Acetaminophen Toxicity: Signs, Risks, and What to Do If You’ve Taken Too Much
When you take acetaminophen, a common pain and fever reducer found in over 600 medications, including Tylenol and many cold and flu combos. Also known as paracetamol, it’s one of the safest drugs when used correctly—but it’s also the leading cause of acute liver failure in the U.S. and Europe. You don’t need to swallow a whole bottle to cause harm. Just going over the daily limit—4,000 milligrams for most adults—can trigger serious damage, especially if you drink alcohol, have liver disease, or take multiple products that contain it.
Liver damage, the primary risk of acetaminophen toxicity, happens because the body turns the drug into a toxic byproduct when too much is present. Normally, your liver handles this safely. But when overwhelmed, it can’t detoxify fast enough, and liver cells start dying. This isn’t like a stomach bug—it often has no symptoms at first. By the time nausea, vomiting, or right-side abdominal pain show up, the damage may already be advanced. That’s why N-acetylcysteine, the antidote for acetaminophen overdose, works best when given within 8 hours. After 24 hours, its effectiveness drops sharply. Emergency rooms use blood tests to measure acetaminophen levels and liver enzymes like ALT and AST to confirm toxicity.
Many people don’t realize they’re at risk because they’re taking more than one product with acetaminophen. A cold medicine, a sleep aid, and a pain reliever—all can add up. Even a single extra-strength Tylenol tablet contains 500 mg. Four of those in a day is already half the limit. And if you’ve had a few drinks? That threshold drops to just 2,000 mg. The FDA now requires warning labels on OTC products, but confusion still runs high. What’s worse, some people think "natural" or "non-prescription" means safe in any dose. It doesn’t.
If you suspect an overdose—even if you feel fine—call poison control or go to the ER. Don’t wait for symptoms. N-acetylcysteine can save your liver if given early. And if you’re on chronic pain meds, talk to your doctor about alternatives. There are safer ways to manage pain, especially if you drink alcohol or have liver issues. The posts below cover real cases, hidden risks in common meds, how to read labels correctly, and what to do if you’ve accidentally doubled up. You’ll find practical advice from people who’ve been there, and clear guidance to help you avoid the same mistake.
- Colin Hurd
- Dec, 3 2025
- 13 Comments
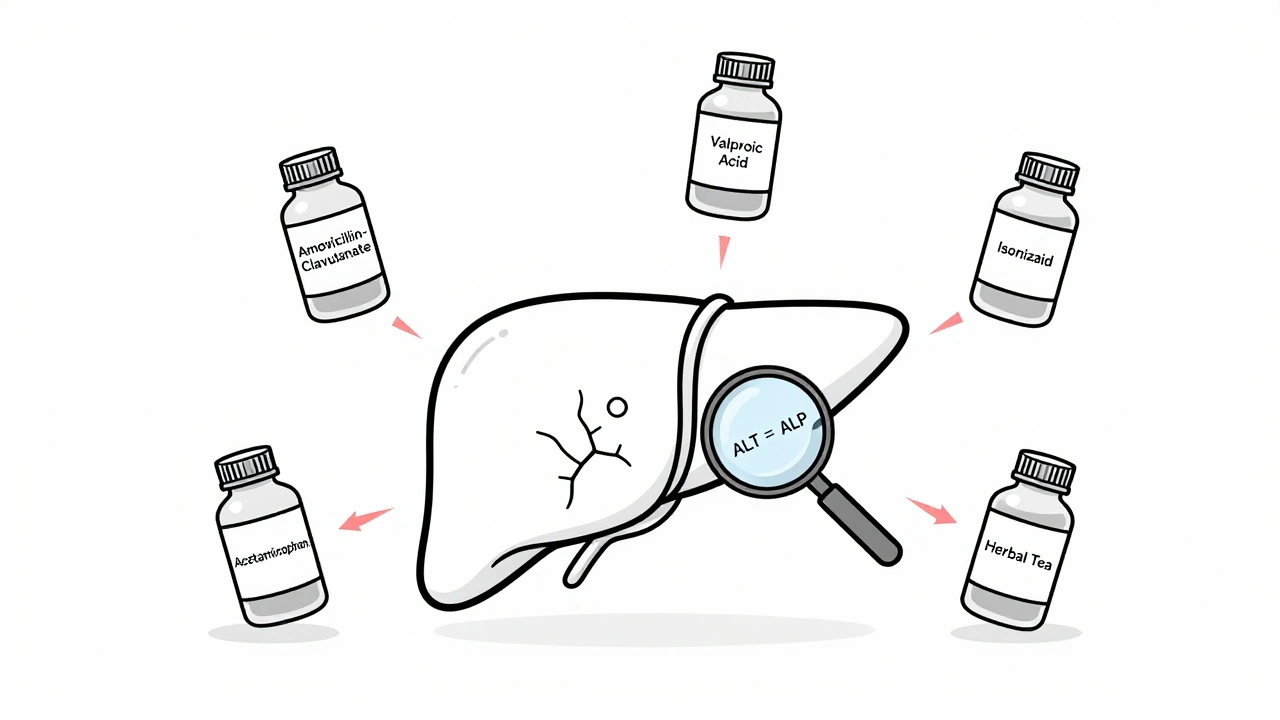
Drug-Induced Liver Injury: High-Risk Medications and How to Monitor Them
Drug-induced liver injury can be caused by common medications and supplements. Learn which drugs carry the highest risk, how to spot early signs, and what monitoring steps can prevent serious liver damage.