IBS vs. IBD: What’s the Real Difference Between Functional and Inflammatory Bowel Disorders?
- Colin Hurd
- 4 December 2025
- 11 Comments
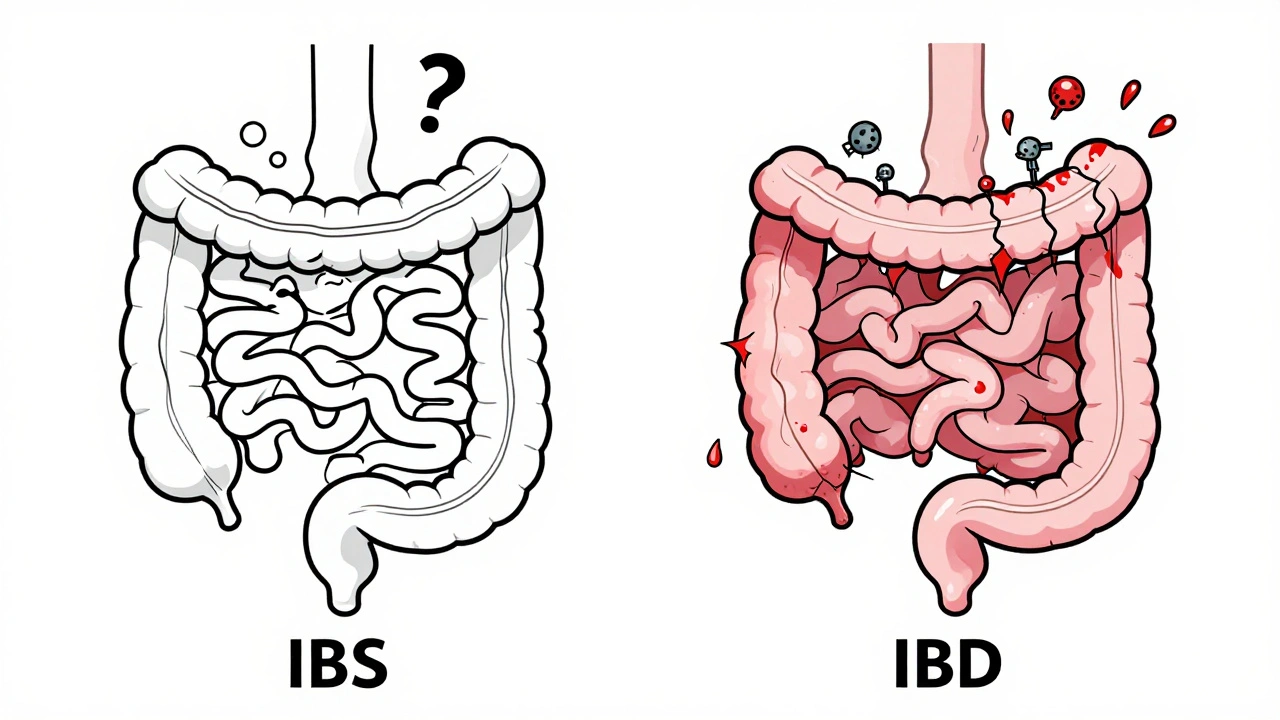
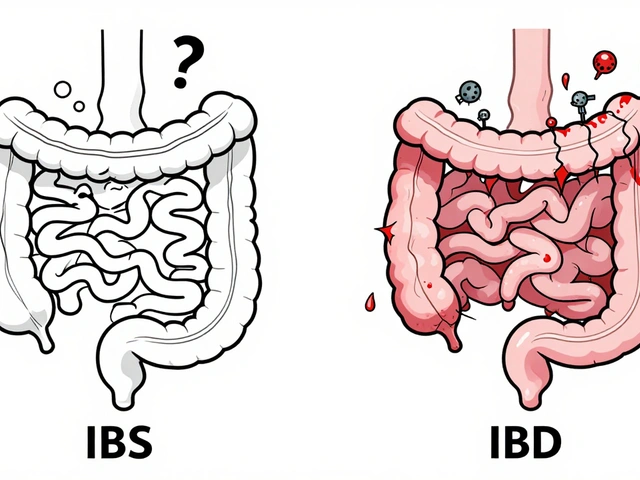
Think you have a bad case of stomach bugs or food intolerance? Maybe it’s IBS. Or maybe it’s something more serious-IBD. The symptoms can feel almost identical: cramps, bloating, diarrhea, constipation. But here’s the truth most people don’t tell you-IBS and IBD aren’t just different versions of the same thing. They’re completely different diseases. One doesn’t damage your gut. The other can tear it apart.
