Food Allergies: How IgE Reactions Cause Anaphylaxis and How to Prevent Them

- Colin Hurd
- 26 December 2025
- 14 Comments
What Exactly Is an IgE Food Allergy?
When your body mistakes a harmless food protein for a dangerous invader, it sends out IgE antibodies to fight it. This isn’t just a mild reaction-it’s a full-scale immune alert that can turn deadly in minutes. Unlike digestive issues that show up hours later, IgE-mediated food allergies hit fast: hives, swelling, wheezing, vomiting, or a sudden drop in blood pressure. These symptoms aren’t random. They’re the result of mast cells and basophils dumping histamine and other chemicals into your bloodstream the moment the allergen reappears.
It’s not just about eating the food. For some kids, a peanut crumb on a toy or skin contact through eczema can start the process. That’s why babies with severe eczema are at higher risk-their broken skin barrier lets allergens in the wrong way. Research shows up to 40% of peanut allergies begin this way, not from eating.
Why Food Allergies Are More Common Now
Thirty years ago, food allergies were rare. Today, about 8% of kids and 5% of adults in places like the U.S., Australia, and Europe have them. The numbers jumped 50% between 1997 and 2011. Why? Scientists don’t have one answer, but the clues point to modern life.
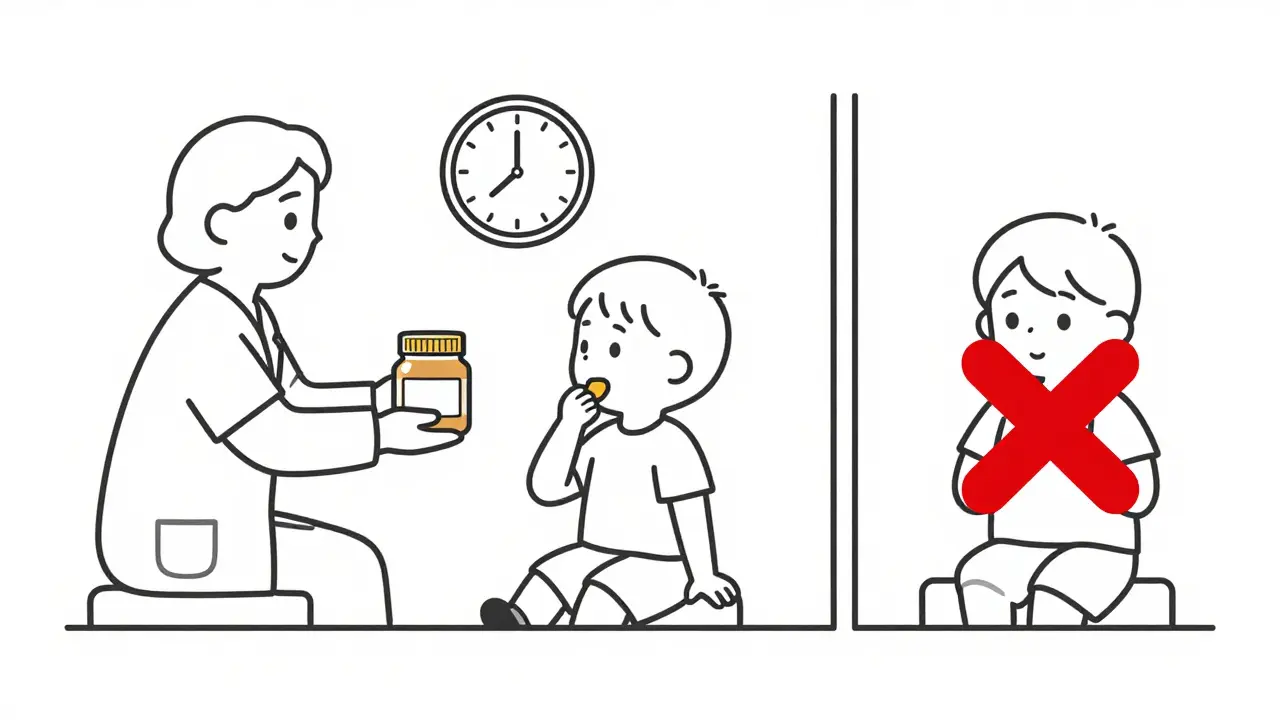
One big theory is the dual-allergen-exposure hypothesis. If your baby’s skin is cracked from eczema and they’re exposed to peanut dust in the air or on surfaces, their immune system learns to see peanut as a threat. But if they eat peanut early and safely, their gut teaches their immune system to ignore it. That’s why guidelines now say: don’t wait. Introduce peanut-containing foods between 4 and 6 months for high-risk babies, even if they have eczema or egg allergy.
Studies like LEAP proved this works. Babies who ate peanut regularly from 4 months had an 81% lower chance of developing peanut allergy by age 5. That’s not a small win-it’s a game-changer.
