How to Reconcile Medications After Hospital Discharge to Avoid Dangerous Interactions

- Colin Hurd
- 31 December 2025
- 13 Comments
Leaving the hospital shouldn’t feel like stepping into a medication maze. You’ve got new prescriptions, old ones you thought you were done with, and maybe even a few you forgot you were taking. One wrong pill, one missed dose, or one hidden interaction-and you could be back in the ER. Medication reconciliation isn’t just paperwork. It’s the difference between going home to recover and winding up hospitalized again.
What Medication Reconciliation Actually Means
Medication reconciliation is the process of making sure your home meds match exactly what you’re supposed to take after leaving the hospital. It’s not just about writing down a list. It’s about comparing every pill, patch, or injection you were on before admission with what the hospital gave you, and then figuring out what stays, what gets dropped, and what changes.
The goal? Stop dangerous mistakes. Studies show that nearly half of all medication errors happen during hospital transitions, especially at discharge. The most common? Missing a drug you were taking at home, adding a new one that clashes with something else, or changing the dose without telling you. These aren’t small risks. The Agency for Healthcare Research and Quality found that proper reconciliation cuts adverse drug events by 30% to 50%. That’s hundreds of thousands of avoidable hospital visits every year.
The Real Problem: What Goes Wrong at Discharge
Most hospitals have a reconciliation process on paper. But in practice? It often falls apart. Here’s why:
- Patient self-reporting is unreliable. People forget. They don’t know the names of their meds. They mix up doses. Studies show that when patients list their own meds, 42% of the time, it’s wrong. That’s worse than flipping a coin.
- Discharge summaries aren’t always clear. Even when the hospital gets it right, the discharge instructions might say “continue warfarin” but don’t mention that your daily dose changed from 5mg to 3mg. Or they list a new blood pressure med but forget to take off the old one.
- Time is short. Nurses and pharmacists are stretched thin. The ideal time to do a full reconciliation? 15 to 20 minutes per patient. The average? Less than 8 minutes. That’s not enough to catch a hidden interaction between a new antibiotic and your cholesterol drug.
- Chronic meds get dropped. If you were taken off your heart failure med or diabetes pill during your hospital stay, it’s easy for it to just… not get restarted. Especially if you were in the ICU. One study found ICU patients were over twice as likely to have a chronic medication discontinued at discharge.
One real case from a Reddit user: a man had warfarin stopped before surgery. It wasn’t restarted at discharge. Two weeks later, he had a pulmonary embolism and was readmitted. That’s preventable.
How to Do It Right: A Step-by-Step Plan
You can’t rely on the hospital to get it perfect. But you can make sure you leave with the right information. Here’s what to do-before, during, and after discharge.
Before You Go: Prepare Your Home Med List
Don’t wait until discharge day to figure out what you take. Get your list ready ahead of time. Include:
- All prescription drugs (name, dose, frequency)
- All over-the-counter meds (ibuprofen, antacids, sleep aids)
- All vitamins and supplements (fish oil, magnesium, turmeric)
- All herbal products (st. john’s wort, ginkgo, echinacea)
- All patches, inhalers, eye drops, or injections
Use a phone app, a printed sheet, or even a photo of your pill organizer. Don’t just say “I take blood pressure medicine.” Name it. Write down 10mg lisinopril, once daily. Exact details matter.
During Your Stay: Ask for the Discharge Med List
Two days before discharge, ask your nurse or pharmacist: “Can I see the list of meds you plan to send me home with?” Don’t wait until you’re being wheeled out. Compare it to your own list. Ask:
- “Is this new med replacing one I was taking?”
- “Why was this one taken off?”
- “Is this dose different from what I was on before?”
- “Are any of these known to interact with my other meds?”
Be specific. If you take metformin and your doctor adds a new diuretic, ask if it affects your kidney function. If you’re on statins, ask about grapefruit juice. Don’t assume they’ll catch it.
At Discharge: Get It in Writing
Never leave without a printed, updated medication list. It should show:
- Medications you’re continuing
- Medications you’re starting
- Medications you’re stopping
- Changes in dose or frequency
- Clear instructions: “Take with food,” “Avoid alcohol,” “Check liver enzymes monthly”
Ask for a copy to give to your GP or pharmacist. If they don’t give you one, ask for it again. Say: “I need this to avoid a bad reaction. Can you please print it?”
