Decongestants and Blood Pressure Medications: What You Need to Know About the Hidden Risks

- Colin Hurd
- 29 November 2025
- 13 Comments
Decongestant Safety Checker
Check if Decongestants Are Safe for You
This tool helps determine if decongestant medications might be dangerous based on your blood pressure status and health conditions.
Many people reach for decongestants when they have a cold or allergies. It’s easy - just grab a bottle from the shelf, pop a pill, and feel better in hours. But if you have high blood pressure, that simple act could be dangerous. You might not realize it, but common cold medicines like Sudafed, Advil Cold & Sinus, or even Benadryl Allergy Plus Congestion contain ingredients that can spike your blood pressure - sometimes dangerously so.
How Decongestants Raise Blood Pressure
Decongestants like pseudoephedrine and phenylephrine work by narrowing blood vessels in your nose. That reduces swelling and clears congestion. But here’s the catch: they don’t just narrow vessels in your nose. They tighten blood vessels everywhere - including those in your heart, brain, and kidneys. This increases resistance in your circulatory system, forcing your heart to pump harder. The result? Higher blood pressure.It’s not just a small bump. Studies show that pseudoephedrine can raise systolic blood pressure by 2 to 5 mm Hg on average. For someone with controlled hypertension, that might seem minor. But for someone with uncontrolled high blood pressure, or a history of heart disease, stroke, or arrhythmias, even a small rise can trigger serious events - heart attacks, strokes, or irregular heartbeats.
The FDA has known about this since at least 2005. That’s when a major meta-analysis confirmed that pseudoephedrine causes measurable, statistically significant increases in blood pressure. Since then, warning labels have been updated. But many people still don’t read them.
Which Decongestants Are the Biggest Risk?
Not all decongestants are created equal. The two most common ones are:- Pseudoephedrine - Found in Sudafed, Claritin-D, Zyrtec-D, and many multi-symptom cold medicines. This is the most studied and most potent in raising blood pressure. It’s sold behind the pharmacy counter in the U.S. because of its link to methamphetamine production - but also because of its cardiovascular risks.
- Phenylephrine - Now the most common decongestant in OTC products after pseudoephedrine was restricted. Many assume it’s safer. But recent studies show it still raises blood pressure, especially in higher doses or with repeated use. A case report in US Pharmacist documented a 5-year-old girl whose blood pressure climbed to 135/80 after taking phenylephrine for four days. Her pressure returned to normal once she stopped.
Other decongestants like ephedrine, naphazoline, and oxymetazoline (found in nasal sprays like Afrin) carry similar risks. Even nasal sprays can be absorbed into the bloodstream and affect your heart.
Who’s at the Highest Risk?
Not everyone with high blood pressure will have a bad reaction. But certain people are far more vulnerable:- Those with uncontrolled hypertension - Blood pressure consistently above 140/90
- People with heart disease, including past heart attacks or heart failure
- Those with arrhythmias or a history of irregular heartbeat
- Patients with Prinzmetal angina (variant angina) - a rare type of chest pain caused by artery spasms
- Anyone taking MAO inhibitors like Nardil or Marplan - combining these with decongestants can cause a life-threatening spike in blood pressure
- Older adults on multiple medications - more chances for dangerous interactions
Research suggests that 5-10% of hypertensive patients experience marked increases in blood pressure after taking decongestants. That’s not a small number. And many don’t even realize they’re at risk until it’s too late.
Hidden in Plain Sight: Multi-Symptom Medicines
This is where most people get caught.You think you’re just taking something for a sore throat. But look closer. Tylenol Cold & Flu. Advil Multi-Symptom Cold & Flu. Mucinex Sinus Max. Benadryl Allergy Plus Congestion. These all contain decongestants. So do many nighttime cold remedies, allergy tablets, and sinus relief formulas.
