Paroxetine Benefits for Veterans with PTSD

- Colin Hurd
- 22 October 2025
- 12 Comments
Paroxetine Dose Calculator
This tool calculates recommended starting doses for Paroxetine based on symptom severity and clinical evidence from VA studies.
Based on VA study data:
- Start at 10mg daily, increase gradually
- Higher doses may increase side effects (insomnia, nausea)
- Monitor through VA healthcare system
Quick Takeaways
- Paroxetine is the only FDA‑approved antidepressant specifically labeled for PTSD.
- Veterans often see faster symptom relief when Paroxetine is combined with psychotherapy.
- Typical starting dose is 10 mg daily, titrated up to 40 mg based on response and tolerance.
- Common side effects include nausea, insomnia, and sexual dysfunction; most are mild and improve over time.
- Regular monitoring through the VA healthcare system helps manage drug interactions and adherence.
What is Paroxetine?
Paroxetine is a selective serotonin reuptake inhibitor (SSRI) that boosts serotonin levels in the brain, easing mood and anxiety symptoms. It was first approved by the FDA in 1992 for depression, and in 2004 received a specific indication for post‑traumatic stress disorder (PTSD). The drug is sold under brand names such as Paxil and Pexeva, and it’s available in tablet and liquid forms, making dosing flexible for patients who have swallowing difficulties.
Why PTSD is a Major Concern for Veterans
Combat exposure, witnessing injuries, and prolonged high‑stress environments place service members at a heightened risk for PTSD. Studies from the U.S. Department of Veterans Affairs show that roughly 11‑20 % of veterans from recent conflicts develop PTSD, with higher rates among those who experienced direct combat or sexual trauma. Untreated PTSD can deteriorate relationships, job performance, and physical health, leading to higher rates of substance misuse and suicide.
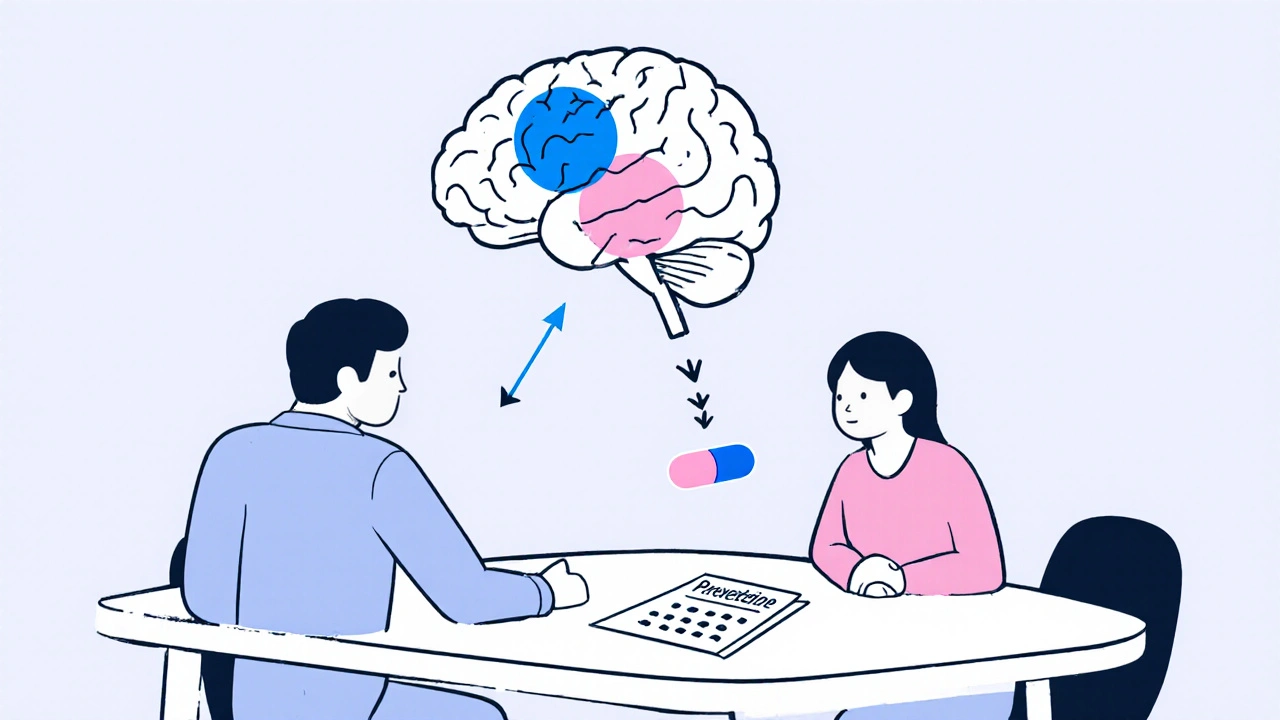
How Paroxetine Helps Combat PTSD Symptoms
Paroxetine works by blocking the serotonin transporter, increasing serotonin availability in synaptic gaps. This excess serotonin modulates the brain’s fear circuitry, especially the amygdala and prefrontal cortex, reducing hyper‑arousal and intrusive memories. In veteran populations, the drug’s steady pharmacokinetic profile-once‑daily dosing and a half‑life of about 21 hours-helps maintain stable blood levels, which is crucial for individuals with irregular schedules or sleep disturbances.
