Massage Therapy for Muscle Spasms: Benefits, Types, and Safe Use

- Colin Hurd
- 27 August 2025
- 16 Comments
When a muscle seizes mid-run or halfway through a workday, you don’t care about Latin names-you just want it to release. Massage can calm a spasm fast, but the trick is using the right pressure, at the right time, for the right kind of spasm. Here’s a clear, evidence-backed guide that shows what works, what doesn’t, and how to do it safely.
- TL;DR: Massage reduces pain, relaxes tight muscle fibers, boosts local blood flow, and improves range of motion. Expect partial relief in minutes and steadier gains across a few sessions.
- Best for overuse spasms and trigger points; it won’t fix nerve compression or severe electrolyte problems, but it can ease guarding and pain.
- Start with gentle pressure (4-6/10), 30-90 seconds per tender spot, then re-test movement. Heat first, light stretch after.
- Use trigger point or myofascial techniques for stubborn knots; book a pro if pain radiates, weakness/numbness shows up, or spasms keep returning.
- Red flags: new severe pain after trauma, fever with muscle pain, calf swelling/heat, chest pain, or bowel/bladder changes-see a doctor.
Why massage helps muscle spasms (and when it doesn’t)
First, quick definitions so we’re talking about the same thing:
- Muscle spasm: a sudden, involuntary contraction-often protective-after overuse, strain, or sitting too long.
- Trigger point (knot): a tiny patch of contracted fibers inside a muscle that’s tender and can refer pain.
- Cramp: an intense spasm, often in calves/feet, sometimes linked to fatigue, dehydration, or electrolytes.
- Spasticity: increased muscle tone from nerve/brain issues (e.g., after stroke); different problem, different playbook.
How does massage therapy calm a spasm? Three main ways:
- Pain gate + nervous system downshift: Pressure and slow strokes flood touch receptors that dampen pain signals (gate-control) and nudge your body toward a parasympathetic state-lower arousal, lower muscle tone.
- Local circulation: Gentle compression and release improve microcirculation, helping clear metabolites and reduce the “locked” feel in a knot.
- Muscle spindle reset: Sustained pressure on a taut band reduces excitability in the spindle reflex, letting the muscle lengthen without fighting you.
What does the research say?
- A Cochrane review (2023) on neck pain found short-term pain relief and function gains from massage compared with minimal care; quality varied but effects were consistent across trials.
- The American College of Physicians guideline (2017) recommends massage as a non-drug option for acute and chronic low back pain.
- A Sports Medicine meta-analysis (2018) reported small-to-moderate benefits of massage on soreness and performance recovery after intense exercise.
- Australian low back pain clinical care standards (2022) position hands-on therapies as adjuncts-useful for symptom relief, combined with movement and education.
So yes-massage often helps the pain and stiffness that come with spasms and trigger points, and it can reduce how often they flare when combined with load management (smart training and breaks) and sleep.
When it’s not the main fix:
- Nerve compression (e.g., sciatica with leg weakness or numbness): massage may soothe guarding but won’t remove compression; you need a physio/doctor plan.
- Electrolyte or drug causes (e.g., diuretics): address the underlying issue first; massage is supportive.
- Spasticity from neurological conditions: gentle massage can reduce discomfort, but medical/rehab strategies drive the results.
Practical benefits you can expect if your spasm is the typical overuse or trigger-point kind:
- Rapid pain reduction (often 20-50% in the session) and easier movement.
- Fewer flare-ups over 1-3 weeks when paired with light strength work and better posture breaks.
- Improved sleep if spasms used to wake you or make it hard to get comfortable.

How to use massage for spasms: techniques, step-by-step, and when to see a pro
You’ve got three options: self-massage, a partner, or a trained therapist. Start simple, test, and only go deeper if your body says yes.
Pressure rule of thumb: stay at a tolerable 4-6/10 discomfort. Sharp, zappy, or breath-holding pain is too much.
Before you begin
- Warm the area (3-5 minutes): heat pack or a hot shower.
- Pick a tool: fingers, a ball (tennis/lacrosse), or a foam roller. For small knots (neck/shoulder), a ball wins. For quads/calves, roller or elbow pressure works.
