Dexamethasone Use During Pregnancy: Risks, Benefits, and Guidelines
- Colin Hurd
- 24 October 2025
- 14 Comments
Expecting a baby brings a flood of questions about what’s safe to take. Among the many medicines that surface in prenatal discussions, dexamethasone often raises the loudest alarm because it’s a powerful steroid. Below you’ll find a clear, no‑nonsense guide that explains when the drug might be helpful, what the real‑world risks are, and how doctors decide whether to prescribe it during pregnancy.
Quick Takeaways
- Dexamethasone is a synthetic glucocorticoid used for inflammation, immune suppression, and fetal lung maturation.
- In the first trimester the drug is linked to a higher chance of certain birth defects; many clinicians avoid it unless absolutely necessary.
- During the third trimester, short‑course use can accelerate fetal lung development and reduce newborn respiratory distress.
- Maternal conditions such as severe asthma, autoimmune disease, or threatened preterm labor are common reasons for prescription.
- Always discuss dosage, timing, and alternatives with your obstetrician; a tailored plan minimizes risk to you and your baby.
What Is Dexamethasone?
Dexamethasone is a synthetic glucocorticoid that mimics the body’s natural cortisol. It is prescribed to shrink inflammation, suppress an overactive immune system, and, in specific obstetric scenarios, speed up fetal lung maturation. First approved in the 1960s, the drug has become a staple in hospitals worldwide because it works quickly and stays active in the body longer than many other steroids.
Why Pregnancy Changes the Equation
Pregnancy isn’t just a bigger version of the non‑pregnant body; the placenta, hormone shifts, and fetal development stage all affect how a medication behaves. When a drug crosses the placenta, it can interact with the developing organs, which are especially sensitive during the first 12 weeks (the organogenesis period). Later in pregnancy, the same drug might be beneficial-for example, helping the baby’s lungs get ready for life outside the womb.
Key Pregnancy Stages and Dexamethasone Safety
| Trimester | Typical Indications | Potential Benefits | Known Risks |
|---|---|---|---|
| First (0‑12 weeks) | Severe autoimmune flare, uncontrolled asthma | Rapid symptom control | Increased odds of oral clefts, limb reduction defects; FDA Category C |
| Second (13‑27 weeks) | Maternal hypertension, refractory eczema | Limited evidence of benefit | Possible growth restriction, altered fetal adrenal function |
| Third (28‑40 weeks) | Risk of preterm birth, fetal lung immaturity | Accelerates surfactant production, lowers neonatal respiratory distress syndrome (RDS) rates | Transient fetal heart rate changes, maternal hyperglycaemia |
When Doctors Actually Prescribe It
Here are the three most common scenarios you’ll hear about:
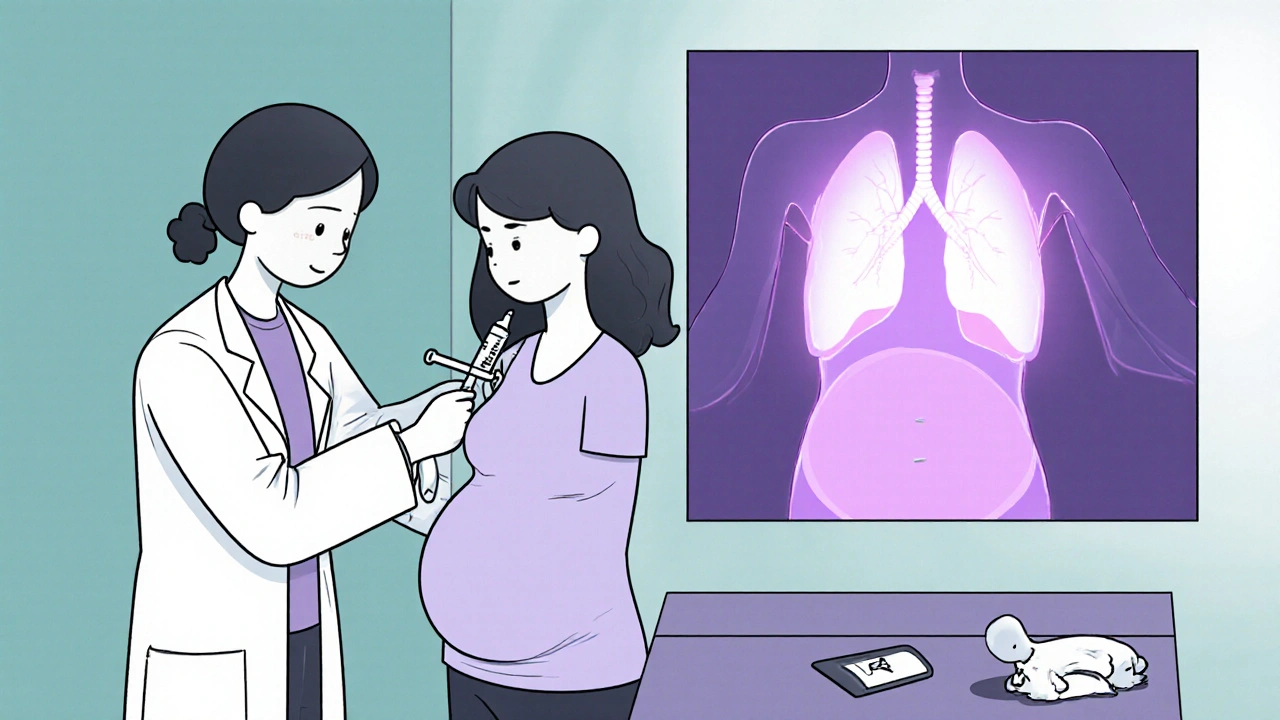
- Preterm labor risk: If your doctor thinks you might deliver before 34 weeks, a short course of dexamethasone (usually 6 mg intramuscularly every 12 hours for two doses) is given to the mother. The goal is to boost the baby’s surfactant production, which dramatically cuts the chance of RDS.
