Drug-Induced Liver Injury: High-Risk Medications and How to Monitor Them
- Colin Hurd
- 3 December 2025
- 13 Comments
Every year, thousands of people end up in the hospital not because of a virus or bad diet, but because of a medication they were told was safe. Drug-induced liver injury, or DILI, is one of the most dangerous but overlooked side effects of common drugs. It doesn’t always show up in routine checkups. It doesn’t always come with obvious symptoms. But when it hits, it can shut down your liver - fast.
What Is Drug-Induced Liver Injury?
DILI happens when a medication, supplement, or even a herbal product damages your liver. It’s not the same as liver damage from alcohol or hepatitis. This is caused by something you took on purpose - a pill you swallowed to feel better. The liver is built to process drugs, but sometimes it gets overwhelmed. The toxic byproducts build up, trigger an immune response, or directly kill liver cells.
There are two main types: intrinsic and idiosyncratic. Intrinsic DILI is predictable. Take too much acetaminophen, and your liver will fail - no matter who you are. Idiosyncratic DILI is the sneaky kind. It strikes without warning, even at normal doses. One person takes the same antibiotic as another and walks away fine. The other ends up in the ICU. There’s no way to know who’s at risk until it’s too late.
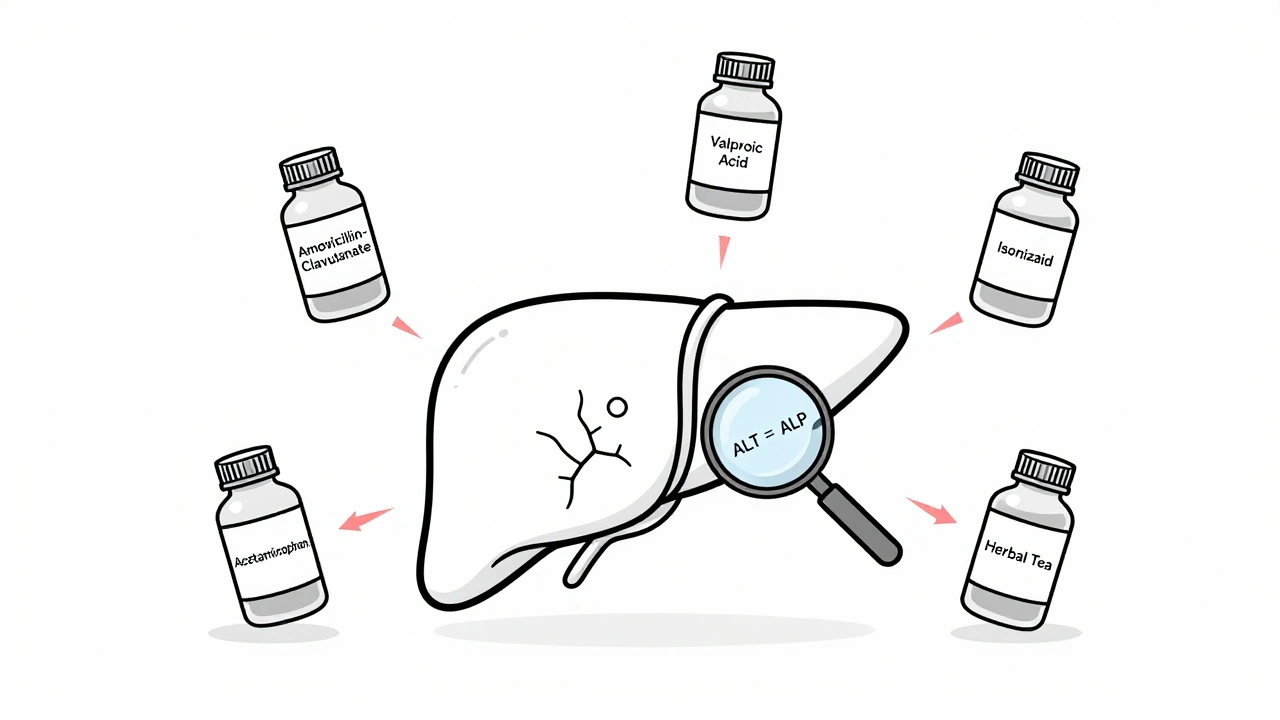
Top 5 High-Risk Medications
Not all drugs are created equal when it comes to liver damage. Some are far more dangerous than others. Here are the biggest culprits based on real-world data from U.S. and European registries.