- Hydrate-especially in hot Perth summers-and do 1-2 slow breaths to ease tension.
Self-massage protocol (universal)
- Scan for tender spots: press or roll slowly until you find a tight, sore patch.
- Apply steady pressure (30-90 seconds): breathe slowly; let the tissue melt, don’t grind.
- Release and move: after pressure, do 5-10 gentle reps through pain-free range (e.g., ankle pumps after calf work, neck rotations after shoulder work).
- Stretch lightly (20-30 seconds), no bouncing.
- Re-test your trigger movement (turn your head, bend forward, jog lightly). If it’s smoother or less painful, you’re on track.
Targeted playbooks
- Calf spasm/cramp: Put a ball under the calf, mid-belly. Sink in, hold 45-60 seconds. Move the ankle up/down while maintaining pressure. Repeat 2-3 spots. If it’s a night cramp, you can gently dorsiflex the foot (toes up) while breathing to invite release; don’t wrench it.
- Neck/upper trap spasm from desk work: Lean against a wall with a ball on the upper trap (top of shoulder). Pressure 30-60 seconds per knot. Follow with 5 slow shoulder rolls and 5 chin nods. Keep screens at eye level to prevent quick relapse.
- Low back spasm after lifting: Avoid hard rolling directly on the low back. Work glutes and hips instead (ball on the glute, 60-90 seconds); then do cat-cow and hip hinges without load. If pain shoots down the leg or you feel numbness/weakness, stop and book a clinician.
- Hamstring or quad spasm after sport: Foam-roll slowly, pausing on hot spots. Two passes is enough. Add 5-8 air squats or bridges afterward to “seal” the relaxation with movement.
Dosage and frequency
- Acute spasm: 1-2 short sessions per day for 2-4 days, then taper.
- Chronic knots: 3-4 sessions per week, 5-10 minutes each area, for 2-3 weeks.
- Pro sessions: 30-60 minutes weekly for 2-3 weeks can break the cycle, then space to maintenance as needed.
Which technique fits which spasm?
- Trigger point therapy: best for pinpoint, referral-prone knots (upper traps, calves, glutes).
- Myofascial release: good when the entire area feels “stuck” with multiple taut bands.
- Sports massage: blends deeper strokes with movement; handy around training blocks.
- Swedish/relaxation: great for nervous system downshift when stress drives your tension.
- Deep tissue: okay once the area tolerates pressure; too early can provoke guarding.
When to see a trained professional
- Spasms keep returning in the same spot despite a week of self-care.
- Pain shoots, tingles, or there’s weakness or numbness.
- There was a pop, bruising, or you can’t load the limb (suspect a tear).
- Night pain that doesn’t ease with position changes, or systemic symptoms (fever, unexplained weight loss).
In Australia, look for a Remedial Massage Therapist with a nationally recognized qualification (HLT level) and membership with Massage & Myotherapy Australia or similar. For nerve-related signs, a physiotherapist (AHPRA-registered) should be your first stop. Private health extras may rebate part of remedial massage; Medicare does not cover massage sessions.
Common pitfalls
- Pressing too hard, too soon. Bruising = you overshot.
- Only massaging, never moving. Always pair with gentle range-of-motion or light strength.
- Chasing pain in the wrong spot. For low back, check hips/glutes. For calf, also treat the soleus (lower calf) and foot.
- Skipping warm-up. Heat and slow breathing amplify the effect.
