Insulin Types and Regimens: How to Choose the Right Diabetes Medication
- Colin Hurd
- 19 November 2025
- 11 Comments
Choosing the right insulin isn’t about picking the most expensive or newest option. It’s about matching your life, your body, and your goals with a plan that actually works - without putting you at risk for low blood sugar or financial stress. For millions of people with diabetes, insulin isn’t a last resort. It’s a daily tool that keeps them alive and well. But with so many types and regimens out there, it’s easy to feel overwhelmed. Let’s cut through the noise.
What Are the Main Types of Insulin?
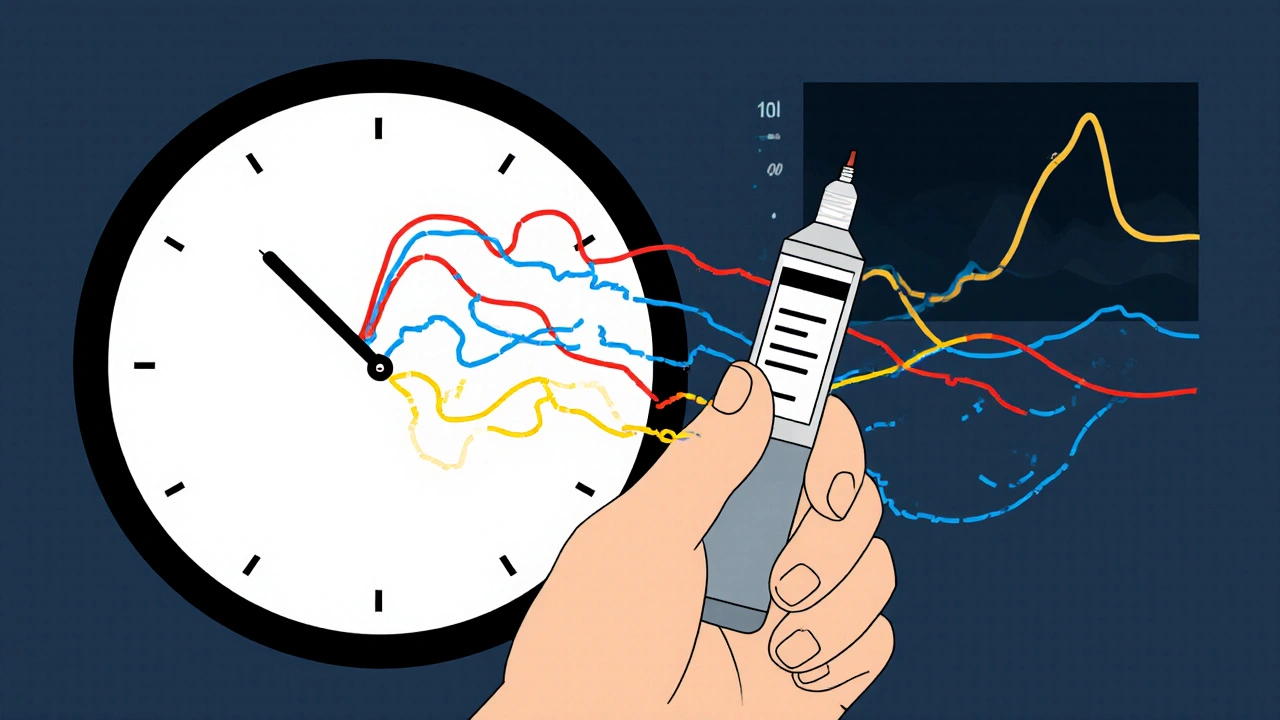
Insulin comes in different flavors - not in taste, but in timing. Each type acts on your blood sugar at a different speed and for a different length of time. Knowing the difference helps you understand why your doctor might pick one over another.
Rapid-acting insulins - like insulin lispro (Humalog), insulin aspart (NovoLog), and insulin glulisine (Apidra) - start working in 10 to 15 minutes. They peak around 30 to 90 minutes and wear off in 3 to 5 hours. These are your mealtime insulins. You take them right before or just after eating to handle the spike from food. They’re more predictable than older regular insulin and cause fewer lows after meals.
