FDA Safety Standards: How Generic Drugs Meet Brand Name Drug Requirements

- Colin Hurd
- 12 January 2026
- 13 Comments
When you pick up a prescription, you might see two options: the name-brand pill you’ve heard of, or a cheaper generic version. You might wonder-are generic drugs really as safe as the brand name ones? The answer isn’t just yes, it’s backed by some of the strictest science and oversight in modern medicine.
Same Active Ingredient, Same Results
Every generic drug must contain the exact same active ingredient as its brand-name counterpart. That means if you’re taking metformin for diabetes, whether it’s sold as Glucophage or a generic version, the molecule doing the work inside your body is identical. The FDA doesn’t allow any variation here. This isn’t a suggestion-it’s a legal requirement under 21 CFR 314.94(a). No exceptions.It’s not just the ingredient. The strength, dosage form (tablet, capsule, liquid), and how it’s taken (by mouth, injection, etc.) must match too. If the brand is a 500mg tablet taken twice daily, the generic must be the same. No more, no less.
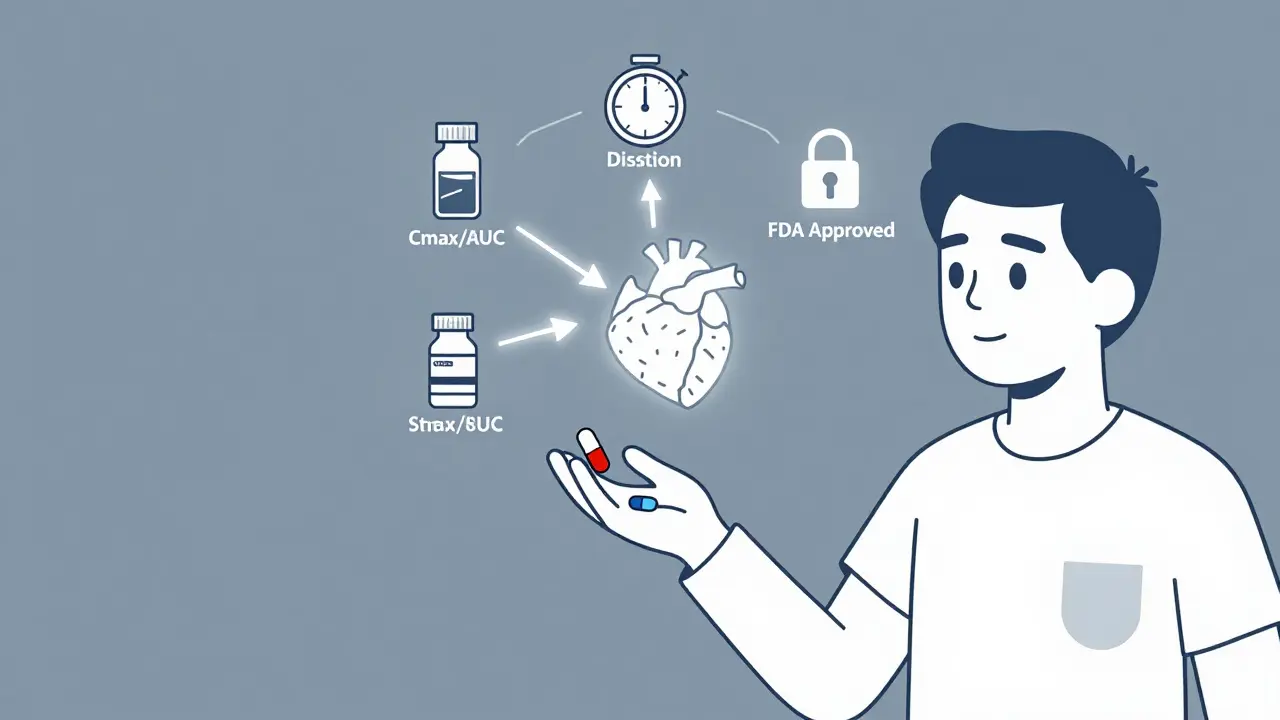
Bioequivalence: The Real Test
Here’s where most people get confused. If the ingredients are the same, why do we need more testing? Because how your body absorbs the drug matters just as much as what’s in it.The FDA requires generics to prove they’re bioequivalent to the brand drug. That means the generic must deliver the same amount of medicine into your bloodstream at the same rate. To prove this, manufacturers run studies with healthy volunteers-usually 24 to 36 people. Blood samples are taken over hours to measure two key things: Cmax (how high the drug peaks in your blood) and AUC (how much total drug your body absorbs over time).