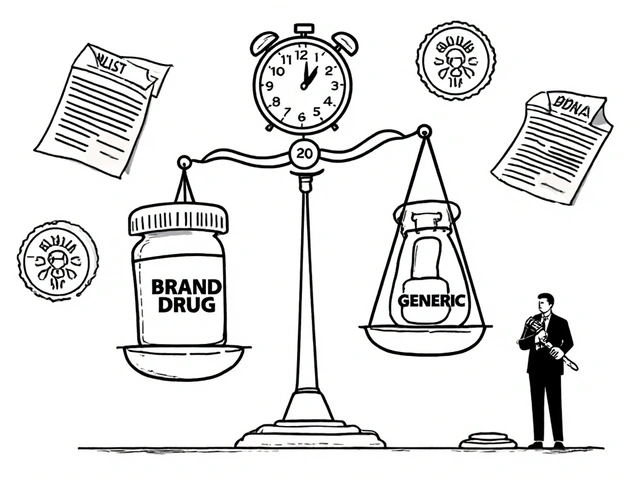
| Technique | Best for | Evidence snapshot | Typical session | Perth 2025 cost (AUD) | Notes |
|---|---|---|---|---|---|
| Trigger point therapy | Local knots in traps, calves, glutes | Consistent short-term pain relief; good for ROM | 30-45 min focused | $80-$120/hr | Expect referral sensations during pressure |
| Myofascial release | Widespread tightness, multiple taut bands | Short-term relief; pairs well with exercise | 45-60 min | $90-$130/hr | Slower, sustained holds; no oil needed |
| Sports massage | Training-related spasms, recovery | Small-moderate effect on soreness/recovery | 30-60 min | $90-$140/hr | Often combined with stretching |
| Swedish/relaxation | Stress-driven tightness | Reduces perceived tension, pain | 60 min | $80-$120/hr | Nervous system calm-down |
| Deep tissue | Chronic stiffness once acute pain settles | Helpful when dosed right; easy to overdo | 45-60 min | $90-$140/hr | Communicate pressure clearly |

Checklists, decision guide, Aussie-specific tips, and FAQs
Quick pre-session checklist
- Any red flags (trauma, fever, chest pain, calf swelling/heat, neuro signs)? If yes, medical review first.
- Warmth: 3-5 minutes heat or shower.
- Tool ready: ball/roller, towel, water.
- Pressure plan: aim for 4-6/10 discomfort, breathe steadily.
After-session checklist
- Re-test movement. Is it smoother or less painful by at least 20%? Good-repeat tomorrow.
- Light stretch, then 5-10 reps of a simple strength move (e.g., calf raises, band pull-aparts).
- Hydrate; in summer heat, add a pinch of salt to your water if you sweat heavily (unless you’re on a low-salt plan).
- Note any bruising or zappy pain; ease up next time.
Simple decision guide
- If the spasm is new, from a clear trigger (long drive, hard workout), and eases with heat and gentle pressure: self-massage first.
- If pain shoots, you feel numb/weak, or the spasm keeps returning in the same spot: see a physio or remedial therapist.
- If you wake at night with calf cramps weekly: check hydration, review meds with your GP, train calves gradually, and use massage for comfort.
- If you’re on blood thinners: massage is okay, but keep pressure moderate and avoid deep work over thin tissues.
Aussie-specific notes (2025)
- Remedial massage rebates are usually under Private Health Extras; amounts vary ($20-$50 back). Medicare does not rebate massage sessions.
- In WA heat waves, cramps spike with dehydration. Plan fluids around outdoor work and sport; massage helps the aftermath, not the cause.
- Check your therapist’s association membership and receipts if you claim Extras.
Mini-FAQ
- How long until a spasm lets go? Many ease within minutes of steady pressure. If nothing changes after 2-3 sessions, switch strategy or see a clinician.
- Will massage stop night leg cramps? It can reduce frequency if cramps are fatigue-related by relaxing tight bands, but it won’t fix electrolyte or medication causes on its own. A 2020 review found mixed results for magnesium in non-pregnant adults; talk to your GP if cramps are frequent.
- How often should I book a massage? For a stubborn knot, weekly for 2-3 weeks works well; then stretch sessions out. Keep up short self-sessions between visits.
- Can I massage a fresh muscle tear? Not in the first 48-72 hours if there’s sharp pain, swelling, or bruising. Rest, gentle pain-free movement, and medical advice first. Later, light work around-not on-the tear can help.
- Is there such a thing as “releasing toxins”? No. Massage changes circulation and nervous system tone; you may feel flushed or sleepy, which is normal, but it’s not “detox.”
- Is massage safe in pregnancy? Yes with a trained practitioner, especially in the second/third trimester. Avoid deep work on calves if there’s swelling or pain-rule out DVT first if you’re concerned.
- What about DOMS after the gym? Light massage can cut soreness and restore range a bit faster. Keep pressure low and pair with easy movement.
Pro tips
- Pair 60 seconds of pressure with 5 slow breaths to amplify relaxation.