Regular (short-acting) insulin - like Humulin R and Novolin R - takes about 30 minutes to start working, peaks at 2 to 3 hours, and lasts up to 8 hours. It’s cheaper but harder to use because you have to plan meals ahead. Most people now use rapid-acting instead, unless cost is a major barrier.
Intermediate-acting insulin - NPH (Humulin N, Novolin N) - kicks in 1 to 2 hours after injection, peaks between 4 and 12 hours, and lasts 12 to 18 hours. It’s often used in the morning and evening to cover blood sugar between meals and overnight. But here’s the catch: its peak time can cause unpredictable lows, especially at night. Many people switch away from NPH because of this.
Long-acting insulins - insulin glargine (Lantus), insulin detemir (Levemir), and insulin glargine U300 (Toujeo) - provide steady background insulin with little to no peak. They last about 24 hours. These are the foundation of most modern insulin regimens. They’re designed to mimic the body’s natural baseline insulin release, so you don’t get sudden drops in blood sugar.
Ultra-long-acting insulin - insulin degludec (Tresiba) - starts working after about 6 hours and lasts over 42 hours. That means you can inject it at different times each day without losing coverage. It’s especially helpful for people with irregular schedules or those who’ve had trouble with nighttime lows. Studies show it reduces severe low blood sugar by 40% compared to glargine.
Inhaled insulin - Afrezza - is a powder you breathe in before meals. It works like rapid-acting insulin but without needles. It starts in 12 to 15 minutes and lasts about 3 hours. Great for people with needle fear - but not for smokers or those with lung issues. It’s also expensive and not covered by all insurance plans.
How Do Insulin Regimens Work?
It’s not just about which insulin you use - it’s how you use it. The way you combine different types is called your regimen. Here are the most common ones.
Basal-bolus therapy is the gold standard for type 1 diabetes and many with advanced type 2. It uses a long-acting insulin once or twice a day for background coverage (basal), plus rapid-acting insulin at each meal (bolus). This mimics how a healthy pancreas works. You adjust your mealtime doses based on what you eat, your current blood sugar, and how active you are. It gives you the most control - but it also means more injections and more learning.
Multiple Daily Injections (MDI) is just another name for basal-bolus. You’re likely to get 3 to 4 shots a day. Some people use insulin pens, others use pumps. It’s flexible and effective, especially if you use a continuous glucose monitor (CGM). People on MDI with CGMs are more likely to hit their A1C goals and have fewer lows.
Premixed insulins - like Humalog Mix 75/25 or NovoLog Mix 70/30 - combine intermediate-acting and rapid-acting insulin in one shot. They’re convenient: two shots a day, usually before breakfast and dinner. But they’re rigid. You have to eat at the same times, with the same carb amounts, every day. If your schedule changes, your blood sugar will swing. Not ideal for most people today.
Basal-only therapy is often the first step for people with type 2 diabetes. You start with a long-acting insulin once a day, usually at bedtime. This helps lower fasting blood sugar. But if your A1C stays above 8%, you’ll likely need to add mealtime insulin later. Many delay this step because they fear injections - but waiting too long can damage your organs.
