Specialty Pharmacy and Generics: Key Practice Challenges and Patient Considerations
- Colin Hurd
- 28 December 2025
- 14 Comments
When a patient with multiple sclerosis switches from a $78,000-a-year brand-name drug to a generic version costing $45,000, the savings look obvious. But for the pharmacist dispensing it, the reality is far more complicated. Specialty pharmacies don’t just fill prescriptions-they manage entire treatment journeys. And when generics enter that space, the rules change. It’s not about cost alone. It’s about stability, trust, and precision.
What Makes Specialty Pharmacy Different?
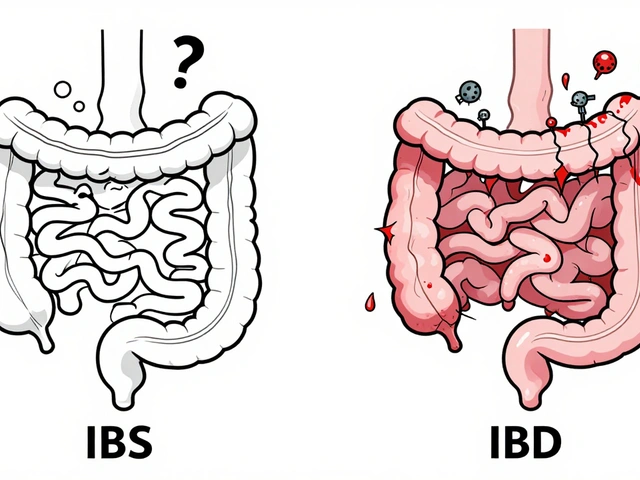
Specialty pharmacy isn’t your local drugstore. These pharmacies handle high-cost, complex medications for chronic conditions like cancer, rheumatoid arthritis, hepatitis C, and HIV. Most of these drugs are biologics-made from living cells, not chemicals. They need cold storage (2-8°C), special handling, and frequent monitoring. Many are given by injection or infusion. Patients often need ongoing education, side effect management, and lab tracking. This isn’t just dispensing. It’s care coordination. Unlike retail pharmacies where 90% of prescriptions are generics, specialty pharmacies rarely see them. Why? Because most specialty drugs have no generic alternative. Until recently, that was the norm. But now, as patents expire, generics-and especially biosimilars-are entering the space. And that’s where things get messy.Generics in Specialty: Not All Are Created Equal
The FDA says generics must be bioequivalent to brand-name drugs. That means they deliver the same active ingredient at the same rate and amount. On paper, it’s a clean standard. In practice, it’s not that simple. For drugs with a narrow therapeutic index (NTI)-like levothyroxine, warfarin, or some epilepsy meds-tiny differences in blood levels can cause serious harm. A patient stable on one generic brand might have a seizure or thyroid crash after switching to another, even if both are FDA-approved. Pharmacists know this. Patients don’t. One Reddit user shared how their thyroid levels spiked after switching generic manufacturers. Their pharmacist said, “It’s the same drug.” But the body doesn’t see it that way. Inactive ingredients-fillers, dyes, coatings-can affect absorption. And those aren’t tracked in bioequivalence studies. Specialty pharmacies must document every switch. They need to know which manufacturer the patient is on. They need to flag allergies to specific excipients. And they need to monitor labs closely after a change. That’s extra work. Extra risk. Extra time.Biosimilars: The New Frontier
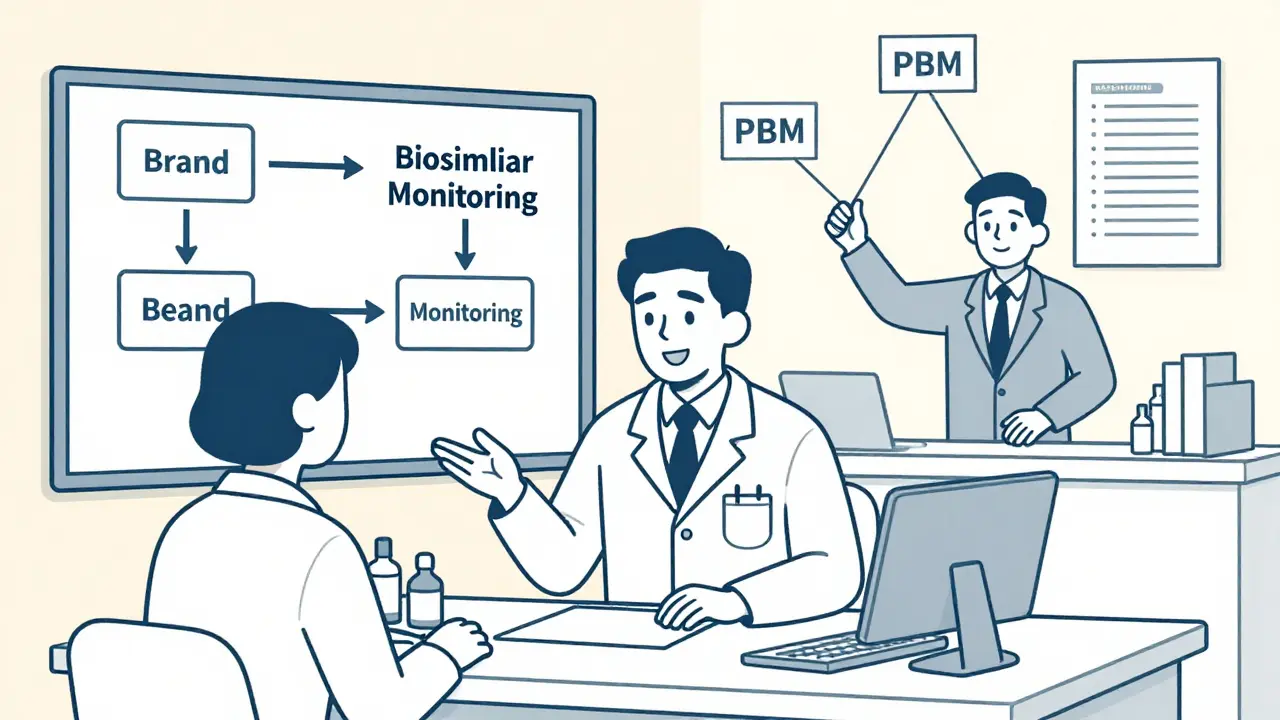
