Surgical Treatments for Penile Lymphedema: Options, Risks, and Recovery
- Colin Hurd
- 18 October 2025
- 12 Comments
Penile Lymphedema Surgical Option Selector
Find Your Best Surgical Option
Answer a few questions to determine which surgical procedure may be most appropriate for your specific situation. This tool is for informational purposes only and should not replace professional medical advice.
When fluid builds up in the penis and skin becomes thick, swollen, or painful, many men wonder if there’s anything beyond creams and compression that can help. Penile lymphedema is a rare condition where the lymphatic system fails to drain fluid from the penile shaft, leading to chronic swelling, discomfort, and sometimes infection. While conservative measures work for early stages, severe cases often require a surgical approach to restore both function and confidence.
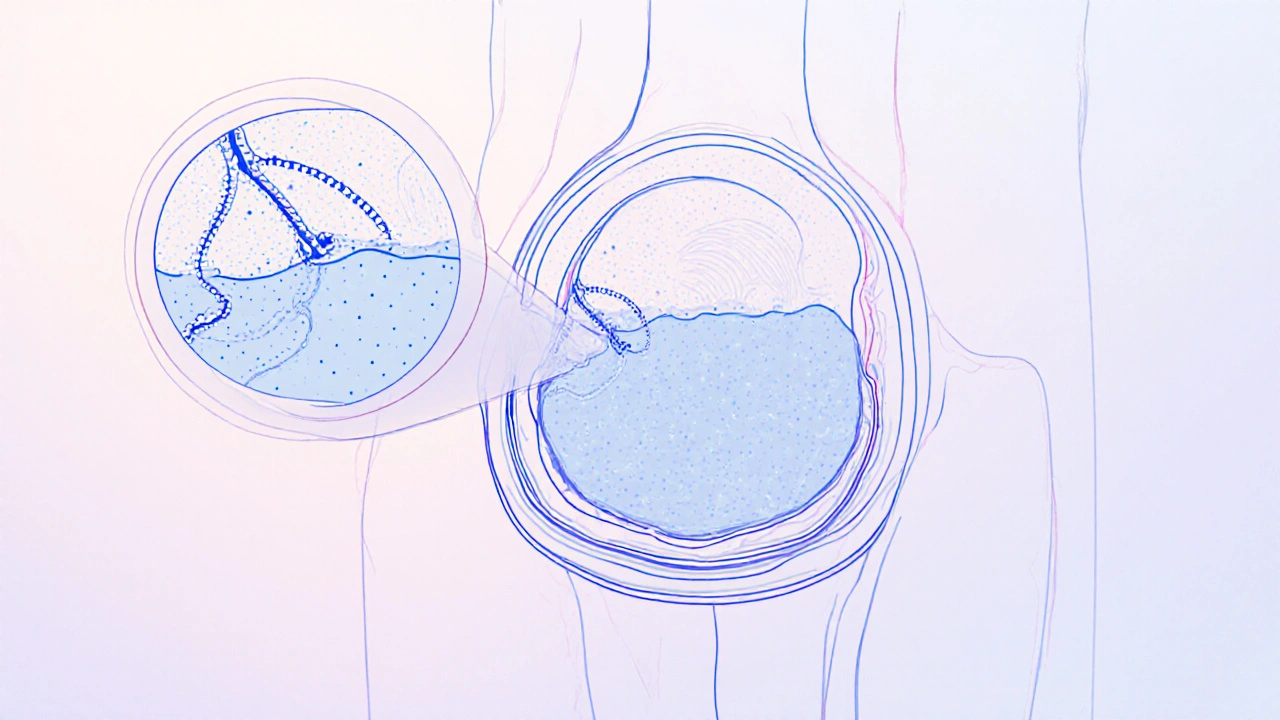
Understanding Penile Lymphedema
Penile lymphedema occurs when the lymphatic vessels that normally transport interstitial fluid back to the bloodstream become obstructed or damaged. Causes include trauma, infections, cancer treatments, or congenital malformations. The resulting fluid accumulation can thicken the dermis, create fibrotic tunnels, and impair erectile function.