- Acetaminophen - This is the #1 cause of acute liver failure in the U.S. Even a single overdose of 7-10 grams can be deadly. But here’s the twist: you don’t have to take it all at once. Taking 4 grams a day for several days - especially if you drink alcohol or have liver disease - can build up to toxic levels. The FDA recommends no more than 3 grams daily for older adults or those with liver issues.
- Amoxicillin-clavulanate - This common antibiotic for sinus infections and pneumonia causes about 14% of all idiosyncratic DILI cases. It doesn’t hurt everyone, but when it does, the damage can be severe. Symptoms like yellow skin, dark urine, and itching often appear 1-6 weeks after starting the drug.
- Valproic acid - Used for seizures and bipolar disorder, this drug can cause liver failure, especially in children under 2. The risk jumps to 10-20% in kids on multiple seizure meds. Adults aren’t safe either - liver enzymes can spike without warning.
- Isoniazid - A key drug for tuberculosis, isoniazid causes liver injury in about 1% of users. For people over 35, that risk doubles. It’s silent at first - no pain, no nausea. Then ALT levels climb to over 1,000 (normal is under 40). Recovery can take six months or more.
- Herbal and dietary supplements - This group has exploded in recent years. Green tea extract, kava, anabolic steroids, and weight-loss pills now cause 20% of DILI cases in the U.S. - up from 7% in 2004. These aren’t regulated like drugs. Labels lie. Ingredients are hidden. One woman developed liver failure after taking a "natural" weight-loss tea that contained unlisted pyrrolizidine alkaloids.
How Doctors Diagnose DILI
There’s no single test for DILI. It’s a diagnosis of exclusion. That means your doctor has to rule out everything else first - hepatitis A, B, or C; autoimmune liver disease; fatty liver; gallstones.
The first clue? Blood work. Two key numbers matter:
- ALT (alanine aminotransferase) - If it’s more than 3 times the upper limit of normal, your liver is under stress.
- ALP (alkaline phosphatase) - If this is more than 2 times normal, bile flow is blocked.
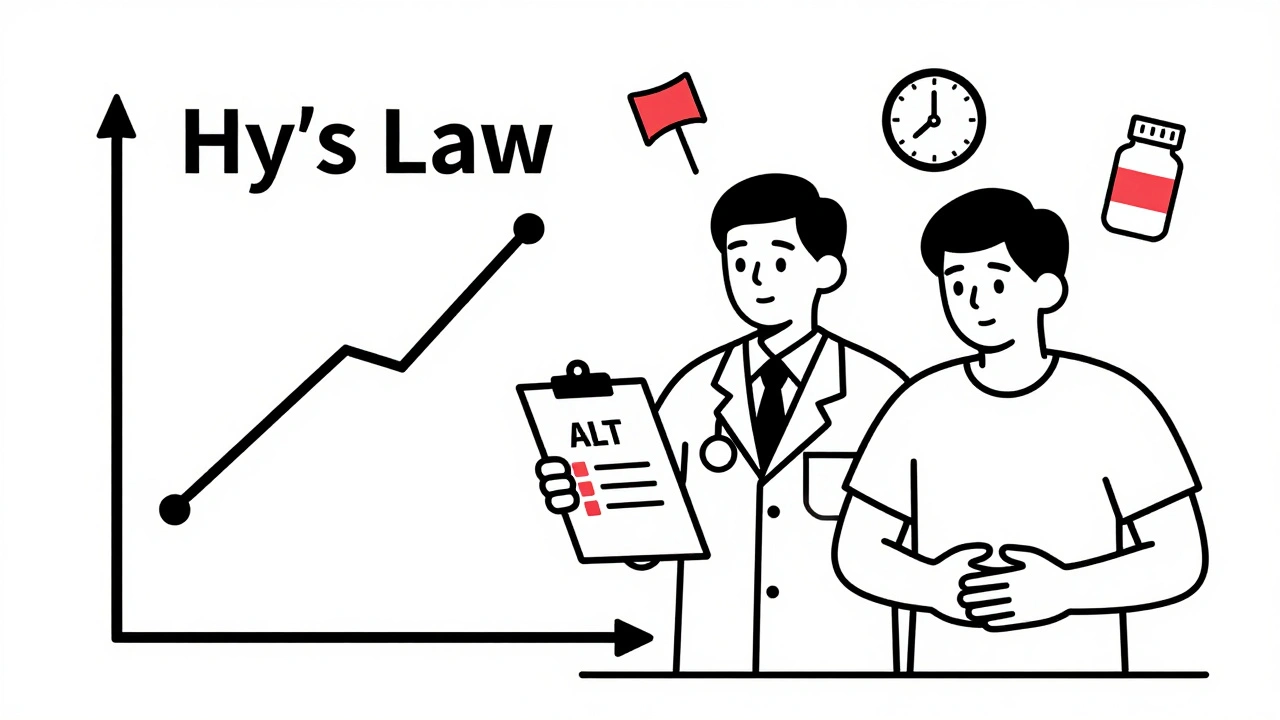
The pattern tells the story. High ALT? That’s hepatocellular injury - like with acetaminophen. High ALP? That’s cholestatic injury - think amoxicillin-clavulanate. But the real red flag is Hy’s Law: if your ALT or AST is over 3x ULN and your bilirubin is over 2x ULN, you have a 10-50% chance of developing acute liver failure. This rule has saved lives since 1978.
Doctors use the RUCAM scale to score how likely the drug caused the injury. A score of 8 or higher means "highly probable." Below 3? "Unlikely." This isn’t perfect - but it’s the best tool we have.
Who Should Be Monitored - and How
You don’t need to test everyone on every drug. But for high-risk medications, monitoring isn’t optional - it’s life-saving.
