Dexamethasone: Uses, Dosage, and Safety
When you see dexamethasone listed on a prescription, it’s helpful to know exactly what you’re dealing with. dexamethasone, a synthetic glucocorticoid that reduces inflammation and suppresses the immune system. Also known as Decadron, it is a cornerstone in modern medicine. Corticosteroids form the broader drug class, and dexamethasone sits near the top because of its high potency. As an anti‑inflammatory drug, it works by blocking the release of cytokines that cause swelling and pain. At the same time, it functions as an immunosuppressant, which is why doctors rely on it for conditions where the immune system overreacts, such as severe allergies or organ transplant rejection. In short, dexamethasone encompasses the power of corticosteroids, the relief of anti‑inflammatory agents, and the control of immunosuppressive therapy.
Because of its versatility, dexamethasone shows up in treatment plans for a wide range of diseases. During the COVID‑19 pandemic, it became a standard of care for patients needing oxygen support, demonstrating that a single molecule can shift outcomes in a global health crisis. Rheumatologists prescribe it for rheumatoid arthritis flares, while pulmonologists use it for acute asthma attacks that don’t respond to inhalers. Oncologists rely on high‑dose regimens to curb chemotherapy‑induced nausea and to treat certain blood cancers. The drug is available as oral tablets, injectable solutions, eye drops, and even intrathecal formulations for spinal administration. Each dosage form carries its own set of dosing rules: a 4 mg tablet for mild inflammation, a 10‑mg injection for rapid control of severe edema, or a 0.1 % eye drop for ocular inflammation. Knowing which form to use and how to adjust the dose is crucial, because the same drug can act differently depending on the route of delivery and the condition being treated.
With great power comes a need for caution. Dexamethasone’s side‑effect profile reflects its strong glucocorticoid activity. Short‑term use can cause elevated blood sugar, mood swings, or insomnia, while long‑term therapy may lead to osteoporosis, cataracts, and adrenal suppression. Because the body’s own cortisol production can shut down when dexamethasone is taken for weeks or months, doctors always recommend a tapering schedule rather than an abrupt stop. Monitoring parameters include blood glucose levels, bone density scans, and regular eye exams. Patients with uncontrolled infections, uncontrolled diabetes, or a history of psychosis should discuss alternatives before starting therapy. By understanding the relationship between dexamethasone, its corticosteroid class, and its anti‑inflammatory and immunosuppressive actions, you can weigh the benefits against the risks and make an informed decision with your healthcare provider. Below you’ll find a curated collection of articles that dive deeper into specific uses, dosage strategies, and safety considerations, giving you practical insights to apply right away.
- Colin Hurd
- Oct, 24 2025
- 14 Comments
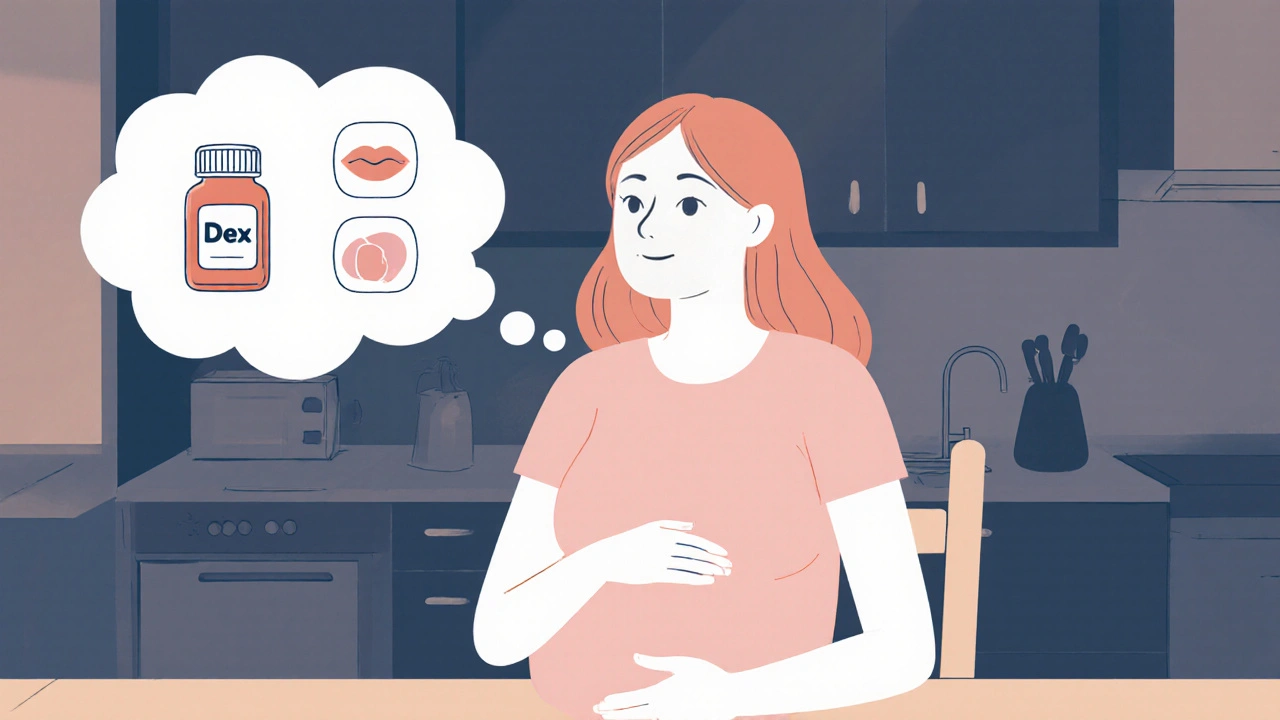
Dexamethasone Use During Pregnancy: Risks, Benefits, and Guidelines
A clear guide on dexamethasone use during pregnancy, covering risks, benefits, dosage timing, maternal side effects, and practical tips for expecting mothers.