Latex Allergy: Cross-Reactivity and Workplace Management

- Colin Hurd
- 27 January 2026
- 11 Comments
What Is Latex Allergy?
Latex allergy isn’t just a rash from touching a balloon. It’s a real immune system overreaction to proteins in natural rubber latex, the same material used in medical gloves, condoms, and even some shoe soles. When someone with this allergy comes into contact with latex, their body treats it like a dangerous invader and releases histamine and other chemicals. That’s what causes itching, swelling, breathing trouble, or worse.
The most serious form is a Type I reaction - an IgE-mediated response that can trigger anaphylaxis. This isn’t rare in high-risk groups. People with spina bifida, for example, have a 20 to 67% chance of developing latex allergy because of repeated exposure during surgeries and medical procedures from birth. Their risk of a life-threatening reaction in an operating room is 500 times higher than someone without the condition. Even five surgeries can be enough to sensitize them.
Who’s at Risk?
Healthcare workers are the second most vulnerable group. Nurses, surgeons, lab techs, and dental staff who wear latex gloves daily are three times more likely to become sensitized than the general public. Studies show 8 to 12% of healthcare workers are allergic. The problem got worse in the 1980s and 90s when universal precautions meant everyone wore gloves - often powdered ones. That powder carried latex proteins into the air. Inhaling it led to asthma, runny noses, and eye irritation. Some workers developed full-blown allergic asthma just from breathing in glove dust.
It’s not just gloves. Latex is in blood pressure cuffs, IV tubing, catheters, elastic bandages, and even some stethoscope tubing. In a hospital setting, you don’t need to touch latex to react. Just being in the same room as someone using powdered gloves can be enough.
Cross-Reactivity: The Hidden Food Link
One of the most confusing parts of latex allergy is how it connects to food. About 30 to 50% of people with latex allergy also react to certain fruits and vegetables. This is called latex-fruit syndrome. The proteins in latex are similar to those in some plants. Your immune system gets confused and attacks both.
Common culprits include:
- Bananas
- Kiwi
- Avocados
- Castor beans
- chestnuts
- Papaya
- Apples
- Carrots
- Potatoes
Not everyone reacts to all of these. Some people only get a mild itch in their mouth when eating a banana. Others have vomiting or throat swelling. If you’ve been diagnosed with latex allergy, talk to your doctor about testing for food cross-reactivity. Don’t assume you’re safe just because you’ve eaten kiwi before - sensitivity can develop over time.

Managing Latex Allergy at Work
If you’re allergic to latex, your workplace should be your safest place - not a hazard zone. But too many workplaces still use powdered latex gloves. That’s outdated and dangerous.
Germany banned powdered latex gloves in the late 1990s. Within a few years, cases of new latex allergies among healthcare workers dropped by nearly 80%. Finland saw the same result. These aren’t theoretical wins - they’re real numbers from real policy changes.
