Metabolic Enzyme Disorders: A Practical Overview
When working with Metabolic Enzyme Disorders, a group of inherited or acquired conditions where enzymes that control biochemical pathways malfunction, leading to build‑up of toxic substances or deficiency of essential metabolites. Also known as enzyme metabolism disorders, they often require lifelong monitoring and specialized treatment plans.
Key Concepts and Related Entities
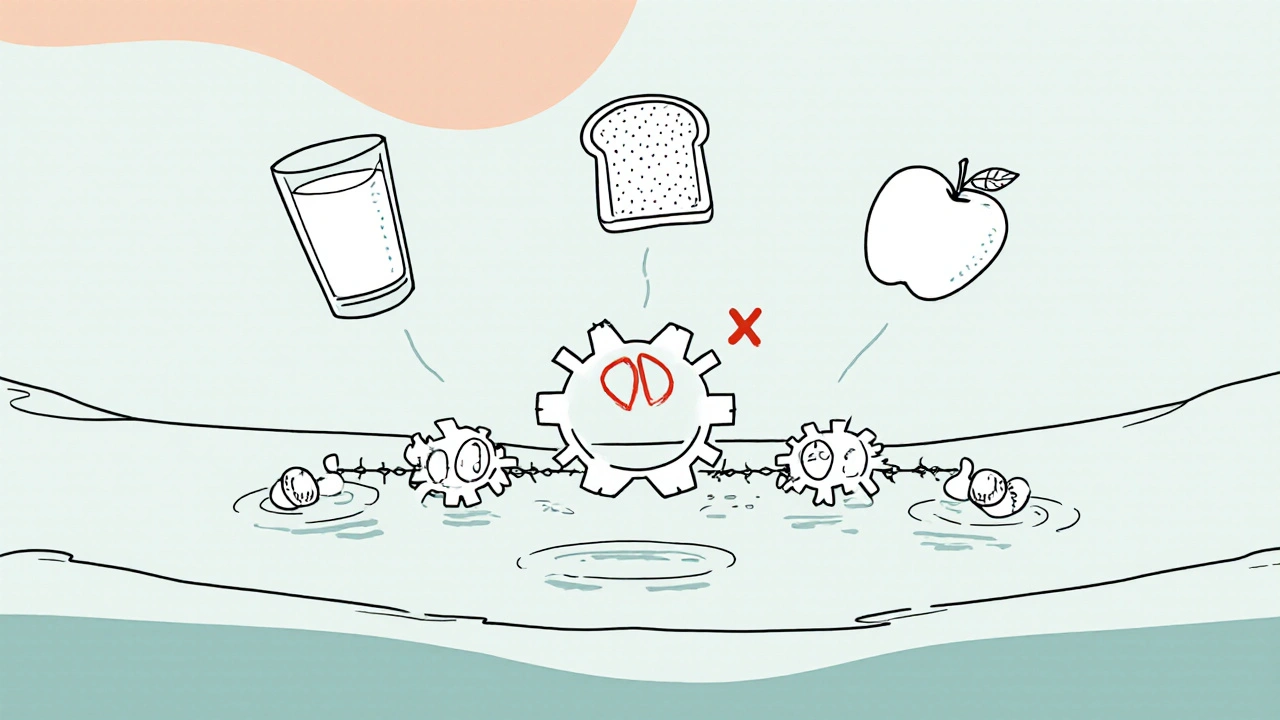
One core Enzyme Deficiency, the specific loss of activity in a single enzyme such as phenylalanine hydroxylase in phenylketonuria or glucocerebrosidase in Gaucher disease directly drives many metabolic enzyme disorders. Because enzymes act as catalysts in Metabolic Pathways, a single defect can ripple through multiple downstream processes, altering energy production, detoxification, and hormone synthesis. This interconnection means that clinicians must consider the whole pathway, not just the isolated enzyme.
Another decisive factor is Pharmacogenomics, the study of how genetic variations affect drug response, especially how altered enzymes change the way medications are metabolized. For patients with metabolic enzyme disorders, standard drug doses can cause unexpected toxicity or therapeutic failure. For example, a person with a CYP2D6 deficiency may process antidepressants like paroxetine much slower, raising the risk of side effects. Understanding these gene‑drug interactions enables personalized dosing and safer prescribing.
Detecting these conditions early often hinges on Genetic Testing, molecular analysis that identifies pathogenic variants in enzyme‑encoding genes, guiding diagnosis, prognosis, and family counseling. Newborn screening programs routinely check for disorders such as galactosemia or medium‑chain acyl‑CoA dehydrogenase deficiency, allowing treatment before irreversible damage occurs. In adults, targeted panels can uncover hidden enzyme issues that explain drug intolerance or unexplained metabolic symptoms.
These entities form a web of relationships: metabolic enzyme disorders encompass enzyme deficiency; enzyme deficiency requires metabolic pathway analysis; pharmacogenomics influences drug metabolism; and genetic testing enables accurate diagnosis. Together they shape a patient‑centered approach that blends biochemical insight with modern genetics.
The articles below reflect this ecosystem. You’ll find guides on medication safety during pregnancy (dexamethasone), comparisons of muscle relaxants (baclofen vs alternatives), the role of antidepressants (paroxetine for PTSD), and practical tips for buying affordable generics online. While each piece focuses on a specific drug or condition, they all intersect with metabolic enzyme disorders through the lenses of enzyme‑driven metabolism, pharmacogenomic considerations, and the importance of precise dosing. Dive in to see how these topics connect and how you can apply the knowledge to manage or understand metabolic enzyme disorders more effectively.
- Colin Hurd
- Oct, 21 2025
- 13 Comments
Enzyme Deficiency Disorders: Types, Symptoms & How to Recognize Them
Learn about enzyme deficiency disorders, their main types, symptoms, diagnosis, and treatment options. Get practical tips for managing conditions like lactase deficiency and PKU.