Key signs include:
- Visible swelling that does not subside with elevation
- Hardening of the penile skin (peau d'orange appearance)
- Pain during intercourse or even at rest
- Recurring cellulitis or fungal infections
Why penile lymphedema surgery May Be Needed
Conservative therapy-manual lymphatic drainage, compression garments, and physiotherapy-helps in mild cases but often falls short when fibrotic tissue has formed. Persistent edema can lead to:
- Permanent loss of penile length
- Sexual dysfunction
- Psychological distress
Main Surgical Options
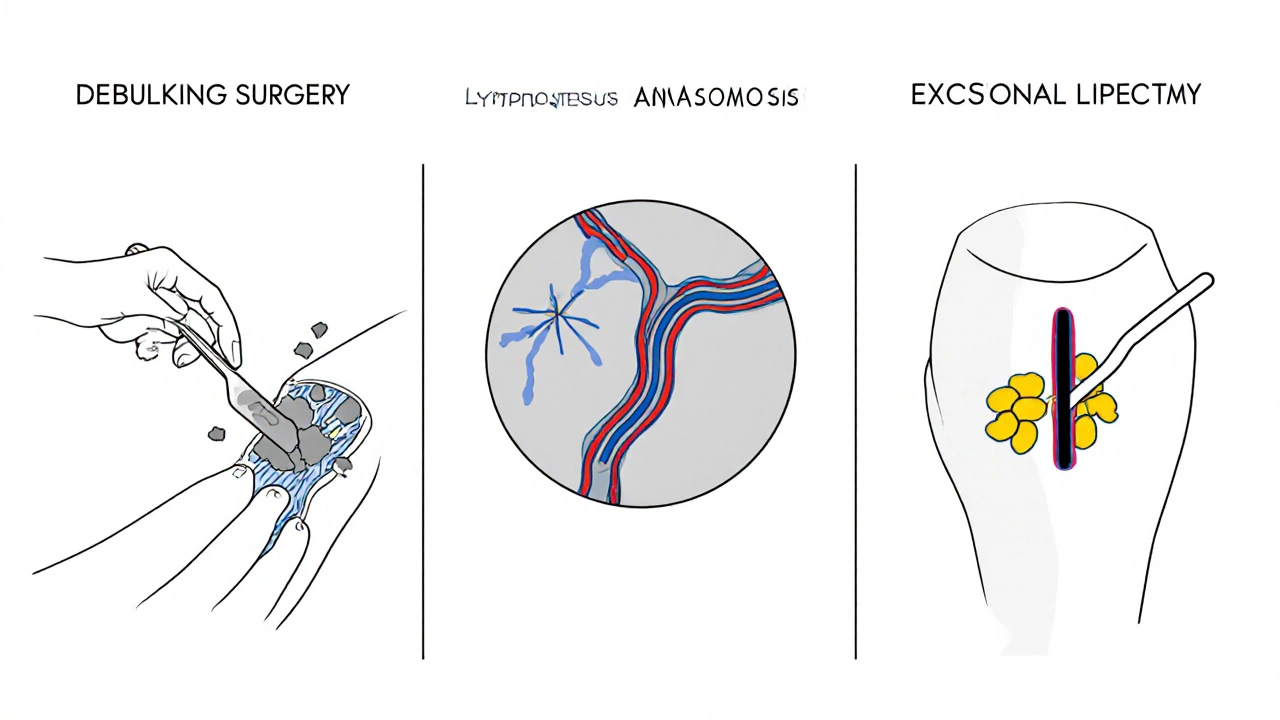
Three techniques dominate modern practice. Each targets a different stage of the disease and carries its own set of benefits.
| Procedure | Invasiveness | Typical Recovery | Success Rate* | Best For |
|---|---|---|---|---|
| Debulking Surgery | High | 6‑8 weeks | 70‑80% | Advanced fibrosis, large volume edema |
| Lymphovenous Anastomosis (LVA) | Moderate | 3‑4 weeks | 60‑70% | Early‑stage disease with patent vessels |
| Excisional Lipectomy | Moderate‑High | 4‑6 weeks | 65‑75% | Mixed edema + excess adipose tissue |
*Success rates reflect symptom reduction at 12‑month follow‑up in peer‑reviewed series (2023‑2024).
Debulking surgery removes the bulk of fibrotic and fatty tissue, reshaping the shaft. It’s often combined with skin grafts when extensive skin loss occurs.
Lymphovenous anastomosis (LVA) connects tiny lymphatic channels directly to nearby veins under a microscope, allowing fluid to bypass the blockage. This technique preserves anatomy and offers quicker return to activity.
Excisional lipectomy focuses on removing deep‑lying adipose deposits while sparing vital neurovascular bundles. It’s useful when obesity compounds lymphedema.
Choosing the Right Procedure
Selection hinges on three clinical variables:
- Stage of disease: Early stages favor LVA; late stages require debulking or lipectomy.
- Patient health: Microsurgical LVA needs a surgeon skilled in super‑microsurgery and a patient who can tolerate anesthesia for 2‑3 hours.
- Functional goals: Men prioritizing rapid return to sexual activity may lean toward LVA, while those needing maximal volume reduction may accept the longer downtime of debulking.
Consultations usually involve both a urologist and a microsurgeon. Imaging-lymphoscintigraphy or indocyanine green (ICG) fluorescence-helps map functional vessels, guiding the surgeon toward the most feasible option.