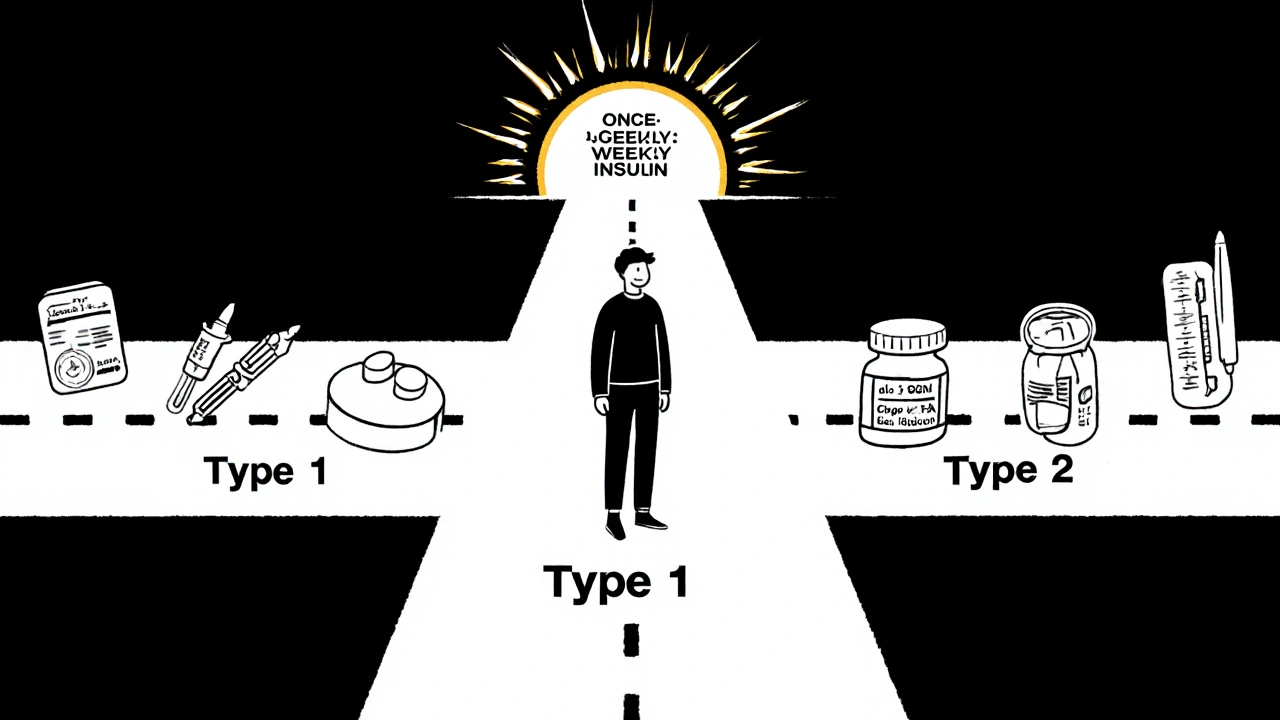
Which Insulin Is Best for Type 1 vs. Type 2 Diabetes?
Type 1 diabetes means your body makes zero insulin. You need it all day, every day. That’s why basal-bolus therapy is the standard. Most people use a long-acting insulin like Tresiba or Lantus for background, and Humalog or NovoLog for meals. Insulin pumps or hybrid closed-loop systems (like the MiniMed 780G) are common here - they automatically adjust insulin based on your CGM readings. Studies show these systems can lower A1C by 0.5% to 1% compared to injections.
For type 2 diabetes, it’s more nuanced. You might still make some insulin - just not enough. Guidelines now say to start with non-insulin drugs first if you have heart or kidney disease. GLP-1 RAs like semaglutide (Wegovy, Ozempic) and SGLT2 inhibitors like empagliflozin (Jardiance) are preferred because they protect your heart, help you lose weight, and lower your risk of kidney failure. But if your A1C is over 9.5%, or you’re very sick or losing weight, insulin becomes the fastest way to bring things under control.
When insulin is needed for type 2, starting with once-daily basal insulin is still the most common approach. But if you’re still struggling with high post-meal sugars, adding rapid-acting insulin to one or two meals - not all - can make a big difference. You don’t have to go full basal-bolus right away.
Cost Matters - A Lot
Here’s the hard truth: insulin is expensive. A vial of Humulin R (human insulin) costs $25 to $35 at Walmart’s ReliOn brand. A vial of Lantus or Tresiba can cost $250 to $350 without insurance. That’s why 1 in 4 insulin users in the U.S. still ration their doses - skipping shots or stretching vials to make them last longer. That’s dangerous.
