L‑Tryptophan & Antidepressants: Overlap, Risks & Safe Use
- Colin Hurd
- 25 October 2025
- 11 Comments
Serotonin Syndrome Risk Calculator
Calculate Your Risk
Ever wondered why a simple amino‑acid supplement can throw a wrench into your antidepressant regimen? The chemistry behind L‑tryptophan is a dietary essential amino acid that serves as the sole precursor for serotonin (5‑hydroxytryptamine) makes that question more than academic. Below you’ll find a step‑by‑step rundown of how tryptophan feeds the brain’s serotonin factory, which drug classes share that pathway, and what safety nets you need to build before mixing the two.
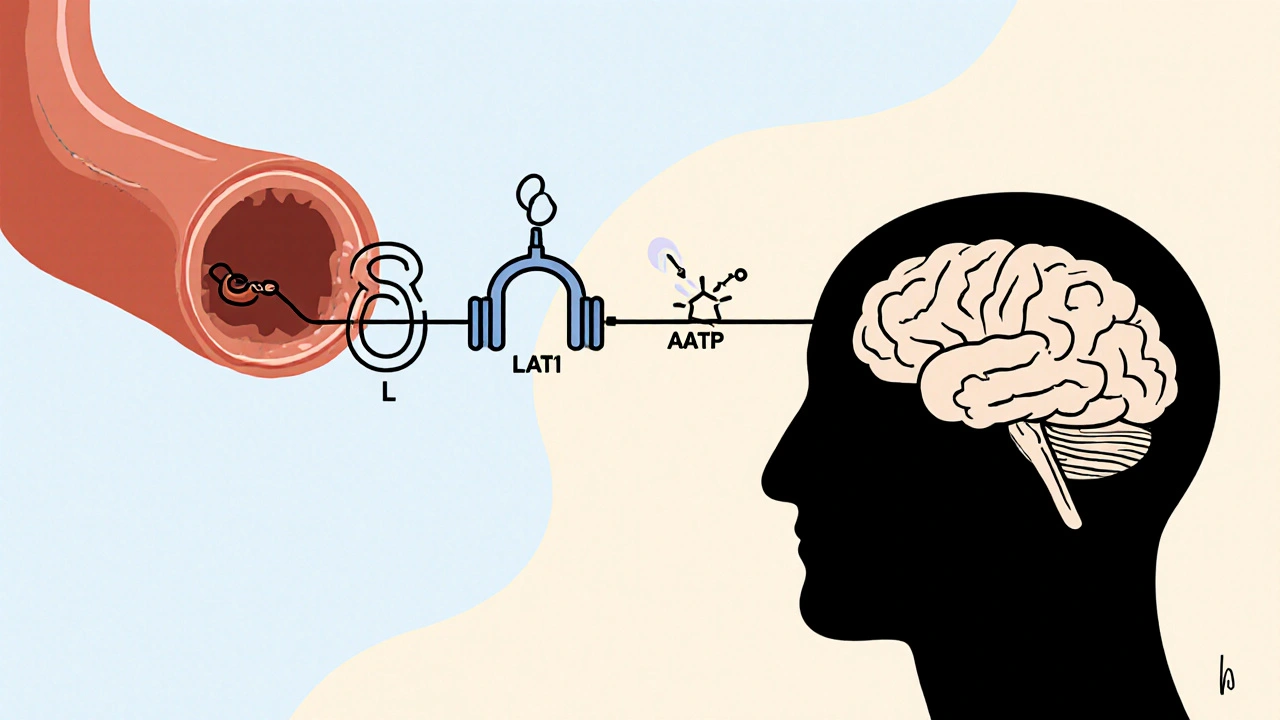
How L‑Tryptophan Turns Into Brain Serotonin
When you eat protein‑rich foods, tryptophan travels in the bloodstream bound to albumin. To get into the brain it must hitch a ride on the large neutral amino‑acid transporter (LAT1). Once across the blood‑brain barrier the molecule undergoes a two‑enzyme chase:
- Tryphangan hydroxylase (TPH) adds a hydroxyl group, converting tryptophan to 5‑hydroxytryptophan (5‑HTP).