Isoniazid (for TB): Get liver tests before starting. Then monthly for the first 3 months. If you’re over 35, get tested every 2 weeks. Stop the drug if ALT rises above 3-5x normal, or if you feel nauseous, tired, or your skin turns yellow.
Valproic acid: Check liver enzymes before starting, at 2 weeks, then every 3 months. If you’re a child under 2, monitor even more closely. Watch for vomiting, confusion, or extreme sleepiness - signs of hyperammonemia, not just liver damage.
Statins: Routine monitoring isn’t recommended. The risk of serious injury is 1 in 100,000. But if you’re on multiple drugs, have liver disease, or drink alcohol, get baseline tests. Report muscle pain or dark urine immediately - those can be early signs.
Antibiotics like amoxicillin-clavulanate: No routine testing is standard - but if you’re on it for more than 2 weeks, ask your doctor about a follow-up ALT test. Most DILI cases show up between weeks 2 and 8.
Pharmacists play a big role here. A study showed that when pharmacists review all your meds - including supplements - they catch dangerous interactions before they happen. One patient avoided liver failure because their pharmacist spotted the conflict between their new antibiotic and seizure medication.
What Happens After Diagnosis?
Step one: Stop the drug. That’s it. That’s the most important thing. In 90% of cases, liver enzymes start dropping within 1-2 weeks after stopping the culprit.
For acetaminophen overdose, time is everything. If you take N-acetylcysteine (NAC) within 8 hours, you have a 100% chance of avoiding liver damage. After 16 hours, that drops to 40%. The Rumack-Matthew nomogram - a chart doctors use - tells them exactly when to give NAC based on your blood level.
For other types of DILI, there’s no antidote. Supportive care is all you get - fluids, rest, avoiding alcohol and other liver stressors. Steroids? Sometimes used in autoimmune-like cases, but evidence is weak. Liver transplant? Needed in about 13% of DILI cases that lead to acute failure.
Recovery takes time. Most people recover fully in 3-6 months. But 12% end up with permanent liver damage. One Reddit user took 10 months to feel normal again after isoniazid. Another waited 3 months for the itching from amoxicillin-clavulanate to go away.

What You Can Do - Before You Take the Pill
You can’t control everything. But you can control how you approach your meds.
- Know your risk. If you’re over 35, have liver disease, drink alcohol, or take multiple drugs, you’re at higher risk.
- Ask your doctor: "Is this drug known to affect the liver? Do I need blood tests?" Don’t assume it’s safe just because it’s prescription.
- Track your supplements. Just because it says "natural" doesn’t mean it’s safe. Keep a list of everything you take - vitamins, herbs, weight-loss pills - and show it to your doctor and pharmacist.