Most consumers don’t check the active ingredients. They see “cold medicine” and assume it’s safe. But if you have high blood pressure, you need to read the label like a pharmacist. Look for these words:
- Pseudoephedrine
- Phenylephrine
- Ephedrine
- Naphazoline
- Oxymetazoline
And don’t forget sodium. Some liquid cold medicines use sodium as a preservative. A single dose can contain over 200 mg of sodium - enough to raise blood pressure in salt-sensitive individuals.
What Should You Do Instead?
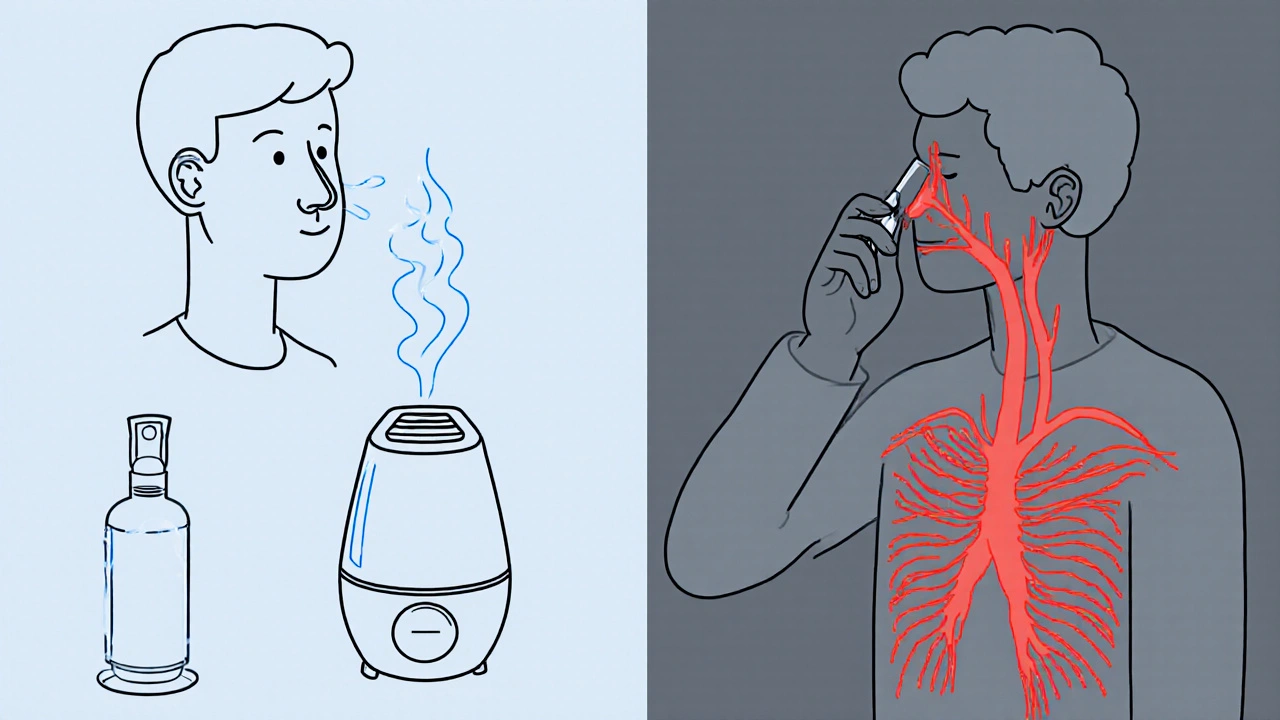
You don’t have to suffer through congestion. There are safer options:- Saline nasal spray - Flushes out mucus without any drugs. Safe for daily use.
- Steam inhalation - Breathe in warm, moist air from a bowl or shower. Helps loosen congestion naturally.
- Humidifiers - Keep the air moist, especially at night. Reduces nasal dryness and swelling.
- Antihistamines without decongestants - Like plain loratadine (Claritin) or cetirizine (Zyrtec). These help with allergy-related congestion but don’t raise blood pressure.
