Warfarin vs. DOACs: Understanding Anticoagulant Safety Today

- Colin Hurd
- 6 January 2026
- 14 Comments
Choosing a blood thinner isn't like picking a vitamin. One wrong move can lead to a stroke, a bleed in the brain, or worse. For millions of people with atrial fibrillation, deep vein thrombosis, or mechanical heart valves, anticoagulants are life-saving. But not all anticoagulants are created equal. Two main types dominate today: warfarin, the old-school staple, and direct oral anticoagulants (DOACs), the newer alternatives. The question isn't just which works better-it's which is safer for you.
Warfarin: The Legacy Drug with a Heavy Burden
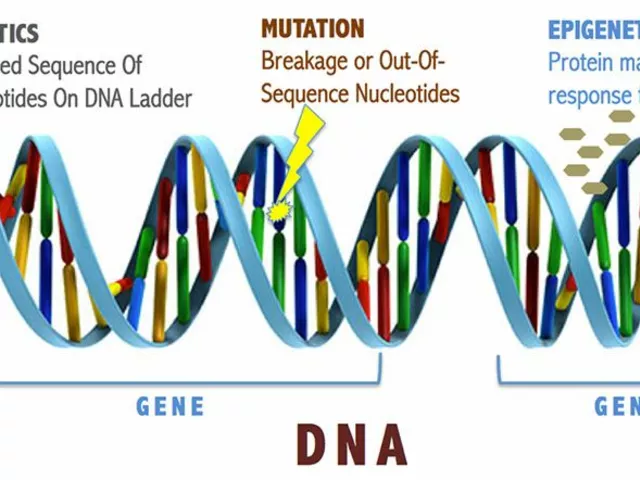
Warfarin has been around since the 1950s. It’s cheap, widely available, and doctors know it inside and out. But that familiarity comes at a cost. Warfarin doesn’t just thin your blood-it messes with your entire body’s vitamin K balance. That’s why you need frequent blood tests. Every few weeks, you get your INR checked to make sure your blood isn’t too thin or too thick. The goal? Keep your INR between 2.0 and 3.0. Miss a test, eat a big salad, start a new antibiotic, or skip a dose, and you’re out of range.
Over 300 drugs interact with warfarin. Antibiotics, painkillers, even some herbal supplements can send your INR skyrocketing or crashing. Vitamin K in leafy greens like kale, spinach, and broccoli directly opposes warfarin’s effect. That means you can’t just eat normally-you have to track your intake. One week you eat lots of greens, the next you don’t? Your INR swings. It’s exhausting.
And the risks? Warfarin users have a 50% higher chance of bleeding in the brain compared to DOAC users. That’s not a small difference. It’s the kind of risk that changes lives. A 2023 JAMA Network Open study showed that over a year, 4.14 out of every 100 warfarin users had a major bleed. That’s nearly 1 in 25 people. For many, the constant monitoring, dietary restrictions, and unpredictable reactions make warfarin feel less like medicine and more like a full-time job.
DOACs: The New Standard, With Fewer Headaches
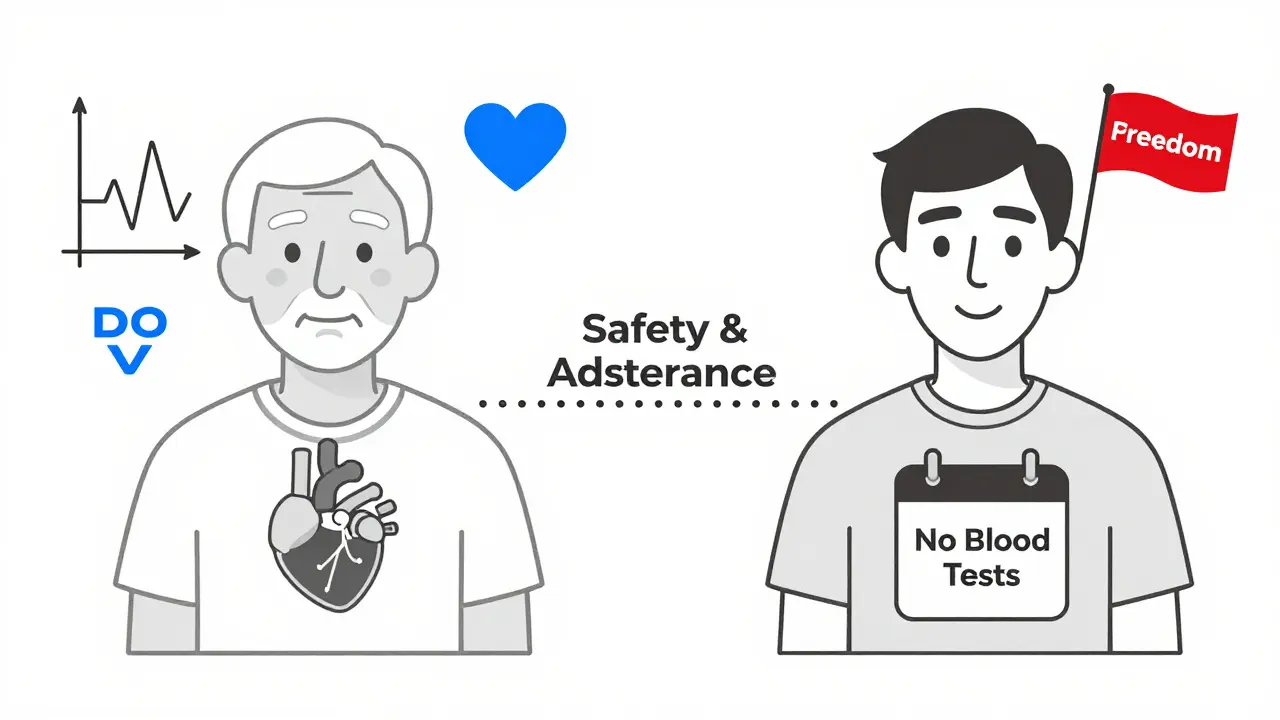
DOACs-like apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban (Savaysa)-changed the game. They don’t need routine blood tests. No INR checks. No counting vitamin K in your meals. You take a pill, once or twice a day, and that’s it. Their effects are more predictable. That’s why, as of 2023, DOACs made up 78% of all anticoagulant prescriptions in the U.S.