- Watch for symptoms. Fatigue, nausea, dark urine, yellow eyes, itchy skin, or abdominal pain? Don’t wait. Get checked.
- Don’t mix alcohol with acetaminophen. Even one drink a day with regular Tylenol use increases your risk.
- Use one pharmacy. They can flag dangerous combinations across all your prescriptions and supplements.
What’s New in DILI Research
Science is catching up. In 2021, researchers found that certain genes make some people far more likely to develop DILI. If you carry HLA-B*57:01, flucloxacillin could destroy your liver. HLA-DRB1*15:01? Amoxicillin-clavulanate becomes dangerous. Genetic testing before prescribing is now being tested in high-risk groups.
New blood tests are coming. MicroRNA-122 rises within hours of liver damage - way before ALT. Keratin-18 shows if liver cells are dying. These could let doctors catch DILI days earlier.
Hospitals are starting to use electronic alerts. If your EHR sees you’re prescribed isoniazid and you’re over 50, it pops up: "Consider baseline liver test." Early data shows this prevents 15-20% of severe cases.
And the FDA now requires drug makers to test for mitochondrial toxicity - the hidden killer behind drugs like troglitazone and fialuridine that once wiped out patients. If a drug looks too similar to those, it gets flagged before it even hits shelves.
Can over-the-counter painkillers cause liver damage?
Yes. Acetaminophen (Tylenol) is the leading cause of acute liver failure in the U.S. Taking more than 3 grams a day - especially if you drink alcohol or have liver disease - can cause serious damage. Even normal doses can be risky if taken daily for weeks. Never combine multiple products that contain acetaminophen - cold meds, sleep aids, and pain relievers often include it.
Are herbal supplements safer than prescription drugs for the liver?
No. Herbal and dietary supplements now cause about 20% of all drug-induced liver injury cases in the U.S. Products like green tea extract, kava, and weight-loss pills are not regulated like drugs, so their ingredients can be inconsistent or contaminated. Many contain hidden toxins that aren’t listed on the label. Natural doesn’t mean safe.
How long does it take to recover from drug-induced liver injury?
Most people recover fully in 3 to 6 months after stopping the drug. But recovery depends on how much damage was done. Some patients see liver enzymes return to normal in weeks. Others take up to a year. About 12% of cases result in permanent liver damage. Early detection and stopping the drug immediately improve outcomes dramatically.
Should I get liver tests before starting a new medication?
It depends on the drug. For high-risk medications like isoniazid, valproic acid, or certain antibiotics, baseline liver tests are standard. For statins or most other drugs, routine testing isn’t needed unless you have risk factors like age over 35, alcohol use, or existing liver disease. Always ask your doctor: "Is this drug linked to liver injury? Should I get tested?"
Can DILI happen even if I’ve taken the drug before without problems?
Yes. This is the most dangerous part of idiosyncratic DILI. You can take amoxicillin-clavulanate or valproic acid for months or years with no issues - then suddenly, your liver reacts. There’s no way to predict who will develop it. That’s why monitoring and awareness are critical, even if you’ve used the drug safely in the past.
Final Thought: Don’t Assume Safety
Medications save lives. But they can also break your liver - silently, suddenly, and without warning. The key isn’t avoiding all drugs. It’s being informed. Ask questions. Know your risks. Track your supplements. Get tested when needed. Your liver doesn’t scream when it’s hurt. It whispers. Listen before it’s too late.

Comments
Michael Feldstein
Just had a patient on isoniazid for TB last month - turned out she was also taking green tea extract for "weight loss." ALT hit 1800. She recovered after stopping both, but it was terrifying. This post nails it: supplements aren't harmless. Always ask about everything, even that "natural" tea your aunt swears by.
December 4, 2025 AT 22:44
Carolyn Ford
Of course the FDA doesn’t regulate supplements - because they’re too busy protecting Big Pharma’s profits. You think they want you to know that 20% of liver failures come from "natural" products? No. They’d rather you keep buying those "detox" powders while they cash in on transplants.
December 6, 2025 AT 10:24
Rebecca Braatz
If you're on any of these meds - especially if you're over 35 or on multiple prescriptions - don't wait for symptoms. Get your liver enzymes checked before you start. It’s a 10-minute blood test. It could save your life. Seriously. Do it. Your future self will thank you.