- If a spot won’t let go, treat the neighbors (e.g., for calf, also treat the soleus and the arch of the foot).
- Finish with the movement you want to improve. Training the new, easier range makes gains stick.
- Log your triggers: long drives, a new shoe, or a training spike often predict where the next knot shows up.
Evidence pointers (for the curious)
- Cochrane Review (2023): massage for neck pain-short-term pain and function improvements versus minimal care.
- American College of Physicians Guideline (2017): recommends massage as a non-drug option for acute/chronic low back pain.
- Sports Medicine Meta-analysis (2018): small-to-moderate benefits for post-exercise soreness and recovery.
- Australian Low Back Pain Clinical Care Standard (2022): supports hands-on care as adjuncts to movement-focused plans.
Next steps and troubleshooting by scenario
- Desk worker with neck spasm: Ball on upper trap, 45 seconds x 3 spots; five chin nods; raise monitor to eye level; micro-breaks every 30-45 minutes. If headaches or arm tingling, see a clinician.
- Runner with calf spasm: Heat 3 minutes; ball holds on calf; 2 sets of 15 calf raises (easy tempo) later that day; check shoe wear. If the calf keeps cramping at night, review fluids and training spikes.
- Tradie with low back spasm: Treat glutes and hips, not just the back. Hip hinges with a dowel to relearn the pattern. If pain radiates below the knee or there’s weakness, book a physio.
- Pregnant with leg cramps: Gentle calf holds, ankle pumps, and hydration. If one calf is swollen, hot, and tender-urgent medical check.
- Older adult with nocturnal cramps: Evening calf massage, warm shower, and light stretches; discuss meds (diuretics, statins) with your GP; consider magnesium only after medical advice due to mixed evidence.
The bottom line: used with smart pressure and paired with movement, massage is one of the simplest ways to take the edge off a spasm and teach your muscles to relax again. If it keeps coming back, dig into why-load, posture, sleep, stress-and get a pro to help you build a plan that sticks.


Comments
Craig Stephenson
Great rundown! I love how you break down the pressure numbers – 4‑6/10 is spot on for most folks. The quick‑hit relief in minutes is a huge win for anyone stuck at a desk. Pairing the massage with a few light reps really cements the benefit. Thanks for the clear guide.
August 27, 2025 AT 09:36
Tyler Dean
They don’t want you to know that massage is just a ploy from the elite to keep us docile.
August 27, 2025 AT 20:43
Susan Rose
Super helpful guide – especially the part about warming up before you start. I’ve been using a heat pack for my neck and it makes the knots melt faster. Also, the checklist makes sure I don’t miss any steps.
August 28, 2025 AT 07:50
diego suarez
I agree with the emphasis on gentle pressure. It’s easy to think “harder is better,” but that just spikes guarding. The advice to test movement after each hold is a smart way to gauge progress. Keeping breathing steady also calms the nervous system.
August 28, 2025 AT 18:56
Eve Perron
What a comprehensive post! I appreciate the blend of evidence citations and practical steps – it makes the science feel accessible. The inclusion of Australian-specific details, like the private health extras, is incredibly useful for readers down under. I also love the visual table comparing techniques; it instantly clarifies which method fits each scenario. The way you spell out the “quick pre‑session checklist” feels like a mini‑protocol that anyone can print and keep by the bedside. Your notes on hydration and electrolyte balance are spot‑on, especially when dealing with night cramps in hot summers. Also, the reminder about red flags – fever, swelling, numbness – is crucial; many people overlook those warning signs. The “Pro tips” section with breathing cues and treating neighboring muscles adds that extra layer of depth that separates a good guide from a great one. Finally, the clear call‑to‑action at the end, urging readers to pair massage with movement and posture work, reinforces the holistic approach needed for lasting relief.
August 29, 2025 AT 06:03
Josephine Bonaparte
Nice work! A quick reminder: after a session, sip water with a pinch of salt if you sweat a lot – helps replace electrolytes and keeps the muscles happy.
August 29, 2025 AT 17:10
Meghan Cardwell
Massage therapy is more than just a feel‑good treat; it’s a neuro‑physiological tool that can actually dial down the hyper‑excitable motor units that cause a spasm.