Each DOAC works differently. Dabigatran blocks thrombin (factor IIa). Apixaban, rivaroxaban, and edoxaban block factor Xa. That’s more targeted than warfarin’s broad vitamin K disruption. Because of this, DOACs have fewer drug interactions. You still need to watch out for some antibiotics and antifungals, but it’s nowhere near the 300+ that warfarin clashes with.
And the safety data? Strong. In atrial fibrillation, DOACs reduce stroke risk by 30% compared to warfarin. They also cut the risk of dangerous brain bleeds by half. For people with deep vein clots, DOACs lower the chance of the clot coming back by 34%. A 2024 American Heart Association study confirmed: DOACs aren’t just convenient-they’re safer.
One of the biggest wins? Adherence. A 2023 study in the American Journal of Managed Care found DOAC users were 32% more likely to stick with their medication than warfarin users. Why? No weekly blood draws. No food rules. No guessing. People just take their pill. For younger patients, that difference is even bigger-up to 41% better adherence.
When Warfarin Still Wins
DOACs aren’t perfect. And they’re not for everyone. If you have a mechanical heart valve, DOACs won’t work. They’ve been tested and failed in this group. Warfarin is still the only proven option. The same goes for people with severe kidney failure-eGFR below 15 mL/min. DOACs can build up in your system and cause dangerous bleeding. Warfarin, while still risky, is more manageable here.
Another twist: not all DOACs are the same. Apixaban has the lowest bleeding risk among them. Rivaroxaban has a higher chance of stomach bleeds. Dabigatran is better at preventing clots than rivaroxaban but has a higher risk of gastrointestinal upset. Your doctor doesn’t just pick a DOAC-they pick the right DOAC for your body.
And then there’s cost. Warfarin costs about $4 for a 30-day supply. Apixaban? Around $587. Even with insurance, copays can hit $100 or more. That’s why some patients, especially those on Medicare or without good coverage, still end up on warfarin-not because it’s better, but because they can’t afford the alternative.

Special Cases: Cancer, Kidney Disease, and Elderly Patients
If you have cancer and atrial fibrillation, apixaban is the clear winner. Studies show it reduces major bleeding by 42% compared to warfarin. Rivaroxaban? No real advantage. For kidney patients, DOACs are safer down to an eGFR of 25 mL/min. Below that, the data gets murky. Some studies say DOACs still beat warfarin in bleeding risk even in advanced kidney disease. Others warn against them. The guidelines say: if you’re on dialysis, stick with warfarin-unless your doctor has strong reasons to try a DOAC.
