Panic, Anxiety | Dry mouth, sleepiness, sexual side effects | More sedating; short half-life |
| Duloxetine (Cymbalta) | SNRI | Depression, Anxiety, Nerve pain | Dry mouth, tiredness, sweating | Treats pain and mood |
If you’re diving into the world of Effexor, knowing what it actually does—on paper and in your brain—makes the journey a little less confusing.
What to Expect: Side Effects and Withdrawal
The part most people worry about with Effexor? The side effects. You hear some wild stories: one mate said he could 'taste metal,' and another compared the first week on Effexor to riding a bus during a cyclone. According to the latest 2025 clinical reviews from the Australian Therapeutic Goods Administration (TGA), the most common side effects are pretty standard for antidepressants but tend to be a bit more intense at higher doses.
Here’s the usual roll call: nausea, headaches, sweating, dry mouth, trouble sleeping, drowsiness or feeling wired, dizziness, loss of appetite, and sometimes, increased anxiety for a week or two. If you’ve ever forgotten to feed the dog before your morning coffee, you know the feeling—your whole system’s a little 'off.' The first few weeks can be wonky, but sticking with it (unless something feels really wrong) usually leads to a smoother ride by week three or four. Very rarely, some people notice higher blood pressure, so your doctor will probably check that now and then, especially at doses above 225 mg daily.
Here’s a kicker: Effexor’s reputation for tough withdrawals isn’t urban legend. That’s why the advice is never to quit cold turkey. If you skip a dose or try stopping suddenly, there’s a decent chance you’ll meet the 'Effexor discontinuation syndrome.' The symptoms can look like the flu (chills, muscle aches), or even cause strange shocks in your head—people call them 'brain zaps.' You might also feel irritable, dizzy, or a bit out of body for a few days (or weeks, if you really rush it). The secret is to taper, slowly, with your doctor’s help. From Aussie Reddit forums to local pharmacist chats, the message is clear: don’t go rogue with your doses.
In my house, with a brainy daughter and curious pets, the topic of medications is just part of dinner chat. Aurelia always asks about side effects before trying new things (even new dog biscuits for Max), and I’m the same when it comes to meds. The more you know, the less you worry.
Some side effects settle on their own. If you get stuck with something annoying, mention it to your doctor—it might just need a dose change or a bit of patience. Of course, any signs of severe allergic reaction or thoughts of self-harm mean immediate help—no waiting it out. And, as with all antidepressants, sometimes things get worse before they get better, so regular check-ins are non-negotiable.
Tips for managing side effects:
- Take your dose with food if you feel queasy.
- Try taking it in the morning if it keeps you awake, or at night if it makes you sleepy.
- Stay hydrated and go easy on caffeine.
- Consider using a weekly pill organiser—forgetting doses is a fast track to feeling rough.
Not everyone will get every side effect, just like Jasmine (our Siamese) only reacts to certain cat treats. But listening to your body and keeping your care team in the loop makes a world of difference.

Everyday Life with Effexor: What Real People Experience
If you read internet forums, chat with family, or swap stories in the lunchtime queue, you quickly realise taking Effexor isn’t a one-track experience. Some folks say the fog lifts in a few weeks—colors look brighter, and the world feels less heavy. Others only feel subtle shifts at first, especially if they start at a very low dose. There’s a whole spectrum, but real stories give some powerful clues about what happens when Effexor kicks in.
One guy in my local cycling group reckons Effexor gave him the 'oomph' to finally get back on the road after months of “not caring.” Another friend said it made her hands sweat for a month but, at the same time, helped her sleep through the night after years of anxiety-related insomnia.
People often talk about side benefits too. For some, physical pain tied to their mood actually eases up. There are also stories about better concentration—students and workers who felt like their brains were finally firing on all cylinders again. It’s not usually immediate, so tracking subtle changes is key. Some keep a journal (yes, old-school pen and paper) to look back and see what’s shifted after a few weeks or months.
The flip side? A handful find it just doesn’t fit. They might notice too many side effects, or that their particular type of sadness or anxiety isn’t budging. That’s why regular check-ins with your GP or psychologist are so helpful. Fine-tuning isn’t just possible; it’s expected.