The Inflation Reduction Act capped insulin at $35 per month for Medicare beneficiaries in 2023. That helped. But it didn’t cover everyone. In 2025, the cap is expanding to commercial insurance plans - a huge win. Still, not all plans include the cheapest analogs. And biosimilars like Semglee (a biosimilar to Lantus) are now available at about half the price. Ask your doctor or pharmacist if a biosimilar is right for you.
Human insulin isn’t perfect - it’s more likely to cause lows - but it’s safe and effective if you’re willing to learn the timing. For people on tight budgets, it’s still a valid choice. You don’t need the fanciest insulin to survive. You need one you can afford to take every day.
What About New Options?
In 2024, the FDA approved the first once-weekly insulin - basal insulin icodec. It’s designed to replace daily long-acting insulins. Early data shows it works just as well as daily degludec, with slightly better A1C results. It’s not yet widely available, but it’s a sign of where things are headed: fewer injections, better control.
There’s also progress on oral insulin. Companies like Oramed are testing pills that deliver insulin through the gut. Early trials show it can lower A1C by 0.8%. It’s not ready for prime time yet, but if it works, it could change everything for people terrified of needles.
And then there’s the rise of smart insulin pens. These connect to your phone, track your doses, and remind you when to inject. They’re not magic, but they help people stay consistent - especially those with busy lives or memory issues.
How Do You Know If Your Regimen Is Working?
It’s not just about your A1C number. It’s about how you feel. Are you having low blood sugar often? Do you feel like you’re always guessing? Are you skipping meals because you’re scared of lows? Are you spending hours calculating carbs? If the answer is yes, your regimen might need tweaking.
Here’s what success looks like:
- A1C between 7% and 8% (or lower if you’re young and healthy)
- Less than 1 low blood sugar episode per week
- No hospital visits for diabetic emergencies
- Ability to eat, travel, and live without constant fear
Most people need 6 to 12 weeks to get comfortable with insulin. Use that time to learn carbohydrate counting, understand your insulin-to-carb ratio, and practice correction doses. A certified diabetes care and education specialist (CDCES) can cut your learning curve in half.
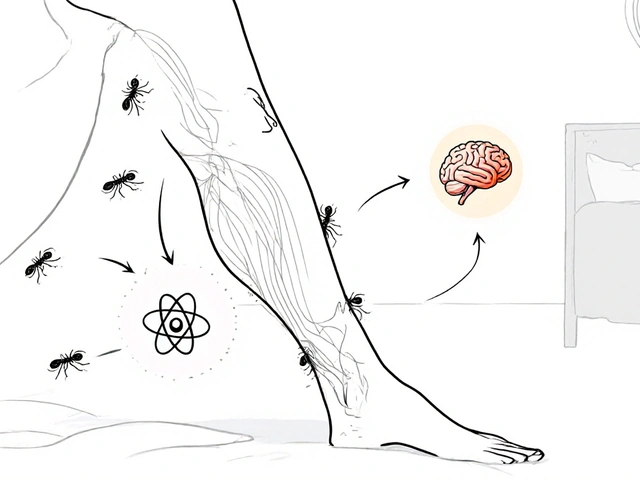
And always use a continuous glucose monitor if you can. It shows you trends, not just snapshots. You’ll see how your body reacts to food, stress, sleep, and exercise - and adjust accordingly.
Common Mistakes and How to Avoid Them
People make the same mistakes over and over:
- Waiting too long to start insulin. If your A1C is above 9%, your body is already being damaged. Don’t wait for “perfect” control.
- Using NPH at night. It peaks at 4-12 hours - that’s when you’re sleeping. You’re setting yourself up for a dangerous low.
- Not adjusting doses. Insulin needs change with weight, activity, illness, and age. A dose that worked last month might be too much now.
- Ignoring hypoglycemia. If you’re having lows, your regimen isn’t working. Talk to your provider - don’t just eat more sugar.
- Believing analogs are always better. If you can’t afford them, human insulin is still life-saving. Use it correctly.