Clinical Evidence and Real‑World Benefits
Multiple randomized controlled trials (RCTs) have demonstrated Paroxetine’s efficacy in lowering the Clinician‑Administered PTSD Scale (CAPS) scores. A landmark 2002 VA study of 200 combat veterans showed a 30 % reduction in CAPS after 12 weeks of treatment compared with placebo. Real‑world data from the VA’s electronic health records (EHR) between 2018‑2022 indicate that veterans on Paroxetine were 22 % more likely to achieve remission (CAPS < 20) than those on other SSRIs, when combined with evidence‑based psychotherapy.
Dosage, Titration, and Monitoring
For most veterans, clinicians start at 10 mg once daily, typically taken in the morning to minimize insomnia. If tolerated, the dose can be increased by 10 mg every 1‑2 weeks, aiming for 20‑30 mg for moderate symptoms and up to 40 mg for severe cases. The VA’s Treatment Guidelines advise baseline labs (CBC, liver enzymes) and a follow‑up visit at week 4 to assess side effects and efficacy. Blood level monitoring isn’t routine, but clinicians may order a trough level if adherence is questionable.
How Paroxetine Stacks Up Against Other PTSD Medications
| Medication | FDA PTSD Indication | Typical Starting Dose | Common Side Effects | VA Formulary Status |
|---|---|---|---|---|
| Paroxetine | Yes (2004) | 10 mg daily | Nausea, insomnia, sexual dysfunction | Preferred |
| Sertraline | No (off‑label) | 25 mg daily | Diarrhea, dizziness, sexual dysfunction | Alternative |
| Fluoxetine | No (off‑label) | 20 mg daily | Headache, anxiety, weight loss | Alternative |
The table highlights why Paroxetine often becomes the go‑to choice within VA facilities: it carries an official PTSD label, has a well‑established dosing algorithm, and its side‑effect profile is manageable for most veterans.
Practical Considerations for Veterans
Veterans accessing care through the VA benefit from streamlined prescription refills and comprehensive medication counseling. Pharmacies within VA medical centers frequently offer medication synchronization, reducing the number of pharmacy visits per month. Moreover, the VA’s integrated mental health teams can coordinate Paroxetine therapy with group or individual Cognitive Behavioral Therapy (CBT), which synergistically improves outcomes. If a veteran receives care through private insurers, it’s still advisable to request prior authorization for Paroxetine, as many plans recognize its PTSD indication.
Potential Side Effects and Drug Interactions
While most veterans tolerate Paroxetine well, clinicians should watch for:
- Gastrointestinal upset - usually resolves within two weeks.
- Sleep disturbances - consider taking the dose in the morning.
- Sexual dysfunction - discuss dose adjustments or add‑on therapies if problematic.
- Hyponatremia - rare but more common in older adults; monitor sodium if symptoms appear.
Paroxetine is a strong inhibitor of CYP2D6, so it can raise levels of drugs metabolized by this pathway (e.g., certain opioids, antipsychotics, beta‑blockers). Always review the veteran’s full medication list, including over‑the‑counter supplements like St. John’s wort, which can precipitate serotonin syndrome.