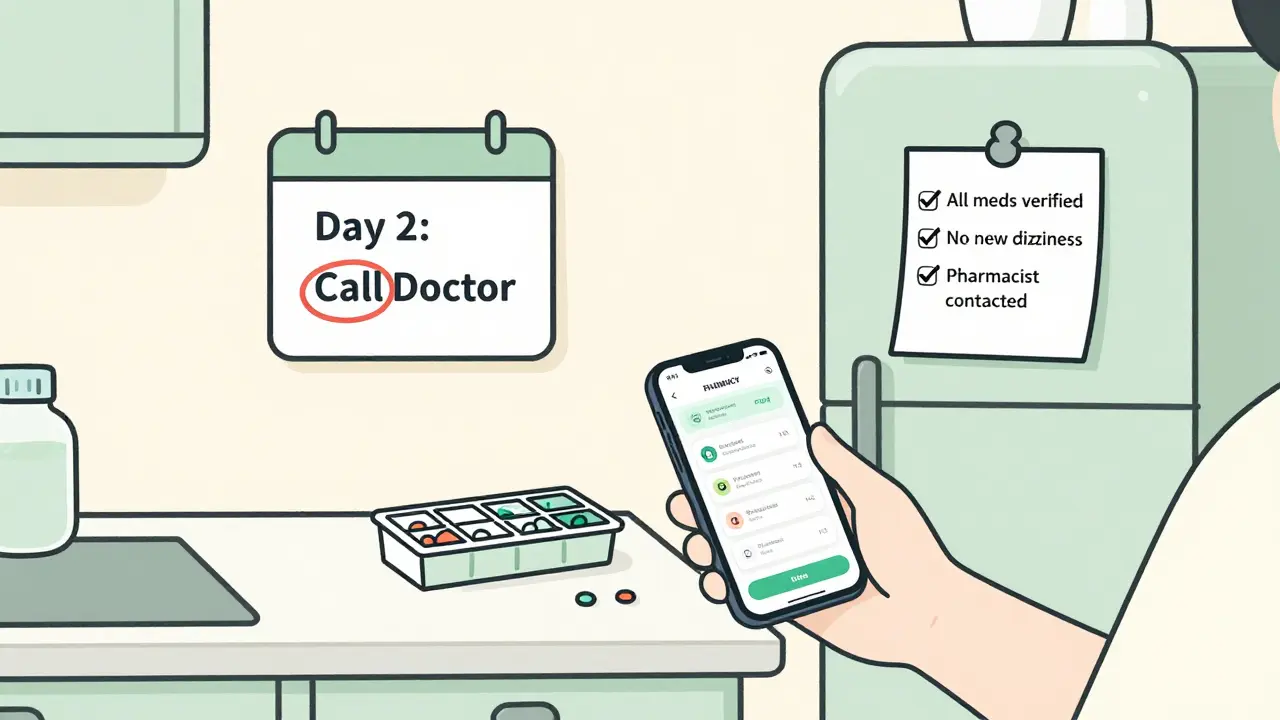
After Discharge: Verify Within 48 Hours
Call your pharmacist or GP within two days. Say: “I was just discharged. Here’s the list I got. Can you check it against my records?”
Pharmacists are trained to spot interactions. They’ll catch things doctors miss-like a new antibiotic clashing with your blood thinner, or a new painkiller adding to your risk of stomach bleeding if you’re on aspirin.
Also, check your pill bottles. Are the labels on the bottles matching the discharge list? If not, call the pharmacy. Don’t guess.
High-Risk Meds You Must Watch For
Some drugs are more dangerous when mixed. If you’re on any of these, double-check them at discharge:
- Warfarin (Coumadin) - Interacts with antibiotics, NSAIDs, and even some supplements like garlic or ginseng. A small change can cause bleeding or clots.
- Metformin - Can be stopped during hospital stays for kidney safety, but not restarted properly. Risk of high blood sugar.