The FDA’s rule? The 90% confidence interval for both Cmax and AUC must fall between 80% and 125% of the brand drug’s numbers. That’s not a guess-it’s a hard scientific standard. If a generic falls outside that range, it’s rejected. For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or lithium-the bar is even higher: 90% to 111%. These are drugs where even a small difference can cause serious side effects or make treatment fail.
Manufacturing: No Cutting Corners
A lot of people think generics are made in cheap, sketchy factories. That’s not true. Every generic drug, no matter where it’s made, must follow Current Good Manufacturing Practices (cGMP). That means:- Every step of production is documented and audited
- Equipment is cleaned, calibrated, and maintained to exact specs
- Raw materials are tested before use
- Final products are tested for purity, potency, and stability
The FDA inspects over 3,500 manufacturing sites worldwide each year-half of them outside the U.S. In 2022, they found a 22% increase in inspections of overseas facilities thanks to their Risk-Based Facility Assessment program. If a factory fails inspection, the FDA can block the drug from entering the U.S. market.
Impurities and Safety Limits
Even tiny amounts of impurities can be dangerous. That’s why the FDA follows international guidelines like ICH Q3B and ICH M7 to set strict limits. For example, any potential carcinogen or genotoxic impurity must not exceed 1.5 micrograms per day-a level so low it’s considered safe even with lifelong exposure.Generic manufacturers must test for these impurities and prove they’re within limits. The FDA doesn’t just accept their word-they run independent tests on samples pulled from the market. In 2021, the FDA’s internal review found that 15% of generic drugs flagged for safety concerns were linked to narrow therapeutic index medications. That’s why the agency now issues product-specific guidances for tricky drugs like antiepileptics and blood thinners.

Dissolution and Stability: Does It Work the Same?
A pill might have the right ingredients and absorb properly-but if it doesn’t dissolve at the right speed, it won’t work right. That’s why dissolution testing is required. The generic must dissolve in the same way as the brand drug, using the same method and conditions. If a manufacturer wants to use a different method, they need to prove it’s scientifically justified.Stability testing is just as strict. Generics must show they remain effective and safe for their entire shelf life-usually 12 to 24 months. That means storing samples under heat, humidity, and light to simulate real-world conditions. If the drug breaks down too fast, it’s rejected.
Labeling: Same Information, Different Packaging
The FDA requires generic drug labels to be “the same as” the brand’s, except for a few allowed differences:- Manufacturer, packer, or distributor name
- Package size
- Inactive ingredients (like dyes, fillers, or flavorings)
- Shape, color, or scoring on the pill
That’s why your generic metformin might be a different color than the brand version. But the warnings, dosage instructions, side effects, and contraindications? Identical. The FDA won’t allow a generic to have weaker safety info.
Complex Drugs: The Harder Cases
Not all drugs are created equal. Simple tablets? Easy to copy. Inhalers, eye drops, creams, or injectables with complex delivery systems? Much harder.The FDA reports a 25% higher rejection rate for ANDAs (Abbreviated New Drug Applications) on complex generics. Why? Because you can’t just measure blood levels-you need to prove the drug reaches the right place in the body the same way. For an inhaler, that means matching particle size, spray pattern, and lung deposition. For a topical cream, it’s about how the drug penetrates the skin.
Some complex drugs, like glatiramer acetate (Copaxone), triggered debate because they’re made from biological materials. In 2013, Teva petitioned the FDA to require immunogenicity testing for generics-something not normally needed. The FDA agreed it was a gray area and has since developed new testing methods for these tricky products.