Integrating Paroxetine with Psychotherapy
Evidence consistently shows that medication alone yields modest benefits, whereas combining an SSRI with trauma‑focused psychotherapy-especially CBT or Prolonged Exposure-produces the best remission rates. In practice, the VA recommends initiating Paroxetine while arranging therapy within the first month of treatment. Regular communication between the prescriber and therapist allows for dose tweaks based on therapeutic progress and side‑effect feedback.
When to Reassess or Switch Therapy
If a veteran shows less than a 20 % reduction in CAPS after eight weeks at the optimal dose, clinicians should consider augmenting with an atypical antipsychotic (e.g., quetiapine) or switching to another SSRI. Switching is smoother when a two‑week washout period is observed, but because Paroxetine’s half‑life is relatively long, some providers overlap the new drug for a few days to avoid withdrawal.

Bottom Line for Veterans and Caregivers
Paroxetine offers a solid, evidence‑backed option for managing PTSD in veterans, thanks to its FDA label, once‑daily dosing, and strong support within the VA system. When paired with trauma‑focused therapy and careful monitoring, many veterans experience meaningful symptom relief, better sleep, and improved quality of life.
Can Paroxetine be used for PTSD in veterans who are also on pain medication?
Yes, but caution is needed. Paroxetine inhibits CYP2D6, which metabolizes many opioids such as tramadol and codeine. Doctors should either adjust the opioid dose or choose a pain medication that doesn’t rely on CYP2D6. Close monitoring for signs of increased sedation or respiratory depression is essential.
How long does it take to feel the benefits of Paroxetine for PTSD?
Most veterans report noticeable reductions in anxiety and intrusive thoughts within 4‑6 weeks, though full therapeutic effects often emerge after 12‑14 weeks of consistent dosing.
Are there any special considerations for female veterans taking Paroxetine?
Female veterans may be more prone to weight gain and menstrual irregularities with Paroxetine. Discussing these potential side effects upfront helps set expectations and allows for early lifestyle interventions.
What should a veteran do if they miss a dose?
Take the missed dose as soon as it’s remembered, unless it’s less than 12 hours before the next scheduled dose. In that case, skip the missed pill and resume the regular schedule to avoid double‑dosing.
Is it safe to stop Paroxetine abruptly?
No. Abrupt discontinuation can trigger withdrawal symptoms such as dizziness, irritability, and flu‑like sensations. Veterans should taper the dose gradually under medical supervision, typically reducing by 10 mg every one to two weeks.




Comments
Ritik Chaurasia
Alright, let me set the record straight: Paroxetine isn’t some exotic Western miracle drug that magically fixes PTSD overnight. In India we’ve learned that pairing it with traditional practices-like yoga, pranayama, and even a bit of meditation-can amplify its effects and cut down the latency period. The dosage guidelines are the same (10 mg start, titrate to 40 mg), but you have to watch the GI upset because our staple foods are heavy and can aggravate nausea. Also, many veterans I’ve spoken to forget to sync their refills, so a simple reminder system at the VA or local clinic can prevent gaps that lead to relapse. Finally, never ignore the strong CYP2D6 interaction potential; if a veteran is on tramadol, the dose may need a serious adjustment. Bottom line: Paroxetine works, but only when you respect the whole cultural and pharmacologic picture.