- Statins - New meds like clarithromycin or grapefruit juice can spike levels and cause muscle damage.
- Antidepressants - SSRIs combined with certain pain meds can trigger serotonin syndrome.
- Diuretics - Can interact with NSAIDs, causing kidney stress or electrolyte imbalances.
Ask your pharmacist: “Which of these meds on my list could be dangerous together?” They’ll tell you.
What to Do If You’re Confused
If you don’t understand why a med was added or removed, don’t take it. Call someone. Here’s who to contact, in order:
- Your hospital’s discharge pharmacist (many have follow-up lines)
- Your primary care doctor
- Your community pharmacist
- Medicare’s 24/7 helpline (1-800-MEDICARE)
Don’t wait until you feel sick. If you’re dizzy, nauseous, or have unusual bruising, stop the new med and call your doctor immediately. It’s better to be safe than sorry.
Technology Can Help-But Not Replace You
Hospitals are starting to use AI tools to scan discharge summaries for missing meds. Some systems flag potential interactions automatically. Epic and Cerner now push discharge lists directly to outpatient EMRs.
But here’s the catch: technology doesn’t know if you stopped taking your fish oil last year. It doesn’t know you take melatonin for sleep. It doesn’t know you’re allergic to sulfa.
As one Harvard doctor put it: “Tech can find the gaps. But only you can fill them.”
Why This Matters Beyond the Hospital
Medication reconciliation isn’t just about avoiding a bad reaction. It’s about staying out of the hospital again. Studies show that patients who get proper reconciliation are 15% less likely to be readmitted within 30 days. That’s not just a number-it’s fewer ER visits, less stress, and more time at home.
And it’s not just about pills. It’s about control. When you understand your meds, you’re not just a patient-you’re an active part of your own care. That’s the real win.
Final Checklist: Before You Leave the Hospital
Use this before you sign out:
- ✅ I have a printed list of all meds I’m going home with
- ✅ It includes doses, frequency, and purpose for each
- ✅ I’ve compared it to my own list and asked about changes
- ✅ I know why any med was stopped or changed
- ✅ I’ve identified any high-risk meds and asked about interactions
- ✅ I have the name and number of someone to call if I’m unsure
- ✅ I’ve scheduled a pharmacy or doctor visit within 48 hours
If you can check all these boxes, you’ve done more than 80% of patients. And you’ve just made your next 30 days a lot safer.
What if I don’t remember all my meds before the hospital?
Don’t panic. Bring any pill bottles, prescription labels, or even photos of your medicine cabinet. Pharmacists can often identify pills by color, shape, and markings. If you have a pharmacy app or online portal, log in and print your history. Even a rough list helps-better than nothing.
Can I just rely on my doctor to fix this after discharge?
No. Your doctor may not see you for weeks. By then, you could have had a reaction, missed a dose, or taken something dangerous. Reconciliation needs to happen before you leave the hospital, and again within 48 hours after. Don’t wait.
Are herbal supplements really a problem?
Yes. St. John’s wort can make blood thinners and antidepressants ineffective. Garlic and ginkgo can increase bleeding risk with warfarin. Turmeric can interfere with blood sugar meds. Always list every supplement-even if you think it’s “natural” or “safe.”
What if the hospital won’t give me a printed list?
Insist. Say: “I need this to avoid a life-threatening interaction. It’s part of my care plan.” If they refuse, ask for the pharmacy department. If that fails, call your primary care provider and ask them to request it. You have a right to this information.
How do I know if a new med is causing a problem?
Watch for new symptoms: dizziness, confusion, nausea, unusual bruising, swelling, rash, or extreme fatigue. If you start a new med and feel worse within 2-3 days, stop it and call your doctor. Don’t wait. Write down what you took, when, and how you felt. That helps them diagnose it faster.




Comments
Paul Ong
Just got out of the hospital last month and this is exactly what I wish someone had told me before I walked out
January 2, 2026 AT 01:41
Richard Thomas
The real tragedy isn't the medical error-it's how normalized it's become. We treat medication reconciliation like a checkbox instead of a sacred contract between patient and system. The hospital isn't failing you because they're lazy-they're failing because the entire structure is optimized for throughput, not truth. You're not supposed to remember every pill you've ever taken. You're not supposed to know that ginkgo thins your blood like aspirin. You're supposed to trust the people who swore an oath. And when that trust breaks, we don't fix the system-we tell you to be more careful. That's not patient-centered care. That's punishment for being human.