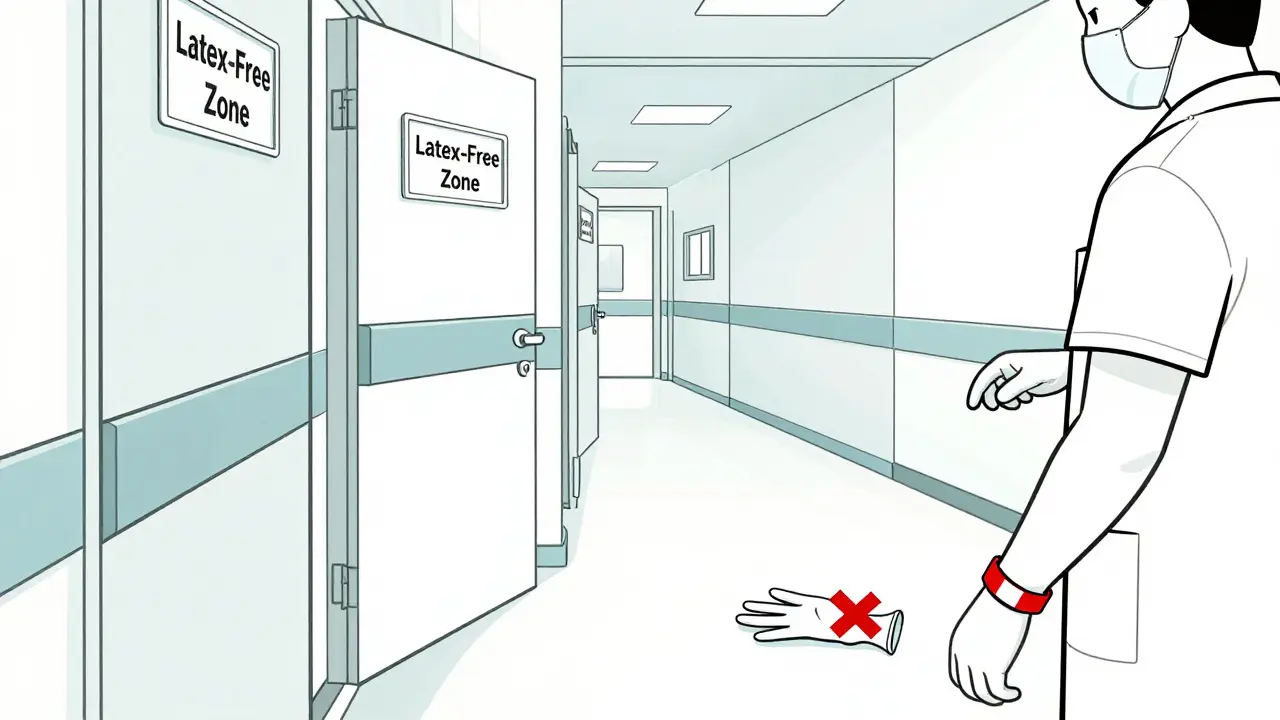
Here’s what a truly safe workplace looks like:
- All gloves are non-latex: nitrile, vinyl, or neoprene
- No powdered gloves anywhere in the facility - even in storage rooms
- Latex-free alternatives for blood pressure cuffs, tubing, and bandages
- Clear signage: “Latex-Free Zone” on doors and supply carts
- Training for all staff on what latex is, where it hides, and how to avoid cross-contamination
Even if you’re not allergic, your actions matter. If your coworker uses powdered latex gloves, you’re putting them at risk. The World Allergy Organization says: if NRL gloves must be used in the same space, everyone else must use non-powdered gloves. No exceptions.
What to Do If You Have a Reaction
Not all reactions are the same. Mild ones might mean red, itchy skin where the glove touched your hand. That’s contact dermatitis - a Type IV reaction. It’s not life-threatening, but it’s a warning sign. Use 1% hydrocortisone cream and switch to non-latex gloves.
But if you feel your throat closing, your chest tightens, or you start wheezing - that’s anaphylaxis. It’s an emergency. Every second counts.
Epinephrine is the only thing that can stop it. If you’re at risk, carry an auto-injector (like an EpiPen) at all times. Know how to use it. Practice with a trainer device. Tell your coworkers where you keep it. Don’t wait for someone else to act.
Also, wear a medical alert bracelet. In a collapse, in an ER, in a car accident - you won’t be able to speak. Your bracelet will. It could save your life.
Prevention Is the Only Cure
There’s no pill, no shot, no treatment that cures latex allergy. The only way to stay safe is to avoid it completely. That means:
- Using non-latex gloves for everything - even at home
- Checking labels on condoms, baby bottle nipples, and toys
- Asking dentists and doctors before any procedure: “Do you use latex?”
- Telling your employer, your gym, your hair salon, your airline - anyone who might handle you or your gear
It’s not paranoia. It’s survival. And it’s preventable. You don’t have to live in fear. You just have to be informed and loud about your needs.
What Employers Must Do
Employers aren’t just being nice when they go latex-free. They’re following the law. Occupational safety standards require them to protect workers from known hazards. Latex allergy is one of the most documented occupational allergies in healthcare. Ignoring it is negligence.