Pre‑ and Post‑Operative Care
Preparing for surgery isn’t just about fasting. Patients are advised to:
- Maintain a healthy weight (BMI < 30) to reduce postoperative swelling.
- Stop smoking at least two weeks prior-nicotine impairs micro‑vascular healing.
- Discuss anticoagulant use with the surgical team; many surgeons ask patients to pause blood thinners 5 days before.
After the operation, the recovery plan typically includes:
- Compression therapy: Custom‑fit penile wraps applied for 4‑6 weeks to support lymphatic channels.
- Physiotherapy: Gentle manual lymphatic drainage sessions 2‑3 times per week for the first month.
- Gradual re‑introduction of sexual activity-often after 6 weeks, once edema has subsided.
Follow‑up visits at 2 weeks, 6 weeks, and 3 months allow the surgeon to monitor wound healing, adjust compression, and assess functional outcomes.
Potential Risks and Complications
Like any operation, penile surgery carries risks. The most documented complications include:
- Infection: Reported in 5‑10% of cases; early antibiotics reduce this risk.
- Neurovascular injury: Damage to the dorsal nerves or arteries can affect sensation or erectile function. Skilled microsurgeons report <1% permanent loss.
- Scar contracture: Excessive scarring may re‑narrow the shaft, sometimes necessitating revision surgery.
- Persistent edema: Incomplete removal of lymphatic obstruction can lead to recurrence, especially if conservative measures aren’t continued.
Patients who follow post‑operative compression and physiotherapy protocols see markedly lower complication rates.

When Surgery Isn’t the Answer
If the edema is mild, recent, or linked to a reversible cause (e.g., medication side‑effects), doctors often start with:
- Manual lymphatic drainage performed by a certified therapist.
- Low‑stretch compression devices designed for the genital region.
- Weight‑management programs to reduce adipose pressure on lymphatics.
In some cases, a combined approach-initial conservative therapy followed by delayed surgery-optimizes outcomes, allowing the tissue to soften before an operation.
Bottom Line
Penile lymphedema is a challenging condition, but modern surgical options give men a realistic chance to regain comfort and sexual function. Selecting the right technique depends on disease stage, overall health, and personal goals. With diligent pre‑ and post‑operative care, most patients experience lasting improvement and a lower chance of recurrence.
Frequently Asked Questions
What causes penile lymphedema?
Common triggers include trauma to the groin, radiation therapy for pelvic cancers, infections such as cellulitis, and congenital abnormalities of the lymphatic vessels. Obesity can also compress lymphatic channels, worsening fluid buildup.
Can lifestyle changes reduce the swelling?
Yes. Maintaining a healthy weight, staying active, and avoiding prolonged sitting can improve lymphatic flow. Daily self‑massage and the use of loose, breathable underwear also help keep the area dry and less prone to infection.
How long does it take to see results after surgery?
Most patients notice a visible reduction in girth within 2‑4 weeks, with maximal remodeling occurring by 3‑6 months. Sexual function typically improves once swelling subsides and compression is tapered.
Is the surgery painful?
Pain is managed with short‑acting anesthesia and postoperative analgesics. Most men report mild discomfort that resolves within a week. Persistent sharp pain should be evaluated for nerve injury or infection.
Will I need additional procedures later?
A small percentage (≈10‑15%) may require a revision if edema recurs or scar tissue contracts. Ongoing compression and physiotherapy greatly reduce the need for repeat surgery.



Comments
Poornima Ganesan
Penile lymphedema, while uncommon, is often misunderstood by both patients and clinicians; the pathophysiology involves obstruction of the delicate lymphatic network, which leads to fluid stagnation and subsequent fibrotic remodeling. In practice, I have seen many men dismiss early swelling as a temporary issue, only to face irreversible changes later. The literature consistently emphasizes that early diagnostic imaging, such as ICG lymphangiography, can delineate viable channels and guide timely intervention. Moreover, the choice between debulking, LVA, or lipectomy is not arbitrary; it hinges on the stage of disease, comorbidities, and the patient's functional priorities. Ignoring the psychosocial impact, especially the loss of confidence, can undermine postoperative compliance with compression therapy. Therefore, a multidisciplinary approach that includes urologists, microsurgeons, and physiotherapists yields the best outcomes. Finally, patients should be counseled that even with optimal surgery, lifelong maintenance, including weight control and smoking cessation, remains essential.
October 18, 2025 AT 20:36
Emma Williams
Thanks for the thorough breakdown.