- Aromatic L‑amino‑acid decarboxylase (AADC) strips away a carboxyl group, yielding serotonin (5‑HT).
Because the brain can’t store large serotonin pools, its synthesis rate bends directly to plasma tryptophan levels. Delgado et al. (1990) showed that a 90 % dip in plasma tryptophan slashes central serotonin by roughly the same margin within a single day.
Which Antidepressants Share the Serotonergic Highway?
Antidepressants fall into two broad camps:
- Selective serotonin reuptake inhibitors (SSRIs) keep serotonin hanging around in the synapse by blocking its re‑uptake transporter.
- Non‑serotonergic agents such as bupropion (dopamine‑noradrenaline reuptake inhibitor) or mirtazapine work mainly on dopamine, norepinephrine, or histamine pathways.
Then there are the older, broader‑spectrum drugs:
- Tricyclic antidepressants (TCAs) like amitriptyline touch both serotonin and norepinephrine re‑uptake.
- Monoamine oxidase inhibitors (MAOIs) prevent breakdown of serotonin, norepinephrine, and dopamine.
All of the above either boost serotonin directly (SSRIs, MAOIs, TCAs) or rely on a functional serotonin system to show full effect.
Clinical Evidence of Overlap: What the Numbers Say
Rapid tryptophan depletion (RTD) studies are the gold standard for testing serotonin dependence. When researchers stripped away tryptophan from patients on SSRIs, nearly half (47 %) slipped back into depressive relapse within 5‑8 hours. By contrast, only 9 % of unmedicated or fully remitted participants showed the same dip (Moncrieff 2022).
TCAs paint a different picture. Charney’s 1984 trial reported a 37‑42 % boost in prolactin release after a tryptophan challenge, suggesting that these drugs amplify tryptophan‑driven serotonin synthesis. MAOIs behaved similarly, enhancing serotonin turnover when extra tryptophan was supplied.
Non‑serotonergic drugs like bupropion didn’t trigger relapse at all in RTD protocols (0 % across three studies, Moore 2000). This split confirms a pharmacological rule of thumb: the more a medication leans on serotonin, the more it will feel the push‑or‑pull of supplemental tryptophan.
Safety First: Serotonin Syndrome and Dose Limits
Serotonin syndrome is the scary‑sounding but real risk when you stack two serotonergic agents. Symptoms range from mild (shivering, sweating) to severe (hyperthermia, seizures). Survey data from Sermo (2022) reveal that 73 % of psychiatrists avoid recommending tryptophan while a patient is on an SSRI, precisely because the interaction isn’t predictable.
Regulatory bodies have drawn hard lines on dosing. The European Food Safety Authority caps supplemental intake at 5 g per day, while the American Psychiatric Association recommends a therapeutic window of 1‑3 g per day for at least four weeks before judging efficacy. Keep plasma tryptophan in the 80‑120 µmol/L band; any higher pushes you closer to excess serotonin especially if a reuptake blocker is already on board.
Historical context matters, too. The 1989 contamination episode-where 1 500 cases of eosinophilia‑myalgia syndrome were linked to impure tryptophan-left a lasting scar. Modern manufacturers must now certify purity, but a 2021 FDA audit still found 41 % of products missing mandatory serotonin‑syndrome warnings.
Practical Guidance for Clinicians and Patients
Here’s a checklist you can paste into a clinic note or personal health journal:
- Confirm baseline stability. Patient should be on a steady SSRI dose for at least two weeks before adding tryptophan.
- Start low, go slow. Begin at 500 mg/day, increase by 250‑500 mg weekly until 1‑3 g/day is reached.
- Monitor plasma levels. Draw blood at weeks 2 and 4; aim for 80‑120 µmol/L.
- Watch for serotonin syndrome. Any sudden sweating, agitation, or fever → stop supplement and re‑evaluate medication.
- Plan wash‑out periods. If switching from an SSRI to a non‑serotonergic agent, allow a 7‑10‑day gap before adjusting tryptophan dose.
Patients on non‑serotonergic drugs (bupropion, mirtazapine) can often tolerate up to 3 g/day with minimal serotonin‑related side effects, but they should still heed the plasma‑level checks because individual genetics can tilt the balance.