Biosimilars are the generic version of biologics. They’re not exact copies-biologics are too complex for that. But they’re highly similar, with no clinically meaningful differences in safety or effectiveness. The FDA approved its first interchangeable biosimilar, Semglee (for insulin glargine), in 2021. By December 2023, 35 biosimilars had been approved. But adoption is slow. Why? Because PBMs (Pharmacy Benefit Managers) control the money. Many still place biosimilars on higher tiers, making patients pay more out-of-pocket. Some require prior authorizations that take weeks. Others don’t even list them on formularies. That’s not about science. It’s about rebates. Specialty pharmacies are caught in the middle. They’re pressured to increase their Generic Dispensing Ratio (GDR), even when no generic exists for the drug they’re dispensing. One pharmacy owner told me they were penalized for a 60% GDR-even though 80% of their inventory had no generic alternative. The system doesn’t match reality.
Cost vs. Care: The Real Trade-Off
Yes, generics save money. The generic version of Copaxone cut annual costs from $78,000 to $45,000. That’s huge for insurers and patients. But savings shouldn’t come at the cost of stability. A 2014 study showed that specialty pharmacy services boosted adherence to MS therapy from 33% to 60%. That’s not because they sold cheaper drugs. It’s because they called patients, tracked labs, answered questions, and managed side effects. That’s the value. Switching a patient to a generic without proper support can undo all that. A patient who’s stable, compliant, and feeling well might panic when their pill changes color. They might stop taking it. They might go to the ER. The cost of that visit? Far higher than the drug savings.How Specialty Pharmacies Should Handle Generics
There’s no one-size-fits-all rule. But here’s what works:- Start with your top therapies. Focus on conditions where generics are available and evidence supports substitution-like rheumatoid arthritis or hepatitis C.
- Standardize your inventory. Don’t stock five different generic manufacturers for the same drug. Pick one preferred source. It reduces confusion and simplifies tracking.
- Document patient-specific risks. If a patient has had a reaction to a specific filler, note it in their file. Don’t assume all generics are interchangeable.
- Don’t switch without consent. Talk to the patient. Explain why you’re changing, what to watch for, and when to call. Don’t wait for them to notice the pill looks different.
- Monitor after substitution. For NTI drugs, check labs 4-6 weeks after switching. Don’t assume bioequivalence means identical response.
- Work with one distributor. Sourcing generics from multiple vendors creates administrative chaos. Stick with one reliable partner who understands specialty needs.
What Patients Need to Know
Patients are confused. They hear “generic = cheaper” and assume “same = better.” But it’s not that simple. They need to understand:- Generic pills may look different-but that doesn’t mean they’re less effective.