- Congenital adrenal hyperplasia (CAH) screening: Pregnant women carrying a fetus at risk for CAH may be offered dexamethasone early in pregnancy to suppress excess androgen production, preventing ambiguous genitalia. This use is controversial and only recommended in specialized centres with strict monitoring.
- Severe maternal disease: Uncontrolled asthma, lupus flares, or inflammatory bowel disease can threaten both mother and baby. In such cases, the benefit of stabilising the mother often outweighs potential fetal risks, especially if treatment starts after organogenesis.
How the Drug Gets to the Baby
The placenta isn’t a perfect barrier. Dexamethasone is a small, lipophilic molecule, so it crosses readily. Once in the fetal circulation, it binds to the glucocorticoid receptor, influencing gene expression that drives lung cell maturation. However, the same pathway can dim down growth signals in other organs, which explains why high doses early on may affect limb formation.
Maternal Side Effects to Watch
While the focus is often on the baby, the mother can experience classic glucocorticoid effects:
- Elevated blood sugar - a concern for women with gestational diabetes or a family history of diabetes.
- Increased blood pressure - can aggravate pregnancy‑induced hypertension.
- Sleep disruption and mood swings - especially with higher or prolonged dosing.
- Potential for infection - steroids suppress immune response, so doctors may prescribe prophylactic antibiotics if the dose is high.

Alternatives and When to Say No
If you’re in the first trimester and your condition isn’t life‑threatening, doctors often switch to other options. For asthma, inhaled corticosteroids or leukotriene modifiers pose far less risk. For autoimmune flares, hydroxychloroquine or azathioprine may be safer long‑term choices. The key is a shared decision‑making process: understand the exact risk magnitude, explore safer meds, and set a clear monitoring plan.
Practical Tips for Expecting Mothers on Dexamethasone
- Track dosage precisely: Keep a written log of each injection or tablet, including time and amount.
- Monitor blood sugar: If you’re diabetic, check levels more often for 48 hours after a dose.
- Stay hydrated: Steroids can cause fluid retention; sipping water helps mitigate swelling.
- Watch fetal movements: Any sudden drop should prompt a call to your obstetrician.
- Plan follow‑up ultrasounds: Your doctor may schedule growth scans to ensure the baby is developing normally.
Frequently Asked Questions
Can dexamethasone cause birth defects?
Evidence shows a modest increase in oral clefts and limb reduction defects when the drug is taken in the first trimester. That’s why clinicians reserve it for severe maternal conditions or for specific fetal therapies carried out in specialist centres.
Why is dexamethasone used to prevent newborn breathing problems?
A short course given after 28 weeks stimulates surfactant production in the fetal lungs. Surfactant keeps the air sacs from collapsing, so babies born early have a much lower risk of respiratory distress syndrome.
Is it safe to breastfeed while on dexamethasone?
Small amounts pass into breast milk, but most studies show no adverse effects on infants when the mother takes typical doses. Still, discuss timing of feeds with your doctor to minimize exposure.
What monitoring does my doctor need to do?
Blood pressure and glucose checks are standard. If you’re on a prolonged course, the doctor may order liver function tests and a fetal growth ultrasound to watch for any growth restriction.
Can I refuse dexamethasone if I’m pregnant?
Absolutely. You have the right to decline any medication. Your doctor should then discuss alternative treatments and the potential consequences of not treating the underlying condition.
Bottom Line
In a nutshell, dexamethasone is a double‑edged sword in pregnancy. Early‑trimester exposure carries a measurable teratogenic risk, while a brief, carefully timed course in the third trimester can be a lifesaver for a pre‑term baby. The safest path is a personalized plan that weighs maternal health needs against fetal vulnerability, with close monitoring at every step.