October 30, 2025 AT 12:13
Stephanie Zaragoza
The article correctly identifies the three primary surgical modalities; however, it could benefit from a more detailed risk stratification, particularly concerning neurovascular complications. Additionally, the success rates cited should be contextualized with the confidence intervals reported in the latest meta‑analyses. Moreover, the postoperative compression protocol seems oversimplified; individual variability in tissue compliance often necessitates adjustments. Finally, a brief discussion on the role of adjunctive physiotherapy would enhance the comprehensiveness of the piece.
November 11, 2025 AT 04:50
Mike Hamilton
From a cultural perspective, it's interesting how different countries approach penile surgery. In some places, the stigma around lymphedema is huge, which can delay seeking help. Also, the belief that natural remedies work sometimes hinders acceptance of microsurgery.
November 22, 2025 AT 21:27
Liberty Moneybomb
Honestly, I think the medical establishment is hiding the truth about these procedures! They want you to believe surgery is the only option, while secret therapies exist that can reverse lymphedema without any cuts. It's all a cover‑up to keep the pharmaceutical profits flowing, and patients are left in the dark, suffering in silence.
December 4, 2025 AT 14:04
Fabian Märkl
Great info! If you're considering any of these surgeries, stay positive and follow the rehab plan-your body will thank you! 😄💪
December 16, 2025 AT 06:41
Natala Storczyk
Patriots must recognize that our national health system should prioritize these life‑changing surgeries, NOT waste resources on frivolous cosmetics! It’s an affront to our heritage when men suffer because the government delays proper treatment; we demand immediate, unrestricted access, and we won’t tolerate any bureaucratic roadblocks!
December 27, 2025 AT 23:18
nitish sharma
Esteemed colleagues, I would like to extend my sincere gratitude for the comprehensive overview presented herein. It is imperative that we maintain the highest standards of postoperative care, especially concerning compression protocols. Kindly ensure that all patient education materials are reviewed for clarity and cultural sensitivity. I remain at your disposal for any further scholarly discourse.
January 8, 2026 AT 15:55
Karla Johnson
When examining the spectrum of surgical interventions for penile lymphedema, it becomes evident that each technique carries its own nuanced set of indications, benefits, and potential drawbacks, thereby necessitating a patient‑centered decision‑making process that incorporates both anatomical considerations and personal preferences. First, debulking surgery, which involves the excision of extensive fibrotic tissue, offers the most dramatic reduction in penile girth, yet it also imposes the longest convalescence period, typically ranging from six to eight weeks, during which patients must adhere to strict compression therapy and limit sexual activity. Second, lymphovenous anastomosis (LVA) presents a minimally invasive alternative that preserves native tissue architecture by connecting lymphatic channels directly to adjacent veins under high magnification; this method often results in a quicker return to functional status, generally within three to four weeks, but its success is contingent upon the presence of patent lymphatics, a condition more frequently observed in early‑stage disease. Third, excisional lipectomy targets the removal of deep adipose deposits, offering a balance between volume reduction and tissue preservation, yet it demands meticulous dissection to avoid compromise of the neurovascular bundles that are critical for erectile function. Moreover, patient factors such as body mass index, smoking status, and comorbidities like diabetes must be meticulously optimized preoperatively, as they influence wound healing and overall surgical outcomes. Imaging modalities, including lymphoscintigraphy and indocyanine green (ICG) fluorescence, provide valuable intraoperative guidance, enabling surgeons to map functional lymphatic pathways and tailor the operative plan accordingly. Postoperative protocols universally emphasize the importance of custom‑fit compression garments, scheduled manual lymphatic drainage sessions, and gradual reintroduction of sexual activity, typically after six weeks, to ensure sustained symptom alleviation. It is also essential to schedule follow‑up visits at two, six, and twelve weeks post‑surgery to monitor for complications such as infection, hematoma, or neurovascular injury, which, while relatively infrequent, can have profound implications on patient quality of life if unaddressed promptly. In conclusion, the optimal surgical choice hinges upon a comprehensive assessment of disease stage, patient health, and individual goals, with a multidisciplinary team approach fostering the best possible functional and aesthetic results.
January 20, 2026 AT 08:32
Joe Moore
Wow, you just read that whole thing and think it's all legit? The real agenda is hidden, they're calibrating the lasers to trap our DNA while we think they're just fixing swelling. Wake up!
February 1, 2026 AT 01:09
Ayla Stewart
I appreciate the thoroughness of the earlier explanation, though I wonder if more emphasis could be placed on pre‑operative counseling to manage expectations around recovery timelines.
February 12, 2026 AT 17:46
Rajesh Singh
The moral imperative here is crystal clear: we must champion every man battling this condition, lest we become complicit in a system that trivializes suffering. When physicians sidestep the deeper psychosocial wounds, they're not just treating tissue-they're neglecting the soul.
February 24, 2026 AT 10:22