When you apply a steady 4‑6/10 pressure, you’re engaging the large‑diameter A‑beta fibers that close the nociceptive gate in the dorsal horn.
That gate‑closing effect lets descending inhibitory pathways take over, shifting the autonomic balance toward parasympathetic dominance.
The increased local microcirculation that follows also flushes out metabolites like bradykinin and substance P that sustain the contractile loop.
Research from the 2023 Cochrane review on neck pain showed a modest but consistent reduction in pain scores after a series of 30‑minute sessions.
A 2017 ACP guideline even gave massage a Level B recommendation as a first‑line non‑pharmacologic option for low‑back pain.
In sports medicine, a 2018 meta‑analysis found that post‑exercise massage shaved off about 10 % of perceived soreness and helped athletes regain range of motion faster.
The key, however, is to pair the hands‑on work with movement; otherwise the gain is fleeting.
For a typical overuse trigger point, start with a 30‑second hold, breathe slowly, then follow with five to ten functional reps of the target joint.
If the spot refuses to release, expand the pressure to the surrounding fascia – the myofascial cascade often breaks the knot’s “anchor.”
Always keep the discomfort below a 6/10 threshold; crossing into sharp pain risks triggering a protective guarding response that undoes the whole session.
Hydration after the work is crucial because the increased circulation mobilizes interstitial fluid that the body needs to re‑absorb.
For chronic knots, schedule three to four short sessions per week for two weeks, then transition to self‑massage and targeted strengthening.
And don’t forget to watch for red flags: radiating numbness, sudden swelling, or systemic symptoms mean you should pause and seek a clinician.
In short, massage is a low‑cost, low‑risk adjunct that, when done correctly, can turn a stubborn spasm into a fleeting annoyance.
August 30, 2025 AT 04:16
stephen henson
Love the detail, especially the breathing cue! 😌 It really helps me stay relaxed during the hold.
August 30, 2025 AT 15:23
Manno Colburn
i caugth a knght one too but i wnt to say hibit ushould not use 2 much force becasue it can hazzard your ptients you need to find the balance. Also do not just do massage you should combine it with the crazy movements the big muscles that hold the body. Also i find that when i do it early in the day it works more it's like your body is not so busy. remember to stay hush your breaht and you should have a good effect. wavelike, more progress, make sure to check for any red phags.
August 31, 2025 AT 02:30
Namrata Thakur
Beautiful explanation, and I love that you highlighted the importance of checking for red flags before starting. In my experience, a gentle calf massage after a run dramatically reduces night cramps, especially when combined with proper hydration.
August 31, 2025 AT 13:36
Chloe Ingham
Wow, this guide reads like a novel – love the drama! The part about “gate‑control” really hit the spot.
September 1, 2025 AT 00:43
Mildred Farfán
Nice work, though I’m still skeptical about “detox” claims – it’s just good circulation, not some mystical cleansing. Still, the practical steps are solid.
September 1, 2025 AT 11:50
Danielle Flemming
This is super encouraging! I’ve been scared of deep‑tissue work, but you broke it down so nicely. I’m going to try the ball technique on my traps tomorrow and then do those gentle chin nods. The checklist will keep me from missing anything, and I love the reminder to stay hydrated. Thanks for making it feel doable.
September 1, 2025 AT 22:56
Anna Österlund
Stop over‑complicating it – just press, breathe, and move. If it hurts, you’re doing it wrong.
September 2, 2025 AT 10:03
Brian Lancaster-Mayzure
I appreciate the balanced tone – you give enough science without drowning the reader. The recommendation to treat neighboring muscles is a nuance many overlook. I’ll definitely add the post‑session stretch routine to my protocol.
September 2, 2025 AT 21:10
Erynn Rhode
Great guide! I especially liked the clear separation of when to self‑massage versus when to see a professional – that helps prevent people from over‑doing it.
The emphasis on hydration and electrolyte balance after the session is something I’ve seen work wonders for my own recovery.
Also, the red‑flag checklist is a lifesaver; many ignore those signs until it’s too late.
One tip: after a massage, a short walk can help keep the circulation going and prevent stiffness.
Overall, this post combines solid evidence with practical steps, making it a go‑to reference for anyone dealing with spasms.
September 3, 2025 AT 08:16