- Elevating your head - Sleep with an extra pillow. Reduces nighttime congestion.
Some people turn to herbal remedies like ephedra or bitter orange - but these can be even riskier. They contain natural stimulants that act just like synthetic decongestants. Avoid them.

When You Must Use a Decongestant
Sometimes, you have no choice. Maybe your sinuses are completely blocked, or you’re in severe discomfort. If you have well-controlled high blood pressure and your doctor says it’s okay, here’s how to do it safely:- Use the lowest effective dose - Start with half a tablet if possible.
- Choose extended-release over immediate-release - It’s absorbed slower, causing less of a spike.
- Take it only once a day - Never exceed the label’s instructions.
- Monitor your blood pressure - Check it before and 2-4 hours after taking the medication. If it rises more than 10-15 mm Hg, stop and call your doctor.
- Don’t use it for more than 3 days - Prolonged use increases risk and can cause rebound congestion.
And always - always - talk to your pharmacist before buying. They’re trained to spot these risks. In the U.S., pseudoephedrine is behind the counter for a reason. Use that moment. Ask: “Is this safe for someone with high blood pressure?”
The Bigger Picture: Why This Keeps Happening
Despite decades of warnings, about 15% of hypertensive patients still take decongestants without medical advice. Why?Because they don’t know what’s in the medicine. Because the label says “for colds” and they assume it’s harmless. Because they’ve taken it before and felt fine - so they think it’s safe again.
But high blood pressure isn’t always obvious. You might feel fine, but your arteries are under stress. A decongestant can be the trigger that pushes you over the edge.
Pharmacists report spending 3-5 minutes per customer during cold season just explaining these risks. The American Heart Association launched a “Medication Check-Up” campaign in 2022 because they know this is a silent, widespread problem. Just because it’s over-the-counter doesn’t mean it’s safe for everyone.
Final Advice: Know Your Meds, Know Your Body
If you have high blood pressure:- Read every OTC label - even if you’ve used it before.
- Keep a list of all your medications - including vitamins and supplements - and review it with your doctor every 6 months.
- When in doubt, skip it. Use saline, steam, or a humidifier instead.
- Ask your pharmacist. They’re your best defense against hidden risks.
- Don’t assume “natural” or “herbal” means safe. Some of the most dangerous stimulants come from plants.
Your blood pressure is a silent indicator of your heart’s health. Don’t let a cold medicine put it at risk. A few days of discomfort are better than a trip to the ER.
Can I take pseudoephedrine if my blood pressure is controlled?
It’s not recommended without medical approval. Even if your blood pressure is controlled, pseudoephedrine can still cause spikes. If your doctor says it’s okay, use the lowest dose, take it once daily, and monitor your blood pressure closely. Never use it for more than 3 days.
Is phenylephrine safer than pseudoephedrine?
Not really. While phenylephrine is less potent than pseudoephedrine, recent studies show it still raises blood pressure - especially in higher doses or with repeated use. Many people think it’s a safe replacement, but it’s not. Both should be avoided if you have high blood pressure.
What cold medicines are safe for high blood pressure?
Look for products labeled “for high blood pressure” or those that contain only one active ingredient - like plain acetaminophen for pain or antihistamines like loratadine for allergies. Avoid anything with “D,” “Sinus,” “Congestion,” or “Multi-Symptom.” Saline sprays, steam, and humidifiers are the safest options.
Can decongestants cause a stroke?
Yes. There are documented cases of strokes and heart attacks linked to decongestant use in people with uncontrolled high blood pressure or heart disease. The vasoconstriction caused by these drugs can trigger clots or burst weakened blood vessels. The risk is low for most, but not zero - especially in vulnerable individuals.
Do nasal sprays like Afrin raise blood pressure?
Yes. Oxymetazoline, the active ingredient in Afrin, is absorbed into the bloodstream. Even though it’s applied locally, it can still cause increases in blood pressure and heart rate. Use it for no more than 3 days and avoid if you have hypertension.