What the Data Says
Let’s cut through the noise with real numbers:- 90% of all prescriptions filled in the U.S. are generics-but they cost only 23% of total drug spending (CMS, 2022)
- 87% of patients on Drugs.com reported no difference in effectiveness between brand and generic cardiovascular drugs (2020-2023)
- A 2022 JAMA Internal Medicine study of 38,000 Medicare patients found no difference in outcomes between brand and generic statins
- 68% of neurologists feel confident in generic antiepileptics, but only 42% feel the same about complex MS drugs
There are exceptions. Some patients report feeling different on generic levothyroxine-even though bioequivalence studies show they’re within the 90-111% range. Why? Possibly because of tiny differences in inactive ingredients affecting absorption in sensitive individuals. That’s why the FDA now recommends patients stick with one manufacturer if they’re on thyroid medication.
What’s Changing Now
The FDA is updating its rules to keep up with science:- In 2022, they proposed a rule letting generic makers update safety labels without waiting for the brand company-ending a 40-year-old restriction
- The FDA is investing $15 million to use AI and modeling to predict how complex drugs behave in the body
- They’ve allocated $50 million through GDUFA III (2023-2027) to improve testing for complex generics
- Over 1,800 product-specific guidances are now available to help manufacturers get it right the first time
The goal? Keep generics affordable without compromising safety. The system works-98% of U.S. hospitals use generics as first-line treatment. But for complex drugs, the science is still catching up.
Bottom Line: Safe, Effective, and Heavily Regulated
Generic drugs aren’t second-rate. They’re held to the same exacting standards as brand-name drugs-sometimes even stricter, especially for high-risk medications. The FDA doesn’t just approve them. They monitor them, inspect them, test them, and update the rules when needed.If you’re worried about switching to a generic, talk to your pharmacist or doctor. For most people, the switch is seamless. For those on narrow therapeutic index drugs, consistency matters-stick with the same generic brand if you notice any changes.
The system isn’t perfect. But it’s one of the most transparent, science-driven drug approval systems in the world. And it’s why you can trust your generic meds to work-just like the brand.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict safety and efficacy standards as brand-name drugs. They must contain the same active ingredient, strength, dosage form, and route of administration. They must also prove bioequivalence, meaning they deliver the same amount of medicine into your bloodstream at the same rate. Manufacturing follows Current Good Manufacturing Practices (cGMP), and impurity levels are strictly controlled.
Why do generic drugs look different from brand-name ones?
Generic drugs can differ in color, shape, size, or flavor because those are inactive ingredients or design choices. The FDA allows these differences as long as the active ingredient and how the drug works in the body are identical. These changes don’t affect safety or effectiveness.
Can I trust generics made overseas?
Yes. The FDA inspects all manufacturing facilities-whether in the U.S., India, China, or elsewhere-with the same standards. In 2022, they increased overseas inspections by 22%. If a facility fails inspection, the FDA blocks its products from entering the U.S. market. All drugs sold in the U.S. must meet the same quality rules, no matter where they’re made.
Are there any generics that aren’t as effective?
For most drugs, no. But for complex products-like inhalers, injectables, or topical creams-proving equivalence is harder. The FDA has a higher rejection rate for these. Also, for narrow therapeutic index drugs (like levothyroxine or warfarin), some patients report differences, possibly due to inactive ingredients. In these cases, staying with the same generic manufacturer is recommended.
How long does it take for a generic to get FDA approval?
The process typically takes 18 to 36 months from development to approval. The FDA’s median review time for a first-cycle ANDA application is about 10 months. Complex generics can take longer due to additional testing requirements. The Generic Drug User Fee Amendments (GDUFA) have cut approval times by 35% since 2012.
Do generics cost less because they’re lower quality?
No. Generics cost less because they don’t need to repeat expensive clinical trials. The brand-name company already proved safety and effectiveness. Generic manufacturers only need to prove bioequivalence and follow the same manufacturing rules. This saves money without cutting corners on safety or quality.
Can I switch between different generic brands?
For most drugs, yes. But for narrow therapeutic index medications like levothyroxine, warfarin, or phenytoin, it’s best to stick with one manufacturer. Even small differences in inactive ingredients can affect absorption in sensitive individuals. If you notice a change in how you feel after switching, talk to your doctor or pharmacist.