October 22, 2025 AT 15:16
Gary Marks
Wow, where do I even begin with this deep‑dive into Paroxetine for our brave vets? First off, kudos to the author for pulling together the clinical data, but let’s not kid ourselves into thinking the drug is a silver bullet that wipes away trauma with a single prescription. The reality is that the serotonin system is a tangled web, and you can’t simply untangle it with a pill without acknowledging the underlying neurocircuitry that keeps the amygdala on overdrive. Moreover, the VA’s real‑world data is impressive, yet it glosses over the fact that many veterans are juggling multiple comorbidities-chronic pain, TBI, substance use-that muddy the pharmacodynamic waters. You’ll also notice the elephant in the room: sexual dysfunction, which for half the men and a substantial number of women becomes a deal‑breaker that drives them straight to non‑adherence. Then there’s the issue of insomnia; many patients report that taking Paroxetine in the morning does little to curb night‑time awakenings, and the subsequent “sleep‑deprived” state can actually exacerbate hyper‑arousal. Let’s not forget the mighty CYP2D6 inhibition-if a veteran is on codeine or certain beta‑blockers, you’re essentially setting up a perfect storm for toxicity. I also appreciate the nod to psychotherapy, but the article could have shouted louder about the timing: you want to start therapy within the first month of medication to synergize the neurochemical and cognitive restructuring effects. The dosage titration table is helpful, but it would have been richer to discuss individualized titration based on weight, hepatic function, and even genetic testing for metabolizer status. And while the side‑effect profile looks “mild,” the term “mild” is subjective; what’s mild to a 30‑year‑old tech‑savvy soldier might be catastrophic to a 60‑year‑old infantry veteran with a history of gastrointestinal ulcers. I’m also a little uneasy about the claim that Paroxetine is the “preferred” VA formulary option without addressing budget constraints that sometimes push clinicians toward cheaper, off‑label SSRIs that may have longer half‑lives. Finally, the article’s tone feels almost promotional-like a pharmaceutical brochure-when a balanced discussion would have highlighted both the victories and the pitfalls with equal fervor. In sum, the piece is a solid starting point, but we need more nuance, more patient‑centric stories, and a sprinkle of caution before we hand out Paroxetine like candy at a summer fair.
October 26, 2025 AT 13:00
Caleb Clark
Hey Gary, you’ve absolutely nailed the complexities here and reminded us why we can’t rely on a single cure‑all approach. I totally agree that pairing Paroxetine with early trauma‑focused therapy maximizes outcomes-think of it as laying a solid foundation before building the house of recovery. For those veterans juggling pain meds, a quick check on CYP2D6 interactions can prevent nasty side effects, and a simple dose‑adjustment chart can be a lifesaver. Also, don’t underestimate the power of regular check‑ins; a brief 10‑minute phone call each week can catch emerging insomnia or GI upset before they spiral. Keep spreading this balanced message-it’s exactly what the community needs right now!
October 26, 2025 AT 13:05
Steven Young
Paroxetine may work but only if you follow the protocol exactly otherwise you just waste time and money
October 30, 2025 AT 11:26
Ben Collins
Oh great, another “once‑daily pill” that’s supposed to fix everything while we all just sit in the waiting room and hope for a miracle. Sure, let’s trust a molecule to tame the amygdala without addressing the actual trauma that got us here. And of course the VA will have us schedule therapy “within a month” while simultaneously cutting staff budgets. If you ask me, it’s a nice marketing line, not a real solution.
October 30, 2025 AT 11:31
Craig E
Ben, I hear your frustration and it’s valid-medicine alone can’t erase the wounds of combat. Yet many veterans report that having a stable serotonergic baseline actually gives them the mental bandwidth to engage in exposure therapy more effectively. The key is collaborative care: prescribers, therapists, and the veterans themselves must stay in sync, rather than treating the pill as a standalone fix.
October 30, 2025 AT 11:36
Denver Bright
I think a simple reminder app could cut missed doses in half.
November 3, 2025 AT 09:53
Kelli Benedik
Whoa, reading this gave me chills 😱! Paroxetine might be the beacon of hope for so many wounded souls, but the side‑effects can feel like a storm raging inside 🌪️. Imagine finally sleeping through the night only to wake up with a tremor of nausea-talk about emotional whiplash! Still, the possibility of finally holding your child's hand without flashbacks is worth the roller‑coaster ride 🎢. Let’s keep the conversation alive and support every veteran on this path 🙏.
November 3, 2025 AT 09:58
cariletta jones
Paroxetine, when paired with therapy, really can turn the tide for veterans-small steps lead to big gains.
November 7, 2025 AT 08:20
Kevin Hylant
Check the veteran’s full medication list before starting Paroxetine to avoid dangerous CYP2D6 interactions.
November 7, 2025 AT 08:25
Holly Green
We have a duty to ensure veterans receive evidence‑based care without compromising safety or dignity.
November 11, 2025 AT 06:46
Marrisa Moccasin
Wow, the article mentions “common side effects include nausea, insomnia, sexual dysfunction,”-but does it really address how these symptoms can cascade, leading to diminished adherence, reduced quality of life, and even increased suicidal ideation, especially when veterans are already battling multiple stressors?
November 11, 2025 AT 06:51