EHR Integration for Pharmacies: How Digital Communication Improves Prescription Safety and Care

- Colin Hurd
- 22 December 2025
- 11 Comments
Imagine this: a patient walks into your pharmacy with a new prescription for warfarin. You check their profile and see they’re also taking amiodarone and have a recent INR of 5.2. Without access to their full medical record, you might just fill the script and move on. But with EHR integration, you see the lab result, the drug interaction warning, and the note from their cardiologist that they’re scheduled for a procedure next week. You call the prescriber. The dose is adjusted. A hospitalization is avoided. That’s not hypothetical-it’s happening in clinics and pharmacies that have made the leap to integrated systems.
Why EHR Integration Matters More Than Ever
For decades, pharmacies and doctors operated in silos. Prescriptions flew through fax machines, paper scripts got lost, and medication histories were pieced together from memory or incomplete printouts. That’s not just inefficient-it’s dangerous. A 2020 study from the University of Wisconsin found that community pharmacists, despite being the most accessible healthcare providers, had almost no access to patient records. They were left guessing what else a patient was taking, what allergies they had, or whether a new drug clashed with their existing regimen. EHR integration changes that. It connects the pharmacy’s system directly to the provider’s electronic health record. This isn’t just about sending a prescription electronically. It’s about two-way communication: doctors see what medications the patient actually picked up, pharmacists see lab results, diagnosis codes, and care plans. The result? Fewer errors, better outcomes, and less waste.How It Actually Works: Standards Behind the Scenes
You won’t see the gears turning, but behind every successful EHR-pharmacy connection are two key standards:- NCPDP SCRIPT 2017071 handles the actual prescription transmission. It’s the digital version of the paper script, but with built-in checks for dosage, allergies, and drug interactions.
- HL7 FHIR Release 4 is the language that lets pharmacists pull in broader clinical data-lab results, diagnoses, past hospitalizations, even care plans written by the patient’s primary doctor.
The Real Benefits: Numbers That Speak Louder Than Promises
It’s easy to talk about "improved care." But here’s what integration actually delivers:- 48% fewer medication errors thanks to automated alerts for interactions, duplications, or inappropriate dosing.
- 63% faster prescription processing-down from 15.2 minutes to 5.6 minutes per script. That’s time saved for pharmacists and patients alike.
- 31% reduction in medication-related hospital readmissions, as shown in a 2021-2022 pilot in East Tennessee that connected 12 independent pharmacies with three clinics.
- 4.2 medication-related problems identified per patient encounter when pharmacists have full EHR access-compared to just 1.7 without it.
- $1,250 annual savings per patient through better medication management and fewer avoidable ER visits.
Who’s Doing It Right-and Who’s Still Struggling
There’s a huge divide between big health systems and independent pharmacies. In hospitals and integrated networks, 89% of pharmacies have EHR access. In independent community pharmacies? Only 12% do. Why? Cost. Implementation for a small pharmacy can run $15,000 to $50,000 upfront, plus $5,000-$15,000 a year to maintain. For a shop making $300,000 in annual revenue, that’s a massive investment. And it’s not just about the software-it’s training, workflow changes, and dealing with IT headaches. Then there’s reimbursement. Only 19 states in the U.S. pay pharmacists for the time they spend reviewing EHR data and coordinating care. In Australia, Medicare doesn’t yet reimburse for pharmacist-led medication reviews conducted through digital systems. Without payment, integration becomes a charity project-not a sustainable service.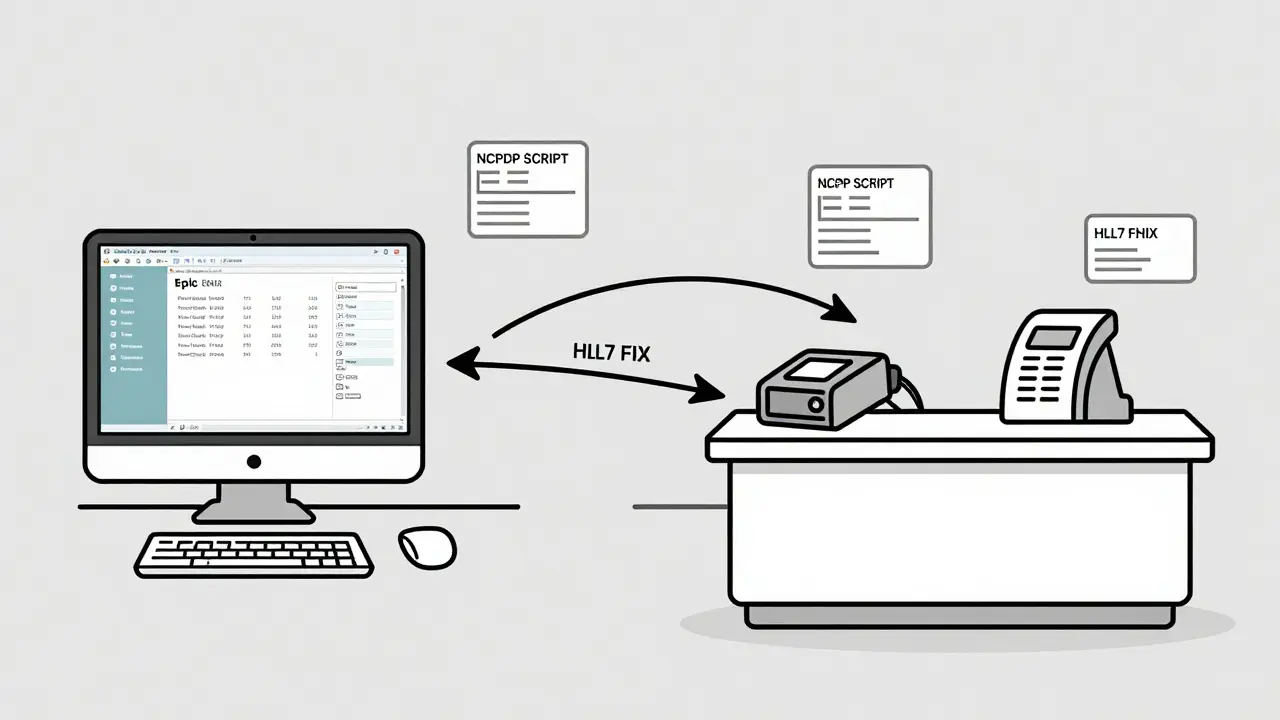
