Drug Pricing: Why Medications Cost What They Do and How to Save
When you pick up a prescription, the price can feel random—sometimes it’s a few dollars, other times it’s over $500. That’s because drug pricing, the system that determines how much pharmaceutical companies charge for medications. Also known as pharmaceutical cost structure, it’s shaped by patents, manufacturing, regulation, and market control—not just how much it costs to make the pill. You’re not just paying for ingredients. You’re paying for research, legal battles, marketing, and the time it takes to get approval from the FDA.
One of the biggest drivers of price differences is the gap between brand-name drugs, medications sold under a company’s original trademark after years of development. Also known as innovator drugs, they’re protected by patents that block competitors for up to 20 years. Once those patents expire, generic drugs, medications that contain the same active ingredient as brand-name drugs but are sold at a fraction of the cost. Also known as off-patent drugs, they enter the market and drop prices by 80% or more—without sacrificing safety or effectiveness. The FDA requires generics to match brand-name drugs in strength, dosage, and how they work in your body. The only difference? No expensive clinical trials. No fancy packaging. No ads on TV. That’s why a 30-day supply of generic lisinopril might cost $4, while the brand version, Zestril, could run $150.
But drug pricing isn’t just about generics versus brands. It’s also about pharmaceutical costs, the full chain of expenses that go into bringing a drug to market—from lab research to distribution. Also known as drug development costs, these include everything from failed experiments to legal fees for patent extensions. Some companies raise prices on older drugs with no competition, even if the cost to produce them hasn’t changed. Others charge high prices for new specialty drugs—like cancer treatments or rare disease therapies—because there’s little pressure to lower them. And while the U.S. spends more per person on drugs than any other country, countries like Canada and the UK negotiate prices directly with makers, keeping costs down.
What you’ll find in these posts isn’t just theory—it’s real, practical insight. You’ll learn how the Hatch-Waxman Act opened the door for affordable generics, why some drugs stay expensive even after patents expire, and how blockchain and refill sync programs are helping patients avoid overpaying. You’ll see how drug-induced liver injury, statin side effects, and insulin regimens all tie into the bigger picture of cost and access. Whether you’re managing diabetes, fighting high blood pressure, or just trying to stretch your prescription budget, this collection gives you the facts you need to ask better questions, make smarter choices, and stop paying more than you have to.
- Colin Hurd
- Dec, 4 2025
- 12 Comments