One of the biggest myths? That insulin causes weight gain. Yes, it can - because it helps your body store energy. But that’s not a reason to avoid it. Combine insulin with movement, portion control, and non-insulin medications like GLP-1 RAs, and you can lose weight even while on insulin.
Can I switch from one insulin type to another on my own?
No. Switching insulin types requires dose adjustments and medical supervision. For example, switching from NPH to glargine usually means lowering your dose by 20% to avoid lows. Never change your insulin without talking to your doctor or diabetes educator.
Is insulin only for type 1 diabetes?
No. While all people with type 1 need insulin, about 1 in 4 people with type 2 diabetes eventually need it too. Insulin is not a sign of failure - it’s a tool. Many people with type 2 start insulin after oral meds stop working or when they’re very sick. It’s often the most effective way to get blood sugar under control quickly.
Why do some people use insulin pens and others use vials and syringes?
Pens are easier, more discreet, and more accurate. Most people prefer them. But vials and syringes are cheaper and work fine if you’re comfortable with them. Some insurance plans don’t cover pens, so people use syringes out of necessity. Both deliver insulin correctly - it’s about what works for your life.
Do I need to refrigerate my insulin?
Unopened insulin should be kept refrigerated between 2°C and 8°C. Once you start using it, most insulins are stable at room temperature (up to 30°C) for 28 to 42 days, depending on the brand. Always check the label. Don’t leave insulin in a hot car or direct sunlight.
What if I miss a dose of insulin?
If you miss a basal insulin dose, take it as soon as you remember - but don’t double up. If you miss a mealtime insulin, check your blood sugar. If it’s high, you may need a correction dose. Never skip insulin for days - high blood sugar builds up and can lead to serious complications. Talk to your provider about a plan for missed doses.
Can I stop insulin once I start?
For type 1 diabetes, no - your body doesn’t make insulin anymore. For type 2, sometimes yes. If you lose weight, become more active, or start a GLP-1 RA, your pancreas might recover some function. But this isn’t guaranteed. Never stop insulin without medical advice. Even if you feel fine, high blood sugar can be silently damaging your kidneys, eyes, and nerves.
What’s Next?
Choosing insulin isn’t a one-time decision. It’s a journey. Your needs change as you age, gain or lose weight, develop other health issues, or change your lifestyle. What works now might not work in a year. Stay flexible. Use your glucose monitor. Talk to your care team. Ask questions. And remember - insulin isn’t punishment. It’s permission. Permission to eat without fear. To move without crashing. To live a full life with diabetes.



Comments
Nikhil Purohit
Just wanted to say that NPH at night is a nightmare waiting to happen. I used to take it before bed for years until I had a seizure at 3 AM. My endo switched me to glargine and my A1C dropped half a point without any extra effort. Don't be that person who thinks 'it's always worked before' - your pancreas doesn't care about your habits, your blood sugar does.
November 20, 2025 AT 03:50
Debanjan Banerjee
Debunking a myth right here: insulin doesn't cause weight gain - your body finally starts storing energy again because it's no longer leaking glucose out through urine. That's not fat gain from insulin, that's your body healing. Pair it with GLP-1s like semaglutide and you’ll lose weight even while injecting. The real issue? People think insulin is the endgame. It's not. It's the reset button.
November 20, 2025 AT 05:19
Donald Frantz
For those of you in the US wondering why your insurance won’t cover Tresiba - it’s because the manufacturers pay pharmacies to push the expensive stuff. Biosimilars like Semglee are just as safe, just as effective, and cost $120 less per vial. Ask for it by name. Don’t let your pharmacist push you into a brand they get kickbacks on.
November 20, 2025 AT 11:25
Eliza Oakes
They say 'insulin isn't punishment' - but have you seen the price tags? This whole system is rigged. Big Pharma knows people will ration. They know we’ll skip doses. They know we’ll die quietly so their stock prices don’t dip. Don’t believe the 'it's a tool' narrative - it’s a lifeline they charge $300 for.