Here’s what employers need to do:
- Replace all powdered latex gloves with non-latex alternatives
- Establish a latex safety committee with nurses, safety officers, and allergy-aware staff
- Track allergic reactions and report them - anonymously if needed
- Provide training every year - not just on what to avoid, but how to recognize early symptoms
- Have an emergency plan for anaphylaxis - including stocked epinephrine in first aid kits
It’s cheaper than lawsuits, workers’ comp claims, and lost staff. And it’s the right thing to do.
Looking Ahead
Manufacturers have improved. Chlorination reduces allergen levels. Powder-free gloves are now the standard. But not everywhere. Some low-cost suppliers still sell old-style gloves. Some clinics still stock them because they’re cheaper.
Research is moving forward too. Scientists are working on recombinant latex allergens for better diagnosis. Maybe one day, immunotherapy will help desensitize people. But that’s still years away.
For now, the best tool we have is awareness. And action.




Comments
Katie Mccreary
I work in a hospital and we still get powdered latex gloves delivered by accident. Someone always grabs them because they're cheaper. Then someone with a latex allergy walks in and starts wheezing. It's not a mystery. It's negligence.
January 27, 2026 AT 23:02
SRI GUNTORO
People who don't take this seriously are just being selfish. If you can't afford non-latex gloves, maybe you shouldn't be in healthcare. This isn't a lifestyle choice-it's a matter of life or death.
January 28, 2026 AT 20:57
Kevin Kennett
I've been a nurse for 18 years. I developed a latex allergy after my third surgery rotation. No one warned me. No one tested me. I thought it was just dry skin until I nearly died in the ER because my EpiPen was expired. This isn't just about gloves-it's about culture. We need to stop treating allergies like inconveniences.
January 29, 2026 AT 01:55
Jess Bevis
In Nigeria, we don’t have this problem because we use gloves made from synthetic rubber. No one even knows what latex is. Why are we still using 90s tech in the US?
January 30, 2026 AT 09:03
Rhiannon Bosse
So wait… are we saying the government is letting hospitals poison people on purpose? Like, who’s behind this? Big Latex? The Glove Cartel? I’m starting to think my dentist is in on it. My mouth itches every time I go. Coincidence? I think not. 🤔
January 31, 2026 AT 23:56
Linda O'neil
If you have a latex allergy, get a medical alert bracelet. Seriously. I had a coworker pass out during a code blue and no one knew why. Turns out she had anaphylaxis and they were using latex tubing. She’s fine now, but it took 12 minutes to figure out what was wrong. Don’t be that person.
February 1, 2026 AT 11:12
Phil Davis
Funny how we all scream about 'universal precautions' but ignore the one that actually kills people. We wear masks for airborne viruses but let powdered latex float around like it's harmless. The irony is thick enough to spread on toast.
February 2, 2026 AT 03:27
Irebami Soyinka
In my country, we don’t wait for someone to die before we fix things. We ban the dangerous stuff first, ask questions later. America? You wait for a lawsuit, then you do the bare minimum. 😒 #LatexIsNotAFashionStatement
February 2, 2026 AT 10:28
Howard Esakov
I mean, if you're allergic to bananas and kiwi and now latex… are you just a walking allergen? Like, are you the human version of a hazmat suit? 😅 I'm not being mean-I'm just saying, your immune system is throwing a rave and no one invited it.
February 2, 2026 AT 20:23
Bryan Fracchia
I think the real issue isn’t the gloves-it’s how we treat people who are different. If you're allergic, you’re not being 'difficult.' You're just trying to survive in a world that treats safety like an optional upgrade. Maybe if we stopped seeing accommodations as favors and started seeing them as rights, we’d all be safer.
February 3, 2026 AT 16:51
fiona vaz
My sister is allergic and once had to leave a birthday party because someone blew up a balloon. She cried. I cried. We switched to foil balloons after that. It’s not hard. Just… don’t be lazy.
February 4, 2026 AT 22:19