January 3, 2026 AT 22:24
Andy Heinlein
bro i printed my whole med list on a sticky note and taped it to my fridge after i got out lol
January 4, 2026 AT 00:13
Ann Romine
I'm from a culture where elders are the keepers of family medicine knowledge. My grandmother used to write down every pill in a little notebook with the doctor's name and why it was given. I carried that habit into adulthood. Now I hand my list to every new provider. It's not just practical-it's ancestral.
January 5, 2026 AT 08:07
Todd Nickel
There's a documented gap between discharge documentation and actual patient comprehension. Studies show that even when patients receive a written list, 68% cannot accurately recite their regimen 72 hours later without prompting. The problem isn't just incomplete data-it's cognitive overload. The average discharge summary contains 12–18 distinct medication changes. The human working memory capacity for complex instructions is 4–7 items. This isn't negligence. It's systemic misalignment. We're asking patients to perform tasks that exceed neurocognitive limits. Until we redesign the communication architecture, we're just rearranging deck chairs on the Titanic.
January 5, 2026 AT 09:06
Austin Mac-Anabraba
Of course you're supposed to double-check your meds. If you can't read a prescription label or remember your own allergies, maybe you shouldn't be trusted with pills at all. This isn't rocket science. It's basic responsibility. The system doesn't owe you a safety net if you're too careless to keep track of what you're taking. I've seen people die because they didn't bother to ask one simple question. Don't be that person.
January 6, 2026 AT 01:49
Phoebe McKenzie
THIS IS WHY WE NEED TO DEFUND HOSPITALS AND GIVE EVERYONE A PERSONAL MEDICINE GUARDIAN. THEY'RE LYING TO YOU ABOUT YOUR DRUGS BECAUSE THEY'RE PAID BY PHARMA. YOU THINK THEY WANT YOU TO LIVE? THEY WANT YOU TO BE ON DRUGS FOREVER. THEY CHANGED MY BLOOD PRESSURE MED WITHOUT TELLING ME AND NOW I'M WEAK. I SAW THE BILL-THEY MADE $800 OFF THAT ONE PRESCRIPTION. THIS IS A COVER-UP.
January 7, 2026 AT 04:14
gerard najera
Always ask why a med was stopped.
January 8, 2026 AT 13:39
Stephen Gikuma
They're hiding the truth. Did you know the FDA allows hospitals to skip reconciliation if they're under budget? That's why they rush you out. It's not incompetence-it's policy. The same people who run the hospitals also own the labs that test your blood. They profit when you're back in the ER. You think this is coincidence? Wake up.
January 8, 2026 AT 16:52
Bobby Collins
my cousin said the hospital gave her a list but it had her dead uncle's meds on it lol
January 10, 2026 AT 01:38
Layla Anna
thank you for writing this 😊 i was so scared after my discharge last week and didn't know who to trust... i called my pharmacist and they caught a dangerous interaction i didn't even know about 🙏 you're right-pharmacists are the real heroes
January 10, 2026 AT 07:40
Heather Josey
This is an exceptionally well-structured and vital guide. I work in patient advocacy and have seen too many preventable readmissions. The checklist at the end should be mandatory for every discharge packet. I’ve distributed this to our entire network. Thank you for turning a complex clinical process into actionable, human-centered guidance. This is the kind of content that saves lives.
January 10, 2026 AT 18:32
Donna Peplinskie
I'm so glad someone wrote this-my mom was discharged last year and they forgot to restart her thyroid med for three weeks. She was exhausted, confused, and nearly fell down the stairs. We didn't catch it until her primary care doctor called to follow up. I've been telling everyone I know to print their own med list before admission. And yes, herbal supplements matter-my sister took turmeric with her blood thinner and ended up in the ER with internal bleeding. Please, please, please don't assume anything is 'natural' and therefore safe. Always tell your team everything.
January 11, 2026 AT 05:47