The Top Triggers by Age
Not all food allergies are the same. What triggers a reaction in a toddler isn’t always the same as what triggers one in an adult.
- Children under 3: Milk (2.5%), egg (1.9%), and peanut (2.2%) are the top three. Many outgrow milk and egg allergies by age 16.
- Adults: Shellfish (2.9%) and tree nuts (1.8%) dominate. These allergies rarely go away.
Even within these, the protein matters. For egg, if your child’s IgE binds to Gal d 1 (a heat-labile protein), they’re more likely to outgrow it. If it’s Gal d 2 (heat-stable), the allergy is more likely to stick. This isn’t just academic-it guides whether you try baked egg in cookies or avoid it entirely.
How Doctors Diagnose Food Allergies
Guessing isn’t enough. A history of reactions plus testing is the baseline.
Skin prick tests show a wheal-if it’s 3mm bigger than the control, it’s positive. But a positive test doesn’t always mean a real allergy. For peanut, you need a wheal of at least 8mm to be 50% sure it’s a true reaction. For egg, it’s 7mm.
Blood tests measure IgE levels in kU/L. A peanut IgE level of 14 kU/L means a 95% chance of a clinical reaction. But even these can be misleading. That’s why component-resolved diagnostics are becoming standard. Testing for Ara h 2 (a peanut protein) gives a much clearer picture. If Ara h 2 IgE is above 0.35 kU/L, there’s a 95% chance the person will react to even small amounts.
The gold standard? The oral food challenge. You eat increasing amounts of the food under medical supervision. About 14-17% of these challenges lead to reactions needing epinephrine. That’s why they’re done in clinics, not at home.
Prevention Starts Before Birth
It’s not just about what you feed your baby-it’s what you did before they were born.
Mothers with higher vitamin D levels during pregnancy (above 75 nmol/L) have babies with a 30% lower chance of food sensitization. Vitamin D helps regulatory T cells-your body’s peacekeepers-that keep the immune system from overreacting.
Emollients matter too. The BEEP trial found that applying petroleum jelly daily from birth to high-risk babies cut food allergy rates by half. It’s simple: keep the skin barrier intact. No cracks, no allergens sneaking in.
And while probiotics were once thought to help, the Cochrane Review in 2020 found no solid proof they prevent food allergies. Don’t waste money on supplements that don’t work.
What to Do If Anaphylaxis Happens
Anaphylaxis doesn’t wait. Every minute counts.
Epinephrine is the only thing that stops it. Auto-injectors like EpiPen (0.3 mg for adults and kids over 30 kg) or Auvi-Q (0.15 mg for 15-30 kg) must be used within 5-15 minutes of the first sign of trouble. Delaying by more than 30 minutes makes a biphasic reaction-where symptoms return hours later-68% more likely. It also triples the chance of needing intensive care.
Here’s the hard truth: only half of people who are prescribed epinephrine carry it all the time. And 40% of those who do use it don’t use it right. They inject into the wrong spot. They hold it too short. They’re scared.
That’s why training isn’t optional. Practice on a trainer pen every month. Teach your child’s teachers, your partner, your babysitter. Make sure they know where the pen is and how to use it. New devices like Auvi-Q give voice instructions during use-boosting correct use from 60% to 92% in simulations.

Treatment Options After Diagnosis
Avoidance is the standard-but it’s not enough. Accidental exposures happen to 50-80% of kids with peanut allergy over five years. One in three of those reactions needs epinephrine.
Oral Immunotherapy (OIT) is now FDA-approved for peanut allergy in kids 4-17. Palforzia, the peanut powder, helps 67% of kids tolerate the equivalent of two peanuts without a reaction. It doesn’t cure the allergy, but it reduces the risk of a life-threatening reaction from a crumb.
Sublingual Immunotherapy (SLIT) puts a tiny amount of allergen under the tongue. It’s less effective than OIT but safer. About half of patients can handle 3-4 peanuts after two years.
Omalizumab (Xolair) is an anti-IgE drug used alongside OIT. It cuts reaction rates during dose increases by half and lets patients reach their target dose faster.
These aren’t magic cures. They require months of daily dosing, and reactions still happen. But for families living in fear, they offer a lifeline.
What the Future Holds
Research is moving fast. The PREPARE trial is testing whether giving pregnant mothers 4,400 IU of vitamin D daily reduces food allergies in kids by age 3. The EAT2 study is introducing six allergens (milk, egg, peanut, sesame, fish, wheat) at 3 months to see if early multi-allergen exposure works better than single-food introduction.
New therapies include TLR9 agonists (immune boosters) paired with allergen therapy-early trials show 80% desensitization rates. Nanoparticles that deliver peanut peptides without triggering IgE are in development. They could one day offer a cure without daily pills or injections.