Top Solutions on the Market
If you’re looking to integrate, here are the main players:- Surescripts: Processes over 22 billion transactions annually. Offers Medication History, Eligibility Checks, and Electronic Prior Authorization. Used by 97% of U.S. pharmacies. Costs $0.03-$0.05 per transaction.
- SmartClinix: Pharmacy-specific EMR with EHR integration starting at $199/month. Popular for its seamless connection with Epic and Cerner systems.
- DocStation: Focuses on provider network management and billing integration. Starts at $249/month.
- UpToDate: Not a pharmacy system, but integrates with 40+ EHRs to deliver evidence-based drug info directly into clinician workflows.
Barriers That Keep Integration Rare
Even when pharmacies want to integrate, they hit walls:- 120+ EHR systems and 50+ pharmacy software platforms mean data doesn’t always match up. A lab result in Epic might be labeled differently in a smaller system.
- Time crunch: Pharmacists spend an average of 2.1 minutes per patient. Even with alerts, there’s no time to dig into complex EHR data without workflow redesign.
- Alert fatigue: Too many warnings-many irrelevant-lead to staff ignoring them. One pharmacist on Reddit said they get 40 alerts per shift, and 35 are "just noise."
- Lack of training: Most pharmacy schools don’t teach EHR integration. Pharmacists learn on the job, often from poorly documented vendor guides.
What’s Next: AI, Patients, and Policy
The future isn’t just about connecting systems-it’s about making them smarter.- AI-powered alerts: CVS and Walgreens are testing machine learning models that scan integrated EHR-pharmacy data to flag high-risk patients before they even walk in. Early results show 37% more accurate intervention targeting.
- Patient-mediated data: The CARIN Blue Button 2.0 system (launched Jan 2024) lets patients download their medication history from their insurer and send it directly to their pharmacy. This bypasses provider delays.
- New standards: NCPDP’s Pharmacist eCare Plan (PeCP) Version 2.0, due in late 2024, will let pharmacists send structured care summaries back to providers-like a mini-discharge note.
- Policy pressure: Medicare Part D Star Ratings now require integrated communication for top scores. California’s SB 1115 mandates EHR integration for medication therapy management by 2026.

How to Get Started
If you’re a pharmacy owner or manager thinking about integration, here’s your roadmap:- Assess readiness: Do you have a stable internet connection? Are your staff comfortable with digital tools? Budget $2,500-$5,000 for a readiness audit.
- Choose your path: Surescripts is the safest bet for most U.S. pharmacies. For Australian pharmacies, check if your system connects to My Health Record.
- Start small: Don’t try to integrate everything at once. Begin with electronic prescribing and medication history access.
- Train your team: Dedicate 2-3 weeks to hands-on training. Don’t assume they’ll figure it out.
- Measure results: Track how many medication errors you prevent, how much time you save per script, and how many patients report better understanding of their meds.
Frequently Asked Questions
What’s the difference between e-prescribing and EHR integration?
E-prescribing is one-way: the doctor sends a prescription to the pharmacy. EHR integration is two-way: the pharmacy can also send clinical data back to the doctor’s record-like medication adherence notes, side effects, or lab results. It’s not just sending a script; it’s sharing the full story behind it.
Can small independent pharmacies afford EHR integration?
It’s expensive-$15,000 to $50,000 upfront-but there are ways to reduce the burden. Some pharmacy chains offer group pricing. Surescripts has tiered pricing based on volume. Some states offer grants for rural pharmacies. And while the cost is high, the ROI is clear: one study showed $1,250 saved per patient per year through avoided hospitalizations and better medication management.