Comments
Angel Molano
Generic drugs are held to the same standards-end of story. If you’re still skeptical, you’re either misinformed or profit-driven.
January 12, 2026 AT 18:10
Kimberly Mitchell
The bioequivalence thresholds are arbitrary. 80-125%? That’s a 45% swing. For a drug like warfarin, that’s not science-it’s gambling with patient lives.
January 12, 2026 AT 19:38
Vinaypriy Wane
I’ve seen patients on levothyroxine switch generics and crash into hypothyroidism-yes, even within the 90–111% range. The inactive ingredients? They matter. A lot. Especially for people with autoimmune thyroiditis. The FDA knows this. Why aren’t they forcing batch consistency?
January 13, 2026 AT 21:33
laura Drever
lol generics are fine until you get the one with the weird filler that makes you feel like you swallowed sand
January 15, 2026 AT 08:54
Diana Campos Ortiz
My grandma’s on levothyroxine. She switched generics once and started zoning out. We went back to the original-and boom, she was herself again. I get the cost thing, but some people aren’t lab rats.
January 17, 2026 AT 02:18
Robin Williams
Look, we’re all just carbon-based lifeforms trying to survive on a rock hurtling through space. But if we can trust a pill made in a factory in Chennai to keep our hearts beating like the one made in New Jersey? That’s the kind of miracle capitalism forgot to charge us for.
January 18, 2026 AT 02:31
Scottie Baker
Ugh, I hate when people act like generics are some kind of miracle. I had a generic statin that gave me muscle pain so bad I could barely walk. Switched back to brand-poof. Gone. So yeah, sometimes they’re not the same. And no, I’m not paying extra for the placebo branding.
January 18, 2026 AT 11:27
Anny Kaettano
For complex generics-especially inhalers and topical formulations-the bioequivalence data is often extrapolated, not directly measured. The FDA’s guidelines assume linear pharmacokinetics, but skin and lungs don’t work like that. We need better models. And yes, we’re talking about real patients here, not just regulatory checkboxes.
January 19, 2026 AT 04:06
Jesse Ibarra
Let me get this straight-some guy in a lab coat in India makes a pill that’s ‘close enough’ to my heart medication, and you want me to trust it? Meanwhile, the FDA inspects 3,500 sites a year? That’s like checking 3,500 cars for brake pads… once… and hoping none of them explode. This isn’t regulation. It’s a prayer.
January 19, 2026 AT 07:48
Randall Little
Interesting that the FDA allows generics to change their labels only after the brand does. That’s like letting a knockoff watch update its time only after Rolex does. Meanwhile, the real innovation? AI modeling to predict drug behavior. That’s the future. Not just matching blood curves.
January 19, 2026 AT 15:57
Rosalee Vanness
Let’s be real-switching generics isn’t just about chemistry. It’s about psychology. If you’ve been on the same brand for years, your brain associates that blue pill with feeling okay. Change the color? Suddenly, your body starts doubting. It’s not placebo-it’s embodied expectation. And for people with chronic conditions, that mental anchor matters more than we admit. So yeah, if your thyroid meds make you feel stable? Don’t mess with it. Your peace of mind is part of the treatment.
January 20, 2026 AT 20:45
Trevor Davis
As a pharmacist, I’ve seen it all. Some patients swear their generic gives them headaches. Others say the brand makes them nauseous. Nine times out of ten, it’s the fillers. Corn starch vs. lactose. Dyes. Even the coating. The active ingredient? Identical. But our bodies? They’re weird. And we’re not all built the same. So yeah-stick with one manufacturer. It’s not paranoia. It’s personal pharmacology.
January 21, 2026 AT 21:33
Pankaj Singh
98% of hospitals use generics? That’s because they’re forced to by cost-cutting administrators, not because they’re safer. The FDA’s data is cherry-picked. What about the 15% of flagged generics tied to narrow therapeutic index drugs? That’s not a footnote-that’s a red flag waving in a hurricane. And don’t get me started on the fact that 70% of generic manufacturers are owned by the same Big Pharma companies that make the brand names. This isn’t competition. It’s a shell game.
January 23, 2026 AT 16:11