Psoriasis Infections: Causes, Risks, and What You Need to Know
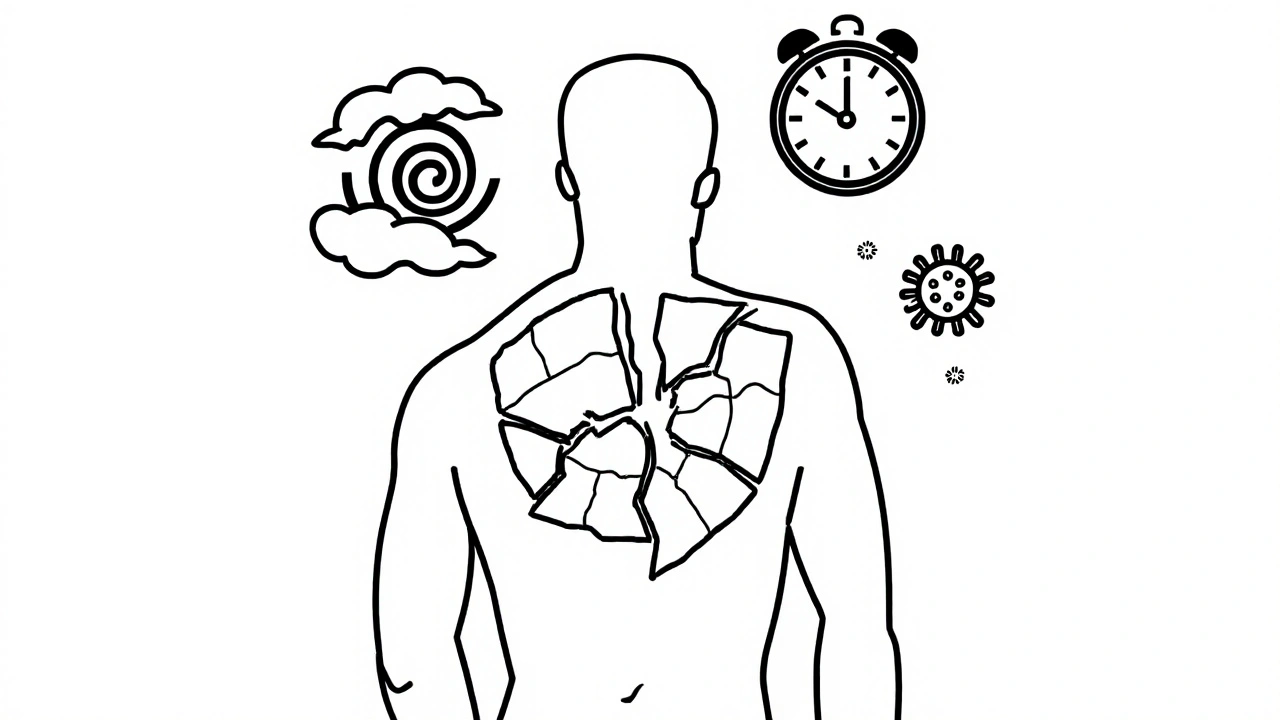
When you have psoriasis, a chronic autoimmune condition that causes thick, scaly patches on the skin. Also known as plaque psoriasis, it doesn’t just affect how your skin looks—it weakens your skin’s natural barrier, making it easier for bacterial infections, like Staphylococcus aureus, that commonly invade broken skin to take hold. These infections don’t just make psoriasis worse—they can trigger full flare-ups, spread to deeper tissue, or even lead to hospitalization if ignored.
People with psoriasis are more likely to get fungal infections, especially candida or ringworm, in skin folds or under scales. The itch-scratch cycle plays a big role: scratching opens tiny wounds, and moisture trapped under plaques creates the perfect environment for germs. Even minor cuts from dry skin or harsh treatments can become entry points. Some studies show over 60% of psoriasis patients have signs of bacterial colonization on affected skin—even without visible signs of infection. That’s why treating the infection isn’t optional—it’s part of managing the disease.
What makes this tricky is that psoriasis flares and infections often look similar: redness, swelling, pain, and pus. But you can’t treat them the same way. Antibiotics won’t help if it’s a fungal issue, and antifungals won’t touch a staph infection. That’s why seeing a doctor for proper testing—like a skin swab or culture—is critical. Once you know what you’re dealing with, treatment gets much simpler. Topical antibiotics like mupirocin, oral antibiotics like cephalexin, or antifungal creams can clear things up fast when used correctly.
And it’s not just about what you put on your skin. Your immune system is already overworked in psoriasis. When an infection hits, it throws your whole system off balance. That’s why stress, poor sleep, or even a cold can make both your psoriasis and any infection worse. Keeping your skin clean, moisturized, and intact is your first line of defense. Avoid picking at scales. Wear breathable fabrics. Don’t share towels or razors. These small habits cut your risk dramatically.
What you’ll find below are real, practical guides from people who’ve been there. You’ll see how antibiotics like cephalexin help fight bacterial outbreaks, why expired mupirocin is dangerous, and how to tell if your flare-up is really an infection. There’s also advice on what to bring to your doctor, how to spot early signs, and which treatments actually work without making things worse. No fluff. No guesses. Just clear, tested info to help you take control before things get serious.
- Colin Hurd
- Nov, 14 2025
- 9 Comments
Psoriasis Triggers: How Stress, Infections, and Skin Barrier Damage Cause Flares
Psoriasis flares are often triggered by stress, infections, and a damaged skin barrier. Learn how these three factors interact and what practical steps you can take to reduce flare frequency and regain control.