Market Snapshot: Why the Debate Persists
The global tryptophan market hit US$347.8 million in 2022 and is projected to grow 7.3 % annually through 2030. In the U.S., about 29 % of psychiatrists sprinkle tryptophan into treatment plans for SSRI partial responders, whereas in Germany the figure jumps to 68 % thanks to prescription‑only status under the name “Trankimazin.” The disparity stems from regulatory lag: EFSA allows a 1 g/day claim for “psychological function,” while the FDA treats tryptophan as a plain dietary supplement with no therapeutic claims.
Meanwhile, research funding is shifting. After Moncrieff’s 2022 umbrella review questioned the serotonin‑depression link, the NIMH redirected $14.7 million in 2023 toward studies on the kynurenine pathway-an alternative route where tryptophan is broken down into metabolites that may be more directly tied to mood disorders.
Bottom Line: When Is L‑Tryptophan Worth Adding?
If you’re on a serotonergic antidepressant and struggling with residual symptoms, a carefully supervised tryptophan trial (1‑3 g/day, 4‑6 weeks, plasma monitoring) can boost serotonin enough to tip the scales in your favor. If you’re already responding well, the risk of serotonin syndrome outweighs any marginal gain. For non‑serotonergic regimens, tryptophan is generally safe and may improve sleep or mood, but keep an eye on gastrointestinal tolerance-about 22 % of supplement users report mild stomach upset at doses above 1 g.
In practice, the decision hinges on three questions:
- Is the current antidepressant primarily serotonergic?
- Has the patient reached a stable therapeutic dose?
- Can you monitor plasma tryptophan and watch for adverse signs?
Answer “yes” to all three, and you have a solid, evidence‑backed case for a trial. Answer “no,” and stick with what’s already working.
| Antidepressant Class | Primary Mechanism | Relapse Rate with RTD* | Serotonin Syndrome Risk (≥1 g L‑Tryptophan) |
|---|---|---|---|
| SSRIs | Re‑uptake inhibition | 47 % | Moderate‑High |
| MAOIs | Monoamine breakdown block | 42 % | High |
| TCAs (amitriptyline, desipramine) | Dual re‑uptake block | 30‑35 % | Moderate |
| Non‑serotonergic (bupropion, mirtazapine) | Dopamine/NE or histamine | 0 % | Low |
*Based on pooled data from rapid tryptophan depletion studies (Moncrieff 2022; Moore 2000).
Frequently Asked Questions
Can I take L‑tryptophan with my SSRI without a doctor’s approval?
No. Because both act on serotonin, unsupervised stacking can trigger serotonin syndrome or reduce the SSRI’s efficacy. A clinician should set a trial protocol, monitor plasma levels, and watch for side‑effects.
What dose of L‑tryptophan is considered safe?
Most authorities cap daily supplemental intake at 5 g. Clinical augmentation studies use 1‑3 g per day for 4‑6 weeks, with plasma monitoring to stay within 80‑120 µmol/L.
Does tryptophan help if I’m not on any antidepressant?
Evidence is mixed. Some short‑term trials report modest mood lifts and better sleep, especially at 500‑1 000 mg doses, but large‑scale studies haven’t confirmed a strong antidepressant effect in drug‑free participants.
Are there any foods that naturally boost tryptophan enough to matter?
Turkey, chicken, cheese, nuts, and beans contain tryptophan, but dietary amounts rarely raise plasma levels to the therapeutic range without supplementation. A balanced diet can support baseline serotonin production, though.
What are the early signs of serotonin syndrome I should watch for?
Look for agitation, rapid heart rate, high blood pressure, dilated pupils, muscle rigidity, tremor, sweating, and gastrointestinal upset. If symptoms appear, stop the supplement and seek medical help immediately.



Comments
Jennie Smith
Wow, this deep‑dive really shines a light on how intertwined tryptophan and our meds can be! I love the way you broke down the biochemical steps – it makes the whole process feel less intimidating. For anyone juggling an SSRI, this checklist feels like a lifeline. Keep sprinkling that colorful science, it's both empowering and easy to digest. 🌈
October 25, 2025 AT 18:28
Donal Hinely
Nice breakdown, but let’s not forget cultural diets matter too – some folks get enough tryptophan from their everyday meals.