What should I do if my blood pressure spikes after taking a decongestant?
Stop taking the medication immediately. Rest and check your blood pressure again in 30 minutes. If it stays high (above 180/120) or you feel chest pain, dizziness, or shortness of breath, seek emergency care. Even if you feel fine, call your doctor - you may need to adjust your blood pressure meds.



Comments
LINDA PUSPITASARI
Just took Sudafed last week for my sinus thing and felt like my heart was gonna explode 😵💫
Turns out I didn't even know it had pseudoephedrine. Lesson learned. Now I read labels like I'm decoding a spy novel. Stay safe out there folks.
November 30, 2025 AT 14:17
gerardo beaudoin
Phenylephrine isn't safer. I used to think it was. Turns out it's just the new fake safe option. My dad had a spike after using it for three days. Scary stuff.
November 30, 2025 AT 14:29
tushar makwana
in india we just use steam and salt water. no pills. no stress. body knows how to heal if we let it. 🙏
December 1, 2025 AT 22:19
Richard Thomas
It is both lamentable and profoundly concerning that the pharmaceutical industry continues to market compounds with well-documented cardiovascular risks as benign over-the-counter remedies, particularly when the causal mechanisms are not only understood but have been peer-reviewed for nearly two decades. The absence of mandatory consumer education initiatives constitutes a systemic failure in public health governance.
December 2, 2025 AT 16:47
Sara Shumaker
I used to think 'natural' meant safe. Then I learned ephedra is a plant. And it can kill. We need to stop romanticizing 'natural' remedies like they're magic. Nature doesn't care if you have high blood pressure. It just does what it does.
Maybe the real problem isn't the medicine-it's how we think about medicine.
December 3, 2025 AT 07:24
Scott Collard
You're all missing the point. The FDA doesn't care. They're paid off. This is why you die quietly.
December 4, 2025 AT 10:45
Robert Bashaw
I took that Sudafed like it was candy. Felt like my head was in a vice. Heart pounding like a bass drum at a rave. I thought I was having a panic attack. Turns out? My blood pressure was doing the Macarena. Never again. Now I carry a little note in my wallet: 'NO D. NO SINUS. NO LIES.' 💥
December 5, 2025 AT 10:59
Bernie Terrien
Decongestants are just slow-motion poison for hypertensives. The fact that you can buy them next to candy is a crime.
December 5, 2025 AT 11:31
Jennifer Wang
Per the American Heart Association guidelines, individuals with hypertension should avoid sympathomimetic amines, including pseudoephedrine and phenylephrine, due to their alpha-adrenergic agonist properties, which may precipitate hypertensive crises. Non-pharmacologic interventions are strongly recommended as first-line therapy. Consultation with a licensed pharmacist is advised prior to initiating any OTC agent.
December 7, 2025 AT 07:58
stephen idiado
Everyone's overreacting. It's just a cold. Take the pill. Stop being weak. Your blood pressure isn't that bad. You're just scared of medicine.
December 9, 2025 AT 05:21
Subhash Singh
While the physiological mechanism of vasoconstriction is well established, the clinical significance of minor systolic elevation in normotensive individuals remains debatable. Furthermore, pharmacokinetic variability across populations necessitates individualized risk assessment rather than blanket contraindications.
December 11, 2025 AT 02:49
Geoff Heredia
They put this in OTC meds because they want us to get sick. The CDC and Big Pharma are in cahoots. They make billions off ER visits. You think they want you to heal? Nah. They want you to buy more pills. And that nasal spray? It's laced with tracking chips. I checked the ingredients. 'Oxymetazoline' - sounds like a code word.
December 11, 2025 AT 23:34
Tina Dinh
YESSSSS this needs to be shouted from the rooftops!! 🙌 I used to take that stuff like it was gum. Now I use saline spray, humidifier, and sleep with 3 pillows like a queen 👑 Stay healthy, my people!
December 12, 2025 AT 10:46