IBS: Your Gut Is Working, But It’s Confused
IBS-irritable bowel syndrome-isn’t about inflammation, ulcers, or tissue damage. It’s a functional disorder. That means your digestive tract looks perfectly normal on a colonoscopy, blood test, or MRI. But it doesn’t behave right. It’s like your gut has a faulty wiring system. Signals get mixed up. Muscles contract too hard or too weak. Nerves become overly sensitive. Even normal gas or food movement can feel like sharp pain.
The Rome IV criteria, used by doctors worldwide since 2016, define IBS by three key things: abdominal pain at least one day a week for three months, plus two of these: pain linked to bowel movements, changes in stool frequency, or changes in stool appearance. You might have diarrhea most days (IBS-D), constipation most days (IBS-C), or switch back and forth (IBS-M). Bloating hits 76% of people with IBS. Mucus in stool? That’s common too-seen in nearly half of cases.
Here’s what you won’t find with IBS: blood in your stool, unexplained weight loss, fever, or anemia. If you have any of those, it’s not IBS. It’s something else. And you need to see a doctor right away.
IBS doesn’t lead to cancer. It doesn’t cause strictures or fistulas. It won’t land you in the hospital from a flare-up. But it can wreck your life. People with IBS report giving up coffee, sex, travel, even their phones-just to avoid a bathroom emergency. That’s how disruptive it is.
IBD: Your Gut Is Under Attack
IBD- inflammatory bowel disease-is not a glitch. It’s a war. Your immune system turns on your own digestive tract, attacking the lining like it’s an invader. This causes real, visible damage: ulcers, deep inflammation, scarring, and holes in the bowel wall. There are two main types: Crohn’s disease, which can hit anywhere from mouth to anus, and ulcerative colitis, which only affects the colon and rectum.
Unlike IBS, IBD shows up on tests. Blood work? Elevated CRP and ESR-signs of inflammation. Stool tests? Fecal calprotectin above 250 µg/g (normal is under 50). Colonoscopy? You’ll see red, swollen tissue, bleeding ulcers, or cobblestone lesions. MRI scans show thickened bowel walls or fistulas. These aren’t just symptoms. These are physical injuries.
And the symptoms? They go beyond cramps and bloating. Blood in your stool? Very common-92% of ulcerative colitis patients have it at diagnosis. Black, tarry stools? That’s internal bleeding from Crohn’s. Weight loss? 65% of IBD patients lose weight during flares. Fever? Happens in 40% of moderate to severe cases. You might also get joint pain, red, painful eye patches (uveitis), or painful red bumps on your shins (erythema nodosum). These aren’t random side effects. They’re signs your immune system is attacking your body beyond your gut.
IBD can lead to life-threatening complications. After 10 years of pancolitis, your risk of colorectal cancer jumps by 2% each year. Toxic megacolon-a dangerous swelling of the colon-can happen in 2-4% of severe ulcerative colitis cases. Strictures? One in three Crohn’s patients develops them within a decade. Fistulas? One in six. These aren’t rare. They’re expected outcomes without proper treatment.
How Doctors Tell Them Apart
There’s no single test for IBS. Doctors diagnose it by ruling everything else out. If your blood work is clean, your colonoscopy shows no inflammation, your stool tests are normal, and you don’t have any alarm symptoms-then IBS is the diagnosis. It’s a diagnosis of exclusion. That doesn’t mean it’s imaginary. It just means the damage isn’t visible.
IBD? It’s the opposite. Doctors look for proof of inflammation. They take biopsies during colonoscopy. They check for elevated CRP and calprotectin. They do MRIs to see if the bowel wall is thickening. They look for ulcers, fissures, or fistulas. If any of that shows up, it’s IBD. No guesswork. No waiting. The damage is there.
And here’s something most people don’t know: you can have both. About one in three people with IBD in remission still meet the criteria for IBS. Their gut is healing from inflammation, but the nerves are still hypersensitive. So they get bloating and cramps-even though the inflammation is gone. That’s why treatment has to be layered.