- Switching between generic brands isn’t always safe, especially for NTI drugs.
- If they feel different after a switch, they should contact their pharmacist immediately-not wait for symptoms to worsen.
- Biosimilars aren’t “inferior.” They’re rigorously tested and just as safe as the original biologic.
The Bigger Picture: Policy, Profit, and Patients
The U.S. healthcare system is built on incentives that don’t always align with patient outcomes. PBMs profit from brand-name drugs through rebates. They lose money when biosimilars are used. So they make it harder to switch. Meanwhile, specialty pharmacies operate on razor-thin margins. Many are reimbursed below what they pay for the drug. Add in the cost of staffing, cold storage, and patient support-and it’s a miracle they stay open. The solution isn’t to force more generics. It’s to fix the system. PBMs need to stop penalizing pharmacies for not dispensing generics that don’t exist. Formularies need to be transparent. Reimbursement needs to reflect real costs. And patients need to be treated like partners, not cost centers.What’s Next?
More biosimilars are coming. Humira’s first biosimilars launched in 2023. Others will follow. The Congressional Budget Office estimates biosimilars could save $54 billion over the next decade. But those savings won’t happen unless specialty pharmacies can do their job without broken incentives. That means:- Clear rules for biosimilar substitution
- Reimbursement that covers real costs, not just list prices
- Training for pharmacists on biosimilar education
- Systems to track patient outcomes after switches
Can I switch my patient from a brand-name specialty drug to a generic without consulting the prescriber?
No. Even if a generic is available, switching a patient on a specialty medication requires clinical judgment. For drugs with a narrow therapeutic index-like levothyroxine, warfarin, or some immunosuppressants-switching without approval can lead to treatment failure or serious side effects. Always check state laws, prescriber preferences, and patient history before making any substitution. Document the decision and notify the prescriber.
Why do generic specialty drugs look different even when they’re the same medication?
Generic drugs must contain the same active ingredient, but they can use different inactive ingredients-like fillers, dyes, or coatings. These affect color, shape, and markings, but not effectiveness. The problem? Patients often think a change in appearance means the drug is different or weaker. That’s why counseling is critical. Always explain the change, reassure the patient, and warn them to report any new side effects.
Are biosimilars the same as generics?
No. Generics are exact chemical copies of small-molecule drugs. Biosimilars are highly similar to complex biologic drugs, but not identical. They’re made from living cells, so minor differences are unavoidable. However, they must show no clinically meaningful differences in safety or effectiveness. Biosimilars require special education because patients and providers often confuse them with generics. Interchangeable biosimilars can be substituted like generics, but only if the FDA has designated them as such.
Why do some specialty pharmacies get penalized for low generic dispensing rates?
Some Pharmacy Benefit Managers (PBMs) measure a Generic Dispensing Ratio (GDR) and penalize pharmacies that don’t meet targets. But many specialty drugs-especially biologics-have no generic version. Penalizing pharmacies for this is like punishing a bakery for not selling gluten-free cakes when no flour exists. This misalignment creates unfair pressure and can lead to poor decisions. Pharmacies should push back and demand metrics that reflect actual drug availability.
How can specialty pharmacies improve patient adherence when switching to generics?
Adherence drops when patients are confused or scared. To prevent this, specialty pharmacies should: (1) Contact patients before switching to explain why and what to expect, (2) Provide written materials with the new pill’s appearance, (3) Schedule follow-up calls 2-4 weeks after the switch to check for side effects, and (4) Offer medication therapy management (MTM) to address concerns. Studies show these steps can maintain or even improve adherence rates after substitution.


Comments
Teresa Rodriguez leon
Switching a patient on MS therapy to a generic without warning them about the pill color change is a recipe for non-adherence. I’ve seen patients quit cold turkey because they thought the new pill was counterfeit. No one tells them the inactive ingredients changed. The pharmacy’s job isn’t just to dispense-it’s to prevent panic.
December 29, 2025 AT 18:37
Jasmine Yule
Let’s be real-PBMs are the real villains here. They get kickbacks from brand-name manufacturers and punish pharmacies for not pushing generics that don’t exist. It’s like blaming a barber for not selling hair transplants. The system is broken, and frontline pharmacists are the ones getting fired for it.
December 31, 2025 AT 18:17
Manan Pandya
As a pharmacist in Mumbai, I’ve seen this play out with biosimilars for rheumatoid arthritis. The science supports substitution, but cultural mistrust runs deep. Patients equate cheaper with inferior. We spend hours educating them-not because it’s in the job description, but because someone has to. The FDA’s bioequivalence standards are a technicality. The human response is what matters.