For older adults, DOACs are generally safer. They’re less likely to cause brain bleeds, which is a huge concern in people over 75. But dosing matters. Many DOACs have reduced-dose options for people with low body weight or kidney issues. Taking the wrong dose can be dangerous. A 2023 study found that low-dose DOACs increased stroke and death risk by 25% compared to standard doses. So if your doctor prescribes a lower dose, make sure it’s based on clear criteria-not just convenience.
What Happens If You Need Emergency Surgery?
One of the biggest fears with DOACs is: what if I have a fall and need surgery? With warfarin, you can reverse it with vitamin K or fresh frozen plasma. It’s messy, slow, and not always reliable. DOACs have specific reversal agents now. Idarucizumab (Praxbind) reverses dabigatran in minutes. Andexanet alfa (Andexxa) reverses apixaban and rivaroxaban. These aren’t magic bullets-they’re expensive and need hospital use-but they exist. Warfarin doesn’t have that luxury.
Still, most DOACs clear from your system in 12 to 24 hours. If you’re scheduled for surgery, you stop the pill a day or two before. For warfarin, you might need to stop a week early and get multiple INR checks to make sure it’s safe. That’s a big difference in planning.
Real People, Real Choices
On patient forums, the sentiment is clear. Over 80% of DOAC users say they prefer it because they don’t have to think about their diet or get blood drawn. One woman on Reddit said, “I used to carry a food log like a diary. Now I eat what I want and take my pill. It’s freedom.”
But cost is real. A man in Ohio wrote: “I’ve been on warfarin for 12 years. My copay is $5. Apixaban? $150. I can’t switch. I’d rather risk a bleed than go broke.”
And for those with mechanical valves? They’re loyal to warfarin. Not because they love the tests, but because they know it works. One patient said, “I’ve had two heart valves for 15 years. My INR’s been steady. I don’t trust the newer drugs with my life.”
The Bottom Line: What Should You Do?
If you’re starting anticoagulation for atrial fibrillation or a blood clot, DOACs are the first choice-unless you have a mechanical valve or very bad kidney function. Apixaban is often the safest bet. Rivaroxaban is fine, but watch for stomach bleeds. Dabigatran works well but can cause nausea.
If you’re already on warfarin and doing well-with steady INRs, no bleeds, and good adherence-there’s no rush to switch. But if you’re struggling with diet, tests, or interactions, talk to your doctor. Switching to a DOAC could cut your bleeding risk in half and give you back your life.
And if cost is the barrier? Ask about patient assistance programs. Many drugmakers offer free or discounted DOACs for those who qualify. Never stop your anticoagulant without talking to your doctor. Stopping suddenly can cause a clot within days.
Anticoagulants aren’t one-size-fits-all. But today, for most people, the safer, simpler choice is clear: DOACs. The future of blood thinners isn’t about old habits-it’s about smarter, safer, and more human care.



Comments
LALITA KUDIYA
DOACs changed my life 😊 no more spinach anxiety
January 6, 2026 AT 22:21
Rachel Steward
Let’s be real-DOACs aren’t ‘safer,’ they’re just marketed better. Warfarin’s been used for 70 years. DOACs? We’re still collecting long-term data. The JAMA study you cited? It’s funded by pharma. The real risk isn’t bleeding-it’s corporate greed disguised as progress. You think your INR is a burden? Try living in a country where you can’t even afford the damn pill. This isn’t medicine-it’s capitalism with a stethoscope.
And don’t get me started on ‘adherence.’ People don’t skip doses because they’re lazy-they skip because they’re drowning in bills. Apixaban costs more than my rent in some zip codes. You want safer? Fix the system first. Then maybe we’ll talk about ‘optimal anticoagulation.’
Also, ‘no dietary restrictions’? Really? Dabigatran with grapefruit juice? That’s a one-way ticket to ER. And don’t even mention NSAIDs. You think it’s easier? It’s just less visible. The bleeding still happens. It just doesn’t come with a warning label you can read.