One thing that comes up a lot in Aussie communities is the impact on relationships and day-to-day life. Yes, Effexor can sometimes affect libido or appetite, but for lots of people the trade-off (feeling actually alive again) is firmly in their favour. Partners and family members also notice—you’ll hear parents and flatmates say, 'You seem lighter,' or 'You haven’t cancelled dinner in weeks.' The medication isn’t magic, but when it helps, it can absolutely shift the mood in an entire household.
There are even stories of folks using Effexor after trying a run of other options. Maybe they tried SSRIs without luck, or had patchy results from talk therapy alone. Giving Effexor a fair go—with patience and slow dose adjustments—sometimes changes the whole playing field. The trick, if you can call it that, is sticking with it just long enough to know for sure.
Dosage Tips, Drug Interactions, and Practical Advice
The 'how to take it' side can be surprisingly technical, even if you’re a pro at swallowing pills. Starting low (often 37.5 mg daily for sensitive folks), doctors may crank up the dose slowly, aiming for the sweet spot where you feel better but don’t live in a cloud of side effects. Effexor XR is easier for most—it’s taken once a day, usually with breakfast. The regular-release version splits your dose morning and night, which means if you miss one, you might feel it fast.
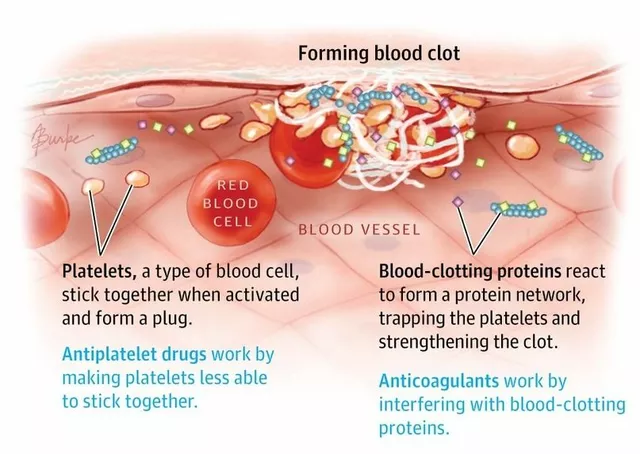
If you’re juggling Effexor and other meds, pay close attention. Effexor can interact with blood thinners, migraine meds (the 'triptans'), and even some herbal supplements like St John’s Wort. The big concern is 'serotonin syndrome,' where you get too much serotonin bouncing around at once. Symptoms can be pretty nasty: confusion, fever, twitchy muscles, and even seizures in severe cases. Honestly, if you’re mixing meds, best to run everything by your doctor or pharmacist and let them double-check for clashes—it's safer than playing Dr Google.
Alcohol? Technically, one or two drinks won’t blow up your treatment, but many people report that booze brings on the sads or ramps up side effects. That means it’s usually worth cutting back or saying no, at least at first. Plus, your liver and sleep quality will thank you.
A couple of other quick-fire tips from local pharmacists and people who’ve stuck with Effexor:
- Always refill ahead of time—missing doses can tank your progress.
- Store it somewhere cool, dry, and out of reach of curious kids and pets (yes, even clever Border Collies).
- If you get extended-release tablets, don’t crush or chew—swallow whole for the right effect.
- If you’re pregnant, planning a family, or breastfeeding, chat with your specialist. Effexor’s safety profile in pregnancy is still debated, though some women use it with close supervision.
- Think through timing with life changes—switching jobs, moving house—since those are stressful even without med adjustments.
One last little tip: keeping hydrated and adding light exercise can soften side effects and give your mood a glow-up quicker than you’d think. Walking Max on the beach works wonders when my brain feels foggy. Sometimes it’s the daily routines that really do help medication work better.
Frequently Asked Questions and Myths About Effexor
The longer a medication’s around, the fatter the file of myths and misunderstandings. Let’s knock out a few Effexor legends you’ll spot on forums or in overheard café chats:
Myth 1: “Effexor will change your personality.”
Nope—it supports you in pulling out of a slump, but you’re still you. If you feel “not yourself,” tell your doctor. Sometimes an adjustment or slower titration clears it up.
Myth 2: “It’s not as good as newer antidepressants.”
Actually, Effexor is still a heavy hitter for folks who didn’t get results from more modern meds. Its dual-action gives it real spark for certain cases.
Myth 3: “Withdrawal isn’t a big deal—just stop if you hate it.”
Ignoring tapering advice is like taking a jump off Cottesloe pier in July. Slow steps make for a smoother ride—always plan your exit strategy with your GP.