November 21, 2025 AT 05:32
Erika Sta. Maria
Ok but like... why are we still talking about insulin like it's the 2000s? We have AI-powered pumps that auto-adjust, we have once-weekly insulin approved, we have oral insulin in trials... and yet my cousin in Mumbai is still using syringes with expired vials because the local clinic only stocks NPH. This isn't medicine. It's a class war wrapped in a syringe.
Also, 'basal-bolus is gold standard' - sure, if you have a PhD in carb counting and a personal chef. My aunt works two jobs and sleeps 4 hours a night. She can't 'adjust for activity' - she just needs something that doesn't require a spreadsheet. Premixed insulin? Maybe not perfect - but it's the only thing that keeps her alive.
And can we talk about how Afrezza is basically the unicorn of diabetes tech? No needles? Yes please. But it costs more than my rent and my insurance says 'no' because it's 'not cost-effective.' Funny how 'cost-effective' means 'don't let poor people breathe easier.'
Also - why does no one mention that insulin pens are literally designed to be disposable? Like, the plastic casing isn't recyclable, the cartridges are single-use, and the needles are thrown away after one prick. We're talking about a chronic condition that requires 3-4 shots a day. That's 1,000+ needles a year per person. Who's cleaning up that mess? The planet? Again, this isn't healthcare - it's capitalism with a stethoscope.
And I swear to god if someone says 'just eat less sugar' one more time I'm gonna scream. Sugar isn't the villain. The system is. The lack of access is. The stigma is. Not the carbs.
November 21, 2025 AT 05:48
David vaughan
I’ve been on insulin for 12 years… and I still get nervous every time I inject. Not because I’m scared of needles - I’m scared of forgetting. One missed dose, one miscalculation, and it’s a hospital trip. That’s why I use a smart pen. It logs everything, reminds me, and even tells me if my dose is too high based on my last 3 readings. It’s not fancy… but it’s saved me from 3 ER visits. If you’re still using paper logs… please, just get a pen.
November 22, 2025 AT 01:36
Corra Hathaway
Y’all are overcomplicating this. Insulin isn’t magic. It’s just a hormone. If your body doesn’t make it, you need it. If you’re scared of needles, try Afrezza. If you can’t afford it, go to Walmart and get Humulin R. It’s not glamorous, but it keeps you alive. And if you’re still arguing about ‘best insulin’ - just pick one that doesn’t make you cry every time you pay your bill. That’s the real win.
November 22, 2025 AT 13:09
Michael Marrale
Wait… so you’re telling me the FDA approved a once-weekly insulin… but it’s not available yet? Hmm. I wonder why. Maybe because the big insulin companies don’t want people to only need one shot a week? That would cut their sales by 85%! And don’t even get me started on the ‘oral insulin’ trials - they’ve been promising it since 2010. Coincidence? I think not. The system is designed to keep you dependent. They don’t want a cure - they want a customer.
November 24, 2025 AT 00:33
Clifford Temple
Let’s be real - insulin is only ‘life-saving’ because the U.S. government lets pharmaceutical companies charge whatever they want. In Canada, a vial of Lantus costs $30. In India, it’s $15. Here? $350. This isn’t healthcare - it’s extortion. And you people act like it’s normal. It’s not. It’s criminal. And if you’re not screaming about this, you’re part of the problem.
November 24, 2025 AT 19:31
Sammy Williams
My grandma switched from Lantus to Semglee last year and saved $200 a month. She didn’t notice any difference in her blood sugar - just less stress about money. If your doc pushes you toward the expensive stuff, ask: ‘Is this really better, or just more expensive?’ Most of the time, the answer is the latter.
November 26, 2025 AT 18:04
Julia Strothers
They say insulin is a tool - but what if it’s a trap? What if the whole ‘basal-bolus’ model was designed by pharma to keep you injecting every day? What if the ‘CGM’ is just a subscription service? What if the ‘smart pens’ are spying on your habits and selling your data? I’ve been off insulin for 6 months now. I eat keto, fast 18 hours, and my A1C is 5.8. They don’t want you to know this works. They want you hooked.
November 28, 2025 AT 01:34