December 6, 2025 AT 17:57
jagdish kumar
The liver is a silent god. We feed it poison, and it forgives. Until it doesn’t.
December 8, 2025 AT 07:23
Rachel Bonaparte
Let me tell you something they don’t want you to know - the whole DILI narrative is engineered. Big Pharma knows acetaminophen is a ticking time bomb, but they’ve spent millions lobbying to keep it OTC. They even funded studies that downplayed the risk. And don’t get me started on how they bury the genetic markers - HLA-B*57:01? That’s a death sentence if you’re prescribed flucloxacillin. They’ve known since 2008. But you? You’re still buying Tylenol at the gas station like it’s candy.
December 9, 2025 AT 06:45
zac grant
Hy’s Law still holds up like a champ - ALT >3x ULN + bilirubin >2x ULN = red alert. That’s the golden combo for predicting acute liver failure. I use it in my clinic every week. The RUCAM scale? Messy, but it’s the only structured tool we’ve got. Pro tip: if someone’s on valproic acid and has a history of epilepsy + polypharmacy, monitor every 2 weeks, not quarterly. That’s where the real danger zone is.
December 9, 2025 AT 12:07
Jenny Rogers
It is, without a doubt, a profound ethical failure of modern pharmacology that substances capable of inducing irreversible hepatic necrosis remain widely accessible without mandatory pre-prescription screening. The commodification of pharmaceuticals has rendered the patient’s biological integrity an afterthought - a statistical artifact in the ledger of corporate liability. One must question the epistemological foundations of a system that permits the ingestion of hepatotoxins without informed, individualized risk stratification.
December 9, 2025 AT 23:34
Benjamin Sedler
Wait - so you’re telling me that the same guy who takes Tylenol for a headache while drinking beer is the same guy who thinks kale smoothies are "healing"? That’s not ignorance, that’s cognitive dissonance on steroids. You’ll take a pill that kills your liver but refuse a flu shot because "it’s not natural." The irony is thicker than the liver fibrosis in these cases.
December 10, 2025 AT 22:12
Karl Barrett
There’s something deeply human about this - we trust pills because they’re labeled, prescribed, approved. But the liver doesn’t care about FDA stamps or pharmacy logos. It only knows chemistry. And when the chemistry turns toxic, it doesn’t warn you. It just… stops. That’s why awareness isn’t enough. We need systems - not just advice. Automated alerts in EHRs? Mandatory pharmacist reviews? That’s the real innovation here.
December 11, 2025 AT 08:19
Isabelle Bujold
I’m a pharmacist in Vancouver, and I see this every week. A patient comes in with a stack of supplements - turmeric, ashwagandha, a "liver cleanse" tea, and a new antibiotic. They say, "I’ve been taking these for years, no problem." Then I check their med list - oh, they’re on valproate and have borderline ALT. I stop the tea, schedule a follow-up, and they’re shocked. "But it’s organic!" I say, "Organic doesn’t mean non-hepatotoxic." We need more pharmacist-led med reviews. It’s not glamorous, but it prevents ICU stays.
December 12, 2025 AT 00:31
michael booth
One pharmacy one prescriber one list of everything you take. That’s the holy trinity of liver safety. I’ve seen patients on 14 different meds including 5 OTC painkillers with hidden acetaminophen. They didn’t even know. Simple fix: write it down. Show it to your pharmacist. Ask the question. It takes five minutes. Could save your liver. Do it.
December 13, 2025 AT 14:07
Joe Lam
Let’s be real - if you’re over 35 and still taking Tylenol daily, you’re not a patient, you’re a walking liver transplant candidate. And the fact that you think "natural" supplements are safe proves you’ve never read a single peer-reviewed paper. Your ignorance is not a virtue. It’s a public health hazard.
December 13, 2025 AT 17:41
Scott van Haastrecht
My cousin died from DILI from amoxicillin-clavulanate. He was 42. Healthy. No alcohol. No supplements. Just a sinus infection. They told him it was "safe." He got jaundice on day 18. By day 22, he was in a coma. No warning. No test. No second chance. This isn’t theoretical. It’s a silent killer. And the medical system still treats it like an afterthought.
December 13, 2025 AT 22:34