Why don’t all pharmacies use EHR integration if it’s so beneficial?
Three main reasons: cost, time, and reimbursement. Many independent pharmacies can’t afford the upfront investment. Pharmacists are already stretched thin-adding EHR reviews without extra time or pay isn’t sustainable. And without Medicare or insurance reimbursement for clinical services delivered through EHRs, there’s no financial incentive to make the change.
Is my patient data safe with EHR integration?
Yes, if done right. All systems must comply with HIPAA (in the U.S.) or the Privacy Act (in Australia). Data is encrypted with AES-256 when stored and sent over TLS 1.2 or higher. Audit logs track every access. The 21st Century Cures Act also bans "information blocking," meaning providers can’t refuse to share data without a valid reason.
How long does EHR integration take to implement?
Typically 3 to 6 months. The first 8-12 weeks are technical setup: connecting APIs, mapping data fields, testing. Then 4-8 weeks of staff training and workflow adjustments. Many pharmacies underestimate the time needed for staff to adapt. Rushing leads to errors and resistance.
What’s the biggest mistake pharmacies make when integrating?
Trying to do everything at once. Start with the basics: electronic prescribing and medication history access. Don’t jump into full clinical decision support until your team is comfortable. Also, don’t skip training. Pharmacists who don’t understand how to interpret EHR data won’t use it-even if it’s there.



Comments
Andrea Di Candia
This is the kind of stuff that actually saves lives, not just boosts profits. I’ve seen pharmacists catch drug interactions that doctors missed because they were rushing between patients. It’s not just tech-it’s care made visible. We treat pharmacies like order desks, but they’re frontline clinical hubs. If we want real healthcare reform, we start here.
December 23, 2025 AT 21:46
Dan Gaytan
YES. 🙌 My grandma almost got doubled up on blood thinners last year because the pharmacy didn’t know she was on warfarin. They only saw the new script. If this system had been in place? She’d still be walking. Thank you for writing this. We need more stories like this.
December 24, 2025 AT 08:49
Raja P
Love the stats. But here’s the real issue: most Indian pharmacies don’t even have stable internet, let alone EHR access. This feels like a US-centric solution. We need low-bandwidth, offline-first tools before we talk about FHIR and NCPDP. Tech shouldn’t exclude the people who need it most.
December 26, 2025 AT 02:38
Bret Freeman
Oh here we go again. Another tech bro pretending digital magic will fix broken healthcare. You think a pharmacist staring at 40 alerts a shift is gonna save lives? No. They’re gonna quit. The system is broken because we treat people like data points, not humans. And now you want to dump more screens on them? Brilliant.
December 27, 2025 AT 20:41
Lindsey Kidd
So proud of the progress! 🌟 I work with rural pharmacies and we just got Surescripts set up last month. Took 5 months, 3 training sessions, and a lot of coffee, but last week we caught a dangerous combo with a patient on lithium and an NSAID. They didn’t even know it was risky. That’s why we do this. You’re not just filling scripts-you’re holding the line.
December 29, 2025 AT 07:06
Austin LeBlanc
Why are we still talking about this like it’s a breakthrough? This is basic. If you’re a pharmacy and you’re not integrated, you’re not just behind-you’re negligent. It’s 2025. We have apps that track our coffee intake. But we’re still flying blind on life-saving meds? Unacceptable. Someone needs to lose their license over this.
December 30, 2025 AT 12:09
niharika hardikar
While the clinical utility of EHR-pharmacy interoperability is empirically validated, the implementation architecture remains fraught with semantic heterogeneity across disparate HL7 FHIR profiles and NCPDP SCRIPT variants. The absence of standardized ontological mappings engenders data integrity failures, thereby undermining the very safety objectives the integration purports to achieve.
December 31, 2025 AT 02:28
Bartholomew Henry Allen
USA leads the world in healthcare innovation. No other country has the infrastructure or discipline to make this work. If you can’t afford it, get a better job. This isn’t a privilege. It’s a requirement. We don’t do half measures here.
January 1, 2026 AT 16:05
Abby Polhill
Interesting how the article never mentions that 70% of these alerts are false positives. I’ve had pharmacists roll their eyes at the system. It’s like having a smoke alarm that goes off every time you toast bread. Tech’s great-but not if it’s noise with a side of burnout.
January 2, 2026 AT 06:16
Jillian Angus
My local pharmacy just started using Surescripts last year. Took them six months to get it right. But now they call me if my meds don’t line up with my doctor’s notes. I didn’t even know they could do that. Feels nice to be seen.
January 2, 2026 AT 09:41
Sidra Khan
Yeah sure, 48% fewer errors. But how many pharmacists got fired because they ‘ignored’ too many alerts? This whole thing feels like a corporate profit play dressed up as patient care. They’re not trying to save lives-they’re trying to bill Medicare for ‘clinical services’ they didn’t earn.
January 4, 2026 AT 02:06