November 6, 2025 AT 07:14
christine badilla
Hold up, are we really talking about throwing another supplement into the mix without a warning label? It's like adding fireworks to a bonfire and hoping for a pretty show. I can already feel the drama building in my gut. The risk of serotonin syndrome is no joke – it's the horror movie of the psych world. And that 1989 contamination saga? Still gives me chills.
November 17, 2025 AT 21:01
Octavia Clahar
Honestly, the drama is overblown if you follow the guidelines. The checklist you gave is solid and keeps things safe.
November 29, 2025 AT 10:48
Justin Scherer
Great info. If you’re starting tryptophan, go low and watch your body. Keep a journal of any changes.
December 11, 2025 AT 00:34
Greg Galivan
Low start is fine but dont skip the plasma check its critical.
December 22, 2025 AT 14:21
Anurag Ranjan
Monitor levels early. It saves future trouble.
January 3, 2026 AT 04:08
James Doyle
While the succinct advice is appreciated, we must also consider the broader ethical implications of supplementing psychopharmacology without robust longitudinal data. The temptation to self‑administer based on a handful of studies can erode the patient‑clinician trust that is foundational to effective treatment. Moreover, the commercial incentives driving supplement proliferation often outpace the rigorous safety evaluations mandated for prescription drugs. It is our responsibility, as a community, to demand higher standards of evidence before normalizing such practices. Ignoring these considerations risks not only individual adverse events but also public health setbacks. Ultimately, a cautious, evidence‑first approach safeguards both efficacy and safety.
January 14, 2026 AT 17:54
ALBERT HENDERSHOT JR.
The interplay between L‑tryptophan and serotonergic agents is a textbook example of pharmacodynamic synergy, and understanding it can transform clinical outcomes. First, tryptophan serves as the sole precursor to serotonin, meaning its availability directly caps how much neurotransmitter the brain can produce. Second, SSRIs, MAOIs, and even TCAs amplify the impact of any added tryptophan by either preventing reuptake or inhibiting breakdown, which can tip the balance toward excess serotonergic activity. Third, the risk of serotonin syndrome escalates when both pathways are potentiated simultaneously, manifesting as autonomic dysregulation, neuromuscular hyperactivity, and cognitive changes. Fourth, the literature shows that rapid tryptophan depletion precipitates relapse in nearly half of patients on SSRIs, underscoring their dependence on the amino‑acid pool. Fifth, however, non‑serotonergic agents like bupropion show negligible relapse rates under the same conditions, highlighting the specificity of the interaction. Sixth, dosing guidelines worldwide converge on a safe supplemental window of 1‑3 g per day, with an upper ceiling of 5 g to avoid toxicity. Seventh, plasma tryptophan monitoring between 80‑120 µmol/L provides an objective metric to tailor therapy and mitigate risk. Eighth, historical events such as the 1989 eosinophilia‑myalgia syndrome remind us that purity and regulatory oversight are non‑negotiable. Ninth, modern manufacturers must now adhere to stringent GMP standards, yet audits still reveal gaps in warning labels that can leave clinicians in the dark. Tenth, clinicians should always obtain informed consent, outlining both potential benefits and the specter of serotonin syndrome. Eleventh, patient education about early signs-sweating, agitation, tremor-can expedite intervention. Twelfth, a structured wash‑out period when switching agents further reduces adverse interactions. Thirteenth, the therapeutic niche for tryptophan is most compelling in partial responders to serotonergic antidepressants, where incremental serotonergic boost may tip the scales toward remission. Fourteenth, for patients stable on non‑serotonergic meds, tryptophan can be a low‑risk adjunct for mood and sleep without major serotonin concerns. Fifteenth, the burgeoning market signals both interest and the need for clearer clinical guidelines. Sixteenth, ultimately, the decision to augment with tryptophan should rest on a trio of criteria: serotonergic medication, stable dosing, and capacity for monitoring. 😊
January 26, 2026 AT 07:41
Suzanne Carawan
Oh sure, because adding another pill always solves everything 🙄
February 6, 2026 AT 21:28
Kala Rani
I think this whole thing is overhyped
February 18, 2026 AT 11:14