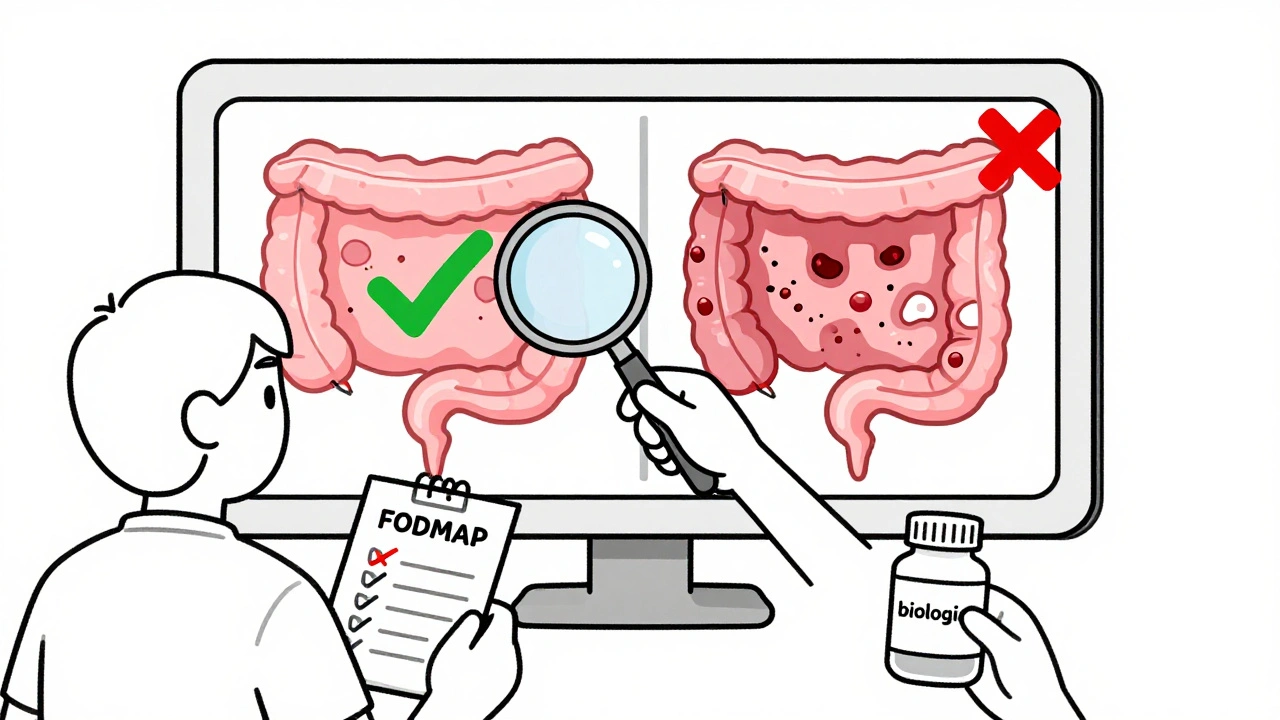
Treatment: Fixing the Wiring vs. Stopping the War
IBS treatment isn’t about drugs that kill inflammation. It’s about calming the nervous system and training the gut.
- The low-FODMAP diet cuts out fermentable carbs that feed gas-producing bacteria. It works for 76% of people with IBS.
- Low-dose tricyclic antidepressants (like amitriptyline) don’t treat depression here-they quiet overactive gut nerves. They reduce pain in 60% of patients.
- Medications like eluxadoline help slow down bowel movements in IBS-D. It improves pain and diarrhea in 35-40% of cases.
- Stress management, gut-directed hypnotherapy, and regular movement are just as important as diet.
IBD treatment is about stopping the immune system from destroying your gut.
- Corticosteroids (like prednisone) bring flares under control fast-70-80% effective-but they’re not safe long-term.
- Biologics like infliximab block TNF-alpha, a key inflammation driver. Half to 60% of Crohn’s patients go into remission within 14 weeks.
- Vedolizumab targets gut-specific immune cells. It helps 48% of ulcerative colitis patients stay in remission after a year.
- Surgery? Sometimes needed. Removing the colon can cure ulcerative colitis. Crohn’s patients often need bowel resections when strictures or fistulas form.
IBS treatments don’t change your disease. They help you live with it. IBD treatments can change the course of your life-preventing cancer, hospitalizations, and surgeries.