Myth 4: “You have to stay on it for life.”
Not true. Some people use Effexor for a handful of tough months; others need it longer or cycle on and off. The plan is based on your experience, not some mythical forever rule.
Myth 5: “Everyone gets all the bad side effects.”
Most people tolerate Effexor well by month two, as long as they keep their dose steady and don’t go astray with timings. Again, every body reacts a bit differently—your journey is unique.
If in doubt, try jotting down your symptoms, questions, and side effects—bring that list to your next check-up. Doctors love real-life data and it keeps your treatment on track.
And if you’re just starting out? Don’t go it alone. Chat with others, connect with a reputable support group (Aussie-run groups are great for local advice), or even have a quick check-in with your pharmacist. Mental health isn’t a straight path, but sharing what you learn makes every step easier.



Comments
Patrick Culliton
Effexor isn’t the miracle pill some hype up.
June 13, 2025 AT 12:53
Andrea Smith
While the overview provides a solid foundation, it is essential to recognize that individual response to venlafaxine can vary considerably. The dual‑action mechanism offers a valuable alternative for patients unresponsive to SSRIs, yet clinicians must remain vigilant regarding dose‑related hypertension. Moreover, the discussion of off‑label applications, such as vasomotor symptom relief, should be approached with caution and thorough patient counseling. It is commendable that the article emphasizes gradual titration, as abrupt changes are a well‑documented precipitant of discontinuation syndrome. In sum, a balanced perspective that integrates clinical vigilance with patient‑centered care will optimise therapeutic outcomes.
June 14, 2025 AT 13:20
Gary O'Connor
yeah, i’ve seen a lot of mates on effexor and most of ‘em say the first week feels like a weird rollercoaster. the nausea and headachz kinda melt away after a couple weeks if you stick with it. just make sure you take it with food ‘cause the stomach can get upset fast. also, don’t be scared to chat with your doc about any weird vibes, they’ll adjust the dose.
June 15, 2025 AT 17:06
Justin Stanus
Effexor’s side‑effect profile can feel like a relentless barrage, especially when you’re already battling anxiety. The ‘brain zaps’ during tapering are more than just a myth; they’ve been documented and can be quite distressing. Forget the hype about it being a quick fix-patience and professional guidance are non‑negotiable. If you’re not prepared for the withdrawal grind, you’ll end up worse off.
June 16, 2025 AT 20:53
Claire Mahony
It’s true that withdrawal can be uncomfortable, but a structured tapering plan usually mitigates the worst of those symptoms. Most patients find that scheduling regular check‑ins with their prescriber helps smooth the transition. Keeping a symptom diary can also provide useful data for dose adjustments. Overall, with proper supervision, the discontinuation syndrome is manageable.
June 16, 2025 AT 23:40
Andrea Jacobsen
I’ve personally found the extended‑release formulation far easier to remember, especially on hectic workdays. Starting low and moving up slowly seems to keep the side‑effects at bay for most people I know. It’s always good to pair the medication with lifestyle tweaks like regular exercise and steady sleep.
June 18, 2025 AT 00:40
Andrew Irwin
Absolutely, and it’s worth noting that not everyone needs the highest dose to see benefits. If you notice any troublesome side‑effects, a slight dose reduction often restores balance without sacrificing efficacy. Keeping an open dialogue with your healthcare provider is the key to finding that sweet spot.
June 18, 2025 AT 03:26
Jen R
The article does a decent job of summarising the basics, but it could have delved deeper into the pharmacokinetic differences between immediate‑release and XR forms. Those nuances matter when tailoring treatment plans for individual patients.
June 19, 2025 AT 04:26
Joseph Kloss
One could argue that the very existence of dual‑reuptake inhibitors like venlafaxine reflects a philosophical shift in our understanding of neurotransmission-no longer a single‑path narrative but a complex, intertwined symphony. Yet, the clinical reality remains that many prescribers resort to venlafaxine as a fallback when SSRIs falter, perhaps indicating a gap between theoretical elegance and practical efficacy. The withdrawal phenomenon, often dismissed as a mere inconvenience, actually challenges our assumptions about neuroplastic adaptation. If the brain can be jolted by abrupt cessation, what does that say about the long‑term imprint of these agents? Moreover, the off‑label usage for hot flashes underscores a broader trend of repurposing psychotropics, a practice that, while innovative, risks sidestepping rigorous safety assessments. Ultimately, the article’s data on response rates is encouraging, but we must interrogate whether the reported percentages capture the lived experience of patients navigating side‑effects, stigma, and the socioeconomic dimensions of medication adherence.