But here’s the reality: even with perfect early introduction, 20% of peanut allergies still develop. Prevention isn’t perfect. That’s why we need better tools-not just for treatment, but for early detection and protection.
Final Thoughts: Prevention Is Possible, But It’s Not Simple
Food allergies aren’t just a childhood issue-they’re a lifelong challenge. But we now know how to stop many of them before they start. Early introduction of allergens, skin barrier care, and vitamin D support are proven tools. Epinephrine saves lives when reactions happen. And new therapies are making it safer to live with allergies than ever before.
Don’t wait for a reaction to act. If you have a family history of allergies, talk to your doctor before your baby turns 4 months. Ask about skin care, vitamin D, and when to introduce peanut. Carry epinephrine. Train everyone around you. Knowledge isn’t just power-it’s protection.




Comments
josue robert figueroa salazar
IgE is just your immune system having a panic attack over a peanut crumb. No wonder we're all so messed up.
December 28, 2025 AT 03:08
david jackson
I mean, think about it-our entire modern existence is basically a perfect storm for allergies. We sanitize everything, seal our kids in plastic, avoid sunlight, and then wonder why their bodies don't know what's real anymore. The skin barrier theory? It’s not just science-it’s a cry from our biology screaming, 'Stop treating me like a lab dish!' And don’t even get me started on how we’ve turned parenting into a high-stakes game of Russian roulette with allergens. We’re so afraid of one tiny reaction that we forget the body’s meant to learn, not just survive. It’s like raising a child in a bubble wrap prison and then being shocked they can’t handle the outside world. This isn’t just about food-it’s about how we’ve lost touch with nature, with dirt, with risk, with trust in our own biology.
December 28, 2025 AT 19:14
Jody Kennedy
This is LIFE-CHANGING info. If you have a baby with eczema-start peanut early. Start it NOW. Don’t wait. Your kid’s life could depend on it. I’m sharing this with every parent I know.
December 30, 2025 AT 07:04
christian ebongue
So we spent 30 years telling people to avoid peanuts… and then turned around and said ‘oops, that was the dumbest idea ever?’ lol. My bad.
December 30, 2025 AT 11:28
jesse chen
I just want to say-thank you. This is the most clear, compassionate, and accurate breakdown I’ve ever read. The part about Ara h 2? I had no idea. And the epinephrine stats? Terrifying. But also… motivating. We need to get better at this.
December 30, 2025 AT 21:14
Lori Anne Franklin
I didnt even know vitamin D had anything to do with this! I’m gonna start giving my lil one some sunshine and cod liver oil. 🌞
December 31, 2025 AT 15:53
Ryan Cheng
If you’re a parent reading this and thinking ‘I don’t know where to start’-you’re not alone. But you’re also not powerless. Talk to your pediatrician. Get a referral to an allergist. Practice with a trainer pen. Teach your daycare staff. Prevention isn’t perfect-but action is always better than fear.
January 2, 2026 AT 05:23
Angela Spagnolo
I… I didn’t realize skin care could prevent allergies? I’ve been using lotion on my son’s eczema since he was born… but I didn’t know it could literally save his life? I’m going to start using petroleum jelly every single day. Thank you.
January 3, 2026 AT 09:06
Sarah Holmes
This entire narrative is a dangerous oversimplification of a complex immunological phenomenon. You reduce decades of biological evolution to a series of parenting hacks, as if human health can be managed like a consumer product. The rise in allergies is not a failure of hygiene-it is a symptom of systemic environmental collapse, industrialized food, and the commodification of medicine. You offer solutions like 'use this ointment' and 'take this pill'-but you ignore the root: a society that has abandoned natural immunity in favor of profit-driven interventions.
January 4, 2026 AT 15:02
Jay Ara
In india we give peanut paste to babies from 6 months and no big deal. Maybe its the way we cook it? Or maybe its just how we live? Not sure but i think its more than just one thing.
January 6, 2026 AT 04:02
Michael Bond
OIT sounds scary but also kind of amazing. I’d do it in a heartbeat if my kid had it.
January 7, 2026 AT 13:32
Kuldipsinh Rathod
My cousin's kid got diagnosed at 2. We were scared to death. Now he eats peanut butter every day after OIT. It's not perfect but it's life-changing.
January 8, 2026 AT 20:20
SHAKTI BHARDWAJ
So you’re saying we should just feed our babies peanut butter like it’s cereal? What’s next? Injecting them with shellfish? This is just Big Pharma’s new money grab disguised as science.
January 9, 2026 AT 19:03
Matthew Ingersoll
This is the kind of post that makes you realize how much we’ve forgotten about our own bodies. We used to raise kids in dirt, eat raw milk, and let them play outside until dark. Now we sanitize everything-and then wonder why their immune systems go haywire. It’s not just about food. It’s about how we live.
January 10, 2026 AT 05:45