What You Need to Do Right Now
If you’ve been told you have IBS but you’re losing weight, bleeding from your rectum, running fevers, or have a family history of colon cancer-get retested. You might have IBD. And IBD gets worse if it’s ignored.
If you have IBD and your symptoms improve on medication but you still get bloating and cramps-you might also have IBS. Don’t assume it’s just "IBD flaring." Ask your doctor about gut-brain therapies.
If you have IBS and you’re on a low-FODMAP diet but still struggling-don’t blame yourself. This isn’t about willpower. It’s about your nervous system being stuck in overdrive. Try gut-directed hypnotherapy. Studies show it works as well as diet for many people.
And if you’re not sure? Get tested. Don’t wait. Blood tests, stool tests, and a colonoscopy are quick. They’re not scary. They’re life-saving.
IBS won’t kill you. But it can make you feel like you’re dying every day. IBD can kill you-if you don’t treat it. But with the right care, both can be managed. The key is knowing which one you have.
Can IBS turn into IBD?
No. IBS does not develop into IBD. They are completely different conditions. IBS is a functional disorder with no inflammation or tissue damage. IBD is an autoimmune disease that causes physical damage to the bowel. You can have both at the same time, but one does not cause the other.
Is blood in the stool a sign of IBS?
No. Blood in the stool is never a symptom of IBS. If you see red blood in your toilet, on toilet paper, or in your stool, it’s a red flag for IBD, colorectal cancer, or another serious condition. See a doctor immediately.
Can stress cause IBD?
Stress doesn’t cause IBD, but it can trigger flares. IBD is caused by genetic and immune factors. Stress doesn’t create the disease, but it can make symptoms worse by affecting gut motility and immune response. Managing stress is part of treatment-but not the cure.
Do I need a colonoscopy to diagnose IBS?
Not always, but often yes. Doctors use colonoscopy to rule out IBD, cancer, or infections before diagnosing IBS. If you’re under 50, have no alarm symptoms, and test results are normal, a colonoscopy may not be needed. But if you’re over 50, have weight loss, bleeding, or a family history of colon cancer, a colonoscopy is required.
Can IBD be cured?
Ulcerative colitis can be cured by removing the entire colon. Crohn’s disease cannot be cured, but it can be put into long-term remission with medication. Many people with Crohn’s live full, active lives without symptoms for years. The goal is to stop inflammation before it causes permanent damage.
Are there foods that trigger IBS but not IBD?
Yes. High-FODMAP foods-like onions, garlic, beans, wheat, and dairy-are common triggers for IBS because they ferment in the gut and cause gas and bloating. People with IBD can also react to these, but their triggers are more about inflammation-spicy foods, alcohol, and high-fat meals. A low-FODMAP diet helps IBS, but it doesn’t treat IBD.
What’s the biggest myth about IBS and IBD?
That IBS is "all in your head." It’s not. The pain is real. The bloating is real. The impact on your life is real. The difference is that IBS doesn’t show up on scans because it’s a nervous system issue, not a structural one. That doesn’t make it less serious. It just means treatment looks different.

Comments
Ashley Elliott
Just wanted to say this post saved me months of guesswork. I thought I had IBS, but when I started bleeding and lost 15 pounds, I pushed for a colonoscopy-turns out it was Crohn’s. If you’re unsure, get tested. Seriously.
Also, low-FODMAP helped me, but only after I stopped blaming myself for "being too picky." It’s not about willpower.
December 5, 2025 AT 22:47
Chad Handy
Look, I’ve had IBD for 12 years and I’ve seen every gimmick under the sun-probiotics, CBD oil, alkaline diets, colon cleanses-and none of it matters unless you’re on biologics. The pharmaceutical industry doesn’t want you to know this, but the truth is your immune system is broken and no amount of yoga or turmeric is going to fix it. You need real medicine. Not wellness culture.
December 7, 2025 AT 09:48
Augusta Barlow
Wait-so you’re telling me the government and Big Pharma are using IBS as a cover-up for IBD? Why? So they can sell you expensive drugs for something that doesn’t exist? I’ve read studies where they inject people with fake inflammation markers just to keep the diagnosis wheel turning. And colonoscopies? They’re not diagnostic-they’re surveillance tools to track who’s "compliant."