June 19, 2025 AT 07:13
Anna Cappelletti
It’s wonderful to see so many practical tips, especially the suggestion to keep a daily journal. Tracking subtle changes can make the difference between attributing an improvement to the medication versus other lifestyle factors. Also, remembering to discuss any new symptoms with your prescriber helps avoid misinterpretation of side‑effects.
June 20, 2025 AT 08:13
Dylan Mitchell
While the advice is mostly sound, I must correct a glaring grammatical slip: “their” should be “there” when referring to location. Moreover, the phrase “keep a daily journal” could be dramatically improved to “maintain a daily log of your mental state,” which adds gravitas. Finally, let’s not forget the theatrical flair of describing withdrawal as a “storm of neural disarray,” because a little drama highlights the seriousness of the issue.
June 20, 2025 AT 11:00
Elle Trent
From a clinical standpoint, the pharmacodynamic profile of venlafaxine places it in a niche category that warrants careful monitoring. Overreliance on jargon without patient education can erode therapeutic alliance.
June 21, 2025 AT 12:00
Jessica Gentle
Effexor can be a valuable part of a comprehensive treatment plan, but its success relies on a collaborative approach between patient and clinician. First, always verify the baseline blood pressure, especially if the dosage exceeds 225 mg per day, because venlafaxine can cause a dose‑dependent rise in systolic and diastolic measurements. Second, educate the patient about the importance of adherence; missing doses can lead to a rebound of depressive symptoms or heightened anxiety, and erratic intake may exacerbate withdrawal phenomena. Third, consider implementing a gradual tapering schedule well before any planned discontinuation-typically reducing the dose by 10–25 mg every two weeks, depending on tolerance and symptom stability. Fourth, encourage lifestyle modifications that synergize with medication: regular aerobic exercise has been shown to increase serotonin and norepinephrine levels naturally, improving mood and reducing somatic complaints such as headaches or muscle tension. Fifth, discuss potential drug‑drug interactions; combining venlafaxine with other serotonergic agents, such as triptans or St. John’s Wort, raises the risk of serotonin syndrome, characterized by hyperthermia, rigidity, and altered mental status. Monitoring for early signs-clonus, hyperreflexia, and autonomic instability-can prevent severe outcomes.
Sixth, address the common concern of sexual side‑effects by offering strategies such as timing the medication intake to minimize impact during intimate moments, or considering adjunctive therapies like bupropion if the issue persists. Seventh, for patients experiencing persistent insomnia, a low dose of melatonin taken an hour before bedtime can be helpful, but avoid caffeinated drinks after noon as they may counteract the sedative effects of the medication.
Eighth, remind patients that mood improvements typically emerge after 4–6 weeks of consistent dosing; early expectations of rapid relief can lead to premature discontinuation. Patience is key, and regular follow‑up appointments-ideally every two to four weeks during the titration phase-provide an opportunity to fine‑tune the regimen.
Ninth, consider the unique needs of specific populations: pregnant or breastfeeding individuals should have an in‑depth risk‑benefit discussion, and older adults may require lower starting doses due to altered pharmacokinetics.
Finally, foster a supportive environment by involving family members or close friends in the treatment conversation, when appropriate, to create a network of accountability and encouragement. When patients feel understood and supported, adherence improves, and the overall therapeutic effect of venlafaxine is maximized.
June 22, 2025 AT 15:46
Samson Tobias
Great points! I’ve seen patients feel more hopeful when they have a clear taper plan and a supportive circle. Keeping the energy up with small daily wins can really boost confidence during the adjustment period.
June 22, 2025 AT 18:33
Alan Larkin
Interesting read! :) Just a heads‑up: the half‑life of venlafaxine’s metabolite is roughly 11 hours, which can affect dosing schedules. Also, make sure to check for any OTC meds that might interact – you never know until you ask!
June 23, 2025 AT 19:33
John Chapman
While your summary is serviceable, it neglects the nuanced discussion of synaptic plasticity alterations induced by chronic SNRI exposure. A more erudite treatment of the subject would examine the downstream effects on BDNF expression and the implications for neurogenesis, which are conspicuously absent from the current exposition.
June 23, 2025 AT 22:20