January 1, 2026 AT 12:35
Aliza Efraimov
I work in a specialty pharmacy in Texas, and I can tell you-this isn’t theoretical. Last week, a patient on a biosimilar for psoriasis started having joint pain again after we switched her to a different manufacturer’s version. Same drug, different filler. Her rheumatologist didn’t believe us until we pulled the lab results. We’re not just pharmacists-we’re detectives, therapists, and patient advocates rolled into one. And we’re underpaid for it.
Stop treating us like order-fillers. We’re managing chronic disease, not selling aspirin.
January 3, 2026 AT 04:14
Nisha Marwaha
From a pharmacoeconomic standpoint, the Generic Dispensing Ratio (GDR) metric is fundamentally misaligned with the clinical reality of specialty pharmacy. Biologics, by their nature, are not subject to traditional generic substitution paradigms. The emergence of biosimilars necessitates a redefinition of substitution protocols, particularly regarding interchangeability designation under the Biologics Price Competition and Innovation Act (BPCIA). Without granular tracking of excipient profiles and pharmacokinetic variability, GDR incentivizes commoditization over individualized care.
January 4, 2026 AT 23:01
Paige Shipe
Wow. So pharmacists are heroes now? Maybe if you stopped switching patients’ meds without telling them, they wouldn’t panic. Also, why are you even working in specialty pharmacy if you’re so afraid of a little cost-saving? It’s 2025. Everything’s generic now. Get with the program.
January 6, 2026 AT 17:43
Tamar Dunlop
While I appreciate the nuanced perspective presented herein, I must respectfully posit that the structural inequities embedded within the Pharmacy Benefit Manager (PBM) ecosystem represent not merely a logistical challenge, but a profound moral failure in the delivery of equitable healthcare. The commodification of life-sustaining therapeutics-particularly for populations already burdened by socioeconomic disparity-demands systemic reform, not merely operational adjustments.
January 8, 2026 AT 08:29
David Chase
USA. We’re #1 in healthcare innovation. Why are we still letting foreign generics and biosimilars mess with our patients’ brains? If it ain’t broke, don’t fix it! Brand-name drugs are American-made. The FDA’s just caving to global pressure. This is why our kids can’t afford insulin-because we let China and India play with our medicine supply chain. STOP THE SWITCHING. AMERICA FIRST.
💯🇺🇸💊
January 8, 2026 AT 11:11
Emma Duquemin
Y’all are acting like switching generics is like swapping out your coffee creamer. It’s not. I had a patient on a biosimilar for lupus who went from feeling like a superhero to feeling like a ghost in two weeks. We didn’t change the drug-we changed the manufacturer. The fillers? Different. The patient’s anxiety? Sky-high. We called her every day for a week. We sent her a photo of the new pill. We sat with her while she cried. That’s not pharmacy. That’s love in a white coat.
And yes-I cried too.
January 9, 2026 AT 18:22
Kevin Lopez
NTI drugs + generics = bad. Biosimilars ≠ generics. GDR is a flawed metric. PBMs are corrupt. Document everything. Don’t switch without consent. End of story.
January 11, 2026 AT 17:30
Duncan Careless
Interesting piece, though I wonder if the focus on pharmacy-level interventions overlooks the broader regulatory inertia. The UK’s NHS has implemented standardized biosimilar substitution protocols with patient education packs-something we seem reluctant to adopt. Perhaps the issue isn’t just incentives, but a cultural aversion to standardization in U.S. healthcare.
January 13, 2026 AT 01:53
Samar Khan
So what? Patients die when they don’t take their meds. If the generic is cheaper, they should just take it. Stop making it a drama. Also, your ‘specialty pharmacy’ is just a fancy word for ‘expensive pharmacy.’
😂💊
January 14, 2026 AT 12:39
Russell Thomas
Oh wow, so now pharmacists are the new therapists? Can we just make them licensed psychiatrists too? I mean, if a pill changes color and someone has an existential crisis… maybe they shouldn’t be on a $45k drug in the first place. Just saying.
January 16, 2026 AT 03:33
Joe Kwon
Just had a 3-hour meeting with our PBM about GDR penalties. We showed them our inventory: 78% of our drugs have no generic. They still want 80% GDR. I asked if they’d penalize a bookstore for not selling books in Klingon. They didn’t laugh. That’s the problem.
January 16, 2026 AT 16:58