My cousin went in for "IBS," came out with a stoma. They never told her it was coming. Coincidence? I think not.
December 8, 2025 AT 14:50
Joe Lam
Let’s be clear: IBS is not a diagnosis. It’s a dumping ground for doctors who don’t want to do the work. You think your gut is "confused"? It’s not. It’s inflamed. You’re just too lazy to get the right tests. Fecal calprotectin isn’t optional-it’s basic. If you’re not getting it, you’re being failed by the system. And yes, I’ve read the Rome IV criteria. I’ve also read the meta-analyses that show 40% of IBS diagnoses are wrong.
Stop romanticizing functional disorders. They’re not mystical. They’re misdiagnosed.
December 9, 2025 AT 04:30
Jenny Rogers
One must consider the ontological implications of somatization in the context of modern gastroenterological epistemology. The Cartesian dichotomy between mind and body has been thoroughly deconstructed by phenomenological medicine, yet the diagnostic framework for IBS remains stubbornly reductionist, perpetuating a hegemonic biomedical paradigm that pathologizes embodied experience while simultaneously erasing its phenomenological authenticity.
Indeed, to label IBS as "functional" is to imply that the suffering is not materially grounded-an epistemological violence that silences the lived reality of those whose pain exceeds the visible metrics of pathology. One might argue, then, that IBS is not a disorder of the gut, but a disorder of the diagnostic gaze.
December 10, 2025 AT 13:34
Rachel Bonaparte
Okay, but have you considered that IBS might be a response to chronic emotional trauma? I mean, think about it-your gut is literally your second brain. If you grew up in a household where you were never allowed to express anger, your nervous system learns to store it in your colon. I had IBS for years, and once I did somatic therapy and cleared out my childhood shame, my symptoms vanished. No diet, no meds.
And don’t even get me started on how IBD is linked to glyphosate in the food supply. The WHO knows. They just won’t say it. I’ve seen the leaked documents. The gut is a mirror of the world’s poison-and we’re all paying the price.
December 12, 2025 AT 10:49
Scott van Haastrecht
THIS IS WHY PEOPLE DIE. You think IBS is "just stress"? My sister had IBS for five years. They told her to eat more fiber. She started bleeding. She lost 30 pounds. They told her it was "anxiety." By the time they diagnosed her with ulcerative colitis, her colon was 80% destroyed. She’s on biologics now. She can’t have kids. She’s in chronic pain. And it all started because someone called her symptoms "functional." Stop being nice. Stop being polite. If you have diarrhea and pain, get a colonoscopy. Now. Not next month. Not when you "feel ready."
People are dying because you’re too afraid to ask for help.
December 12, 2025 AT 11:49
Chase Brittingham
I just want to say thank you for writing this. I’ve been living with IBD for 8 years and I’ve never seen it explained so clearly. The part about having both IBS and IBD in remission? That’s me. I thought I was failing at my treatment until I found out my nerves were still screaming even though the inflammation was gone.
Gut-directed hypnotherapy changed my life. I didn’t believe it at first-thought it was woo. But after 12 sessions, my bloating dropped 80%. No meds. Just my brain learning to chill out.
If you’re reading this and you’re scared to try something new-just give it a shot. You’ve got nothing to lose but the pain.
December 13, 2025 AT 13:08
michael booth
IBS is real. IBD is deadly. Get tested.
December 14, 2025 AT 19:30
Heidi Thomas
Low-FODMAP? That’s just a fancy way of saying "don’t eat anything." And hypnotherapy? Please. If your gut is inflamed, you need steroids, not meditation. I’ve seen people waste years on diets while their Crohn’s eats through their bowel. Stop pretending lifestyle changes are enough. You need immunosuppressants. Period.
December 15, 2025 AT 04:23
Alex Piddington
Thank you for this comprehensive and clinically accurate breakdown. I appreciate the emphasis on distinguishing between functional and structural pathology-a distinction too often blurred in online discourse. The inclusion of fecal calprotectin as a key biomarker is particularly commendable, as it is underutilized in primary care settings.
I would only add that while biologics are transformative, their cost and accessibility remain significant barriers globally. A truly equitable approach to IBD care must address not only medical efficacy but also socioeconomic determinants of health.
For those with IBS, I encourage integration of cognitive behavioral therapy with dietary modification. The evidence for this combined approach is robust and underappreciated.
December 15, 2025 AT 13:39