And yes, reversal agents exist. But they cost $20,000 a dose. Who pays? You? Your insurance? The hospital? The system still fails people when they need it most. DOACs aren’t the future. They’re the same old game with a new label.
Warfarin’s a pain in the ass? Fine. But it’s a pain in the ass we understand. DOACs are a black box with a price tag. And we’re pretending that’s progress. Wake up.
January 8, 2026 AT 08:38
Emma Addison Thomas
I’ve been on warfarin for 15 years since my valve replacement. I know my INR like my own heartbeat. It’s not about convenience-it’s about reliability. I’ve seen too many younger patients switch to DOACs, then panic when they miss a dose and get dizzy. Warfarin doesn’t lie. It tells you exactly what’s happening. You learn to live with it. It’s not perfect, but it’s honest.
And yes, the blood tests are a chore-but they’re also a ritual. A moment each week where I pause, breathe, and remember I’m still alive because of this. I don’t miss the tests. I miss the silence that came before them.
January 8, 2026 AT 15:33
Alex Danner
Biggest myth: ‘DOACs don’t need monitoring.’ Wrong. They need different monitoring. Kidney function. Liver enzymes. Weight changes. Drug interactions. You just don’t get a number on a screen. You get silent, creeping risk. I’ve seen three patients on rivaroxaban bleed out because their creatinine climbed unnoticed. No INR to flag it. No doctor checking. Just… silence. Then a call from the ER.
And yes, adherence is higher-but that’s because it’s easier to forget a pill than to forget a blood test. One missed pill? No warning. One missed INR? You’re bleeding in 48 hours. That’s not freedom. That’s a gamble.
Apixaban is the best of the DOACs. No question. But don’t act like it’s risk-free. It’s just a different kind of risk. And if you’re over 75? Dose matters. A lot. I’ve seen too many ‘low-dose’ prescriptions handed out like candy. That’s not personalized care. That’s lazy.
Bottom line: DOACs are better for most. But ‘better’ doesn’t mean ‘perfect.’ And if your doctor doesn’t talk about the trade-offs, find a new one.
January 10, 2026 AT 06:15
Anthony Capunong
DOACs are a scam designed to make rich people feel better while poor people die on warfarin. This whole ‘freedom’ narrative? It’s propaganda. I’m from Ohio. My neighbor’s on warfarin because he can’t afford Eliquis. He gets his INR checked at the free clinic. He eats kale every damn day because he can’t afford lettuce. He’s alive. And you’re telling me he’s ‘not living well’ because he doesn’t have a $600 pill?
Warfarin is the great equalizer. It doesn’t care if you’re rich or poor. It just works. And if you can’t handle it? Then maybe you’re not ready for anticoagulation. Not everyone deserves to be ‘free.’ Some of us just need to survive.
January 12, 2026 AT 05:21
Katrina Morris
so i just started on apixaban last month and wow like i never realized how much mental energy i was spending on food logs and appointments like its crazy how much less stressed i am now i just take my pill and go about my day like its so simple but idk if its really safer or just less visible? like i still get scared when i cut myself now lol
January 13, 2026 AT 09:13
Paul Mason
Look, I’ve been a GP for 22 years. Warfarin? It’s a dinosaur. DOACs? They’re the future. No debate. The data’s clear. If your patient’s on warfarin and not bleeding, fine. But if they’re struggling? Switch them. Don’t wait. The risk of brain bleed is half. That’s not opinion. That’s science.
Cost? Sure, it’s high. But there are programs. I’ve gotten 14 patients free apixaban through manufacturer aid. You just have to ask. Stop making excuses. Your patient’s life matters more than your comfort with old habits.
January 13, 2026 AT 22:32
Aparna karwande
Oh please. You westerners think you’ve ‘solved’ anticoagulation with your fancy pills? In India, we’ve been managing warfarin for decades with zero labs, zero monitoring, just experience and intuition. Our doctors don’t have your $200 INR machines. We use clinical signs. Bleeding gums? Too thin. Swollen leg? Too thick. We don’t need your algorithms. We need your humility.
You call warfarin ‘archaic’? It’s the only thing keeping millions alive in the Global South. You don’t get to call it ‘burdensome’ when your country can afford reversal agents and $600 pills. Your ‘freedom’ is built on global inequality. And you’re proud of it?