Comments
Ekeh Lynda
Dexamethasone is a powerful synthetic glucocorticoid with a complex risk profile in pregnancy. The drug’s ability to cross the placenta means fetal exposure is inevitable when administered to the mother. In the first trimester the literature documents a modest increase in oral clefts and limb reduction anomalies. This association stems from glucocorticoid mediated interference with embryonic growth signaling pathways. Later in gestation the same mechanism accelerates surfactant production in the fetal lungs. Consequently a short course after 28 weeks can dramatically lower neonatal respiratory distress syndrome rates. However the timing of administration must be meticulously calibrated to avoid unnecessary exposure. Maternal conditions such as severe asthma or lupus often justify the trade off between benefit and fetal risk. When those diseases are uncontrolled the health of the mother outweighs potential teratogenic effects. Physicians therefore rely on a risk benefit matrix that incorporates dosage gestational age and alternative therapies. For example inhaled corticosteroids may control asthma with far less systemic absorption. Likewise hydroxychloroquine offers a steroid sparing option for many autoimmune flares. When no viable alternative exists the dosing schedule is limited to six milligrams every twelve hours for two doses. Monitoring protocols include frequent blood pressure checks glucose surveillance and fetal growth ultrasounds. In summary the decision to use dexamethasone demands a personalized plan that balances maternal wellbeing against fetal vulnerability.
October 24, 2025 AT 16:26
Dawn Bengel
This steroid is a danger to our future generations 🇺🇸💥
November 2, 2025 AT 13:43
junior garcia
Dexamethasone can save a baby’s breath. But it can also scar a tiny hand. Choose wisely.
November 11, 2025 AT 12:00
Dason Avery
When used at the right moment it turns a scary preterm birth into a hopeful story 😊. Doctors have the power to time it perfectly!
November 20, 2025 AT 10:17
Kester Strahan
The PK/PD profile of dexamethasone indicates a high Vd and low clearance in pregnant pts. However the placental transfer coefficent is off the charts making fetal exposure unavoidable. Clinicians should weigh the teratog risk vs the surfactant boost like a cost‑benefit analysis. In practice we often see dose‑adjustments based on maternal cortisol baselines.
November 29, 2025 AT 08:34
Doreen Collins
You’ve broken down the science nicely and it helps a lot. Remember to keep a log of each injection and check your sugars after each dose. And never hesitate to call your OB if you notice any changes in fetal movement.
December 8, 2025 AT 06:51
HILDA GONZALEZ SARAVIA
Dexamethasone’s role in fetal lung maturation is well established and backed by large randomized trials. The typical regimen is 6 mg IM every 12 hours for two doses, administered after 28 weeks gestation. This short burst increases surfactant protein expression and cuts the incidence of respiratory distress syndrome by up to 50 percent. Side effects for the mother include transient hyperglycaemia and a modest rise in blood pressure, which should be monitored. For the fetus the main concerns are limited to the early‑trimester exposure window, where the teratogenic signal is strongest.
December 17, 2025 AT 05:09
Lindy Hadebe
Another glorified steroid with a checklist of risks that nobody reads.
December 26, 2025 AT 03:26
Tammy Watkins
The decision matrix for dexamethasone must integrate maternal disease severity, gestational age, and the availability of alternative therapies. In cases of imminent pre‑term labor the evidence supports a brief, well‑timed course to enhance neonatal outcomes. It is incumbent upon the obstetrician to discuss these nuances with the patient, outlining both potential benefits and documented risks. By fostering an informed dialogue we empower expectant mothers to participate actively in their care.
January 4, 2026 AT 01:43
Casey Morris
Ah, dexamethasone, that venerable glucocorticoid, a true double‑edged sword; its pharmacodynamics are as fascinating as they are formidable, and yet, one must not overlook the ethical dimensions of its prenatal use, especially when the stakes involve both maternal well‑being and fetal integrity, a delicate ballet of risk and reward, undeniably worthy of rigorous discourse.
January 13, 2026 AT 00:00
Teya Arisa
Your eloquent portrayal captures the complexity perfectly, and I wholeheartedly agree that a balanced approach is essential 😊. Continuous glucose monitoring and blood pressure surveillance should be instituted promptly, and multidisciplinary collaboration will ensure optimal outcomes.
January 21, 2026 AT 22:17
Carla Taylor
Dexamethasone can be a lifesaver when used right and it’s cool that doctors have that tool.
January 30, 2026 AT 20:34
Kathryn Rude
Life is a series of choices and dexamethasone sits at a crossroads of survival and risk :) the moral calculus shifts with each trimester and each condition the mother faces. We must weigh the immediate breath of a newborn against the silent echo of a possible defect. In the end the true hero is informed consent.
February 8, 2026 AT 18:51
Mary Mundane
If you’re not desperate, avoid the steroid.
February 17, 2026 AT 17:09