DOACs? Fine for your elite. But don’t pretend your version of ‘better’ is universal. Warfarin isn’t outdated-it’s the last line of defense for the world’s poor. And you’re talking about ‘adherence’ like it’s a personal failure? It’s a systemic crime.
Next time you praise DOACs, ask yourself: who’s being left behind? Because I know who’s dying while you scroll through your pill reminders.
January 14, 2026 AT 16:33
Sai Ganesh
As someone who’s managed both warfarin and apixaban across two continents, I can say this: the real difference isn’t in the drugs-it’s in the support. In the U.S., you have apps, pharmacies, insurance reps, patient advocates. In India? You get a prescription and a prayer.
DOACs are easier only if you have infrastructure. Without it, warfarin’s complexity becomes a strength-because you’re forced to engage. You talk to your doctor. You learn. You adapt. You become part of the process.
DOACs make you passive. Warfarin makes you active. And sometimes, being active is the only thing that keeps you alive.
Don’t romanticize convenience. It’s not always safety.
January 15, 2026 AT 06:57
Ayodeji Williams
yo so i switched to xarelto last year and my grandma said ‘you’re gonna die from a bleed’ 😂 but then i went to the ER after a fall and they gave me andexxa and i was out in 2 hours lmao
warfarin people be like ‘i’ve been doing this for 20 years’ but bro i got a 1000000% better quality of life now
also i eat pizza every night and my INR is fine 😎
January 15, 2026 AT 15:33
Anastasia Novak
Let’s be honest-DOACs are just the pharmaceutical industry’s way of monetizing anxiety. You don’t need a pill to ‘feel safe.’ You need to confront mortality. Warfarin forces you to face it. Daily. INR checks are not a burden-they’re a mirror. You look at that number and you see your own fragility. That’s not a flaw. That’s wisdom.
DOACs? They’re the antidepressants of anticoagulation. You swallow a pill and pretend you’re not dying. You eat your kale. You ignore your kidneys. You assume the system will catch you if you slip. Spoiler: it won’t.
The real tragedy isn’t warfarin’s complexity. It’s that we’ve outsourced our relationship with death to a pill. And we call that progress.
January 16, 2026 AT 19:31
Jonathan Larson
As a clinician who has managed anticoagulation for over two decades, I offer this perspective: the choice between warfarin and DOACs is not a binary decision. It is a dynamic, patient-centered negotiation between risk, resources, and resilience.
DOACs represent a significant advancement in pharmacological precision, reducing intracranial hemorrhage by approximately 50% in atrial fibrillation populations. Their pharmacokinetic predictability allows for greater autonomy in daily life. Yet, their reliance on renal clearance, absence of universal reversal agents for all agents, and prohibitive cost in under-resourced settings necessitate individualized assessment.
Warfarin, despite its limitations, remains a cornerstone therapy for mechanical valve recipients and patients with end-stage renal disease on dialysis. Its reversibility, though imperfect, is clinically proven. Moreover, its low cost preserves access for vulnerable populations.
What unites both classes is not efficacy, but the imperative of vigilance. Whether through INR monitoring or periodic renal function testing, the patient’s role in self-advocacy remains non-negotiable.
The future of anticoagulation lies not in replacing one drug with another, but in expanding access to monitoring, education, and affordability across socioeconomic strata. Technology alone cannot heal. Compassion, equity, and clinical judgment must lead.
January 17, 2026 AT 07:35
steve rumsford
man i was on warfarin for 8 years and i hated it but then i switched to eliquis and now i just forget to take it sometimes and my dr said my last inr was fine?? wait no i dont even get inr anymore lol
also i ate a whole bag of spinach last week and nothing happened
doacs are the real MVP
January 19, 2026 AT 04:42
Rachel Steward
Replying to the guy who said DOACs are ‘just marketing.’ You’re right. But you’re also missing the point. The marketing isn’t the lie. The lie is pretending that warfarin’s ‘experience’ is a virtue. Experience doesn’t save lives when the data says DOACs cut brain bleeds in half. Experience doesn’t pay for a patient’s rent. Experience doesn’t stop a 72-year-old from choosing between insulin and apixaban.
So yes, the pharma ads are slick. But the numbers aren’t. And if you’re defending warfarin because it’s ‘honest,’ you’re not being noble-you’re being negligent. The truth isn’t in the old way. It’s in the better way. And the better way is here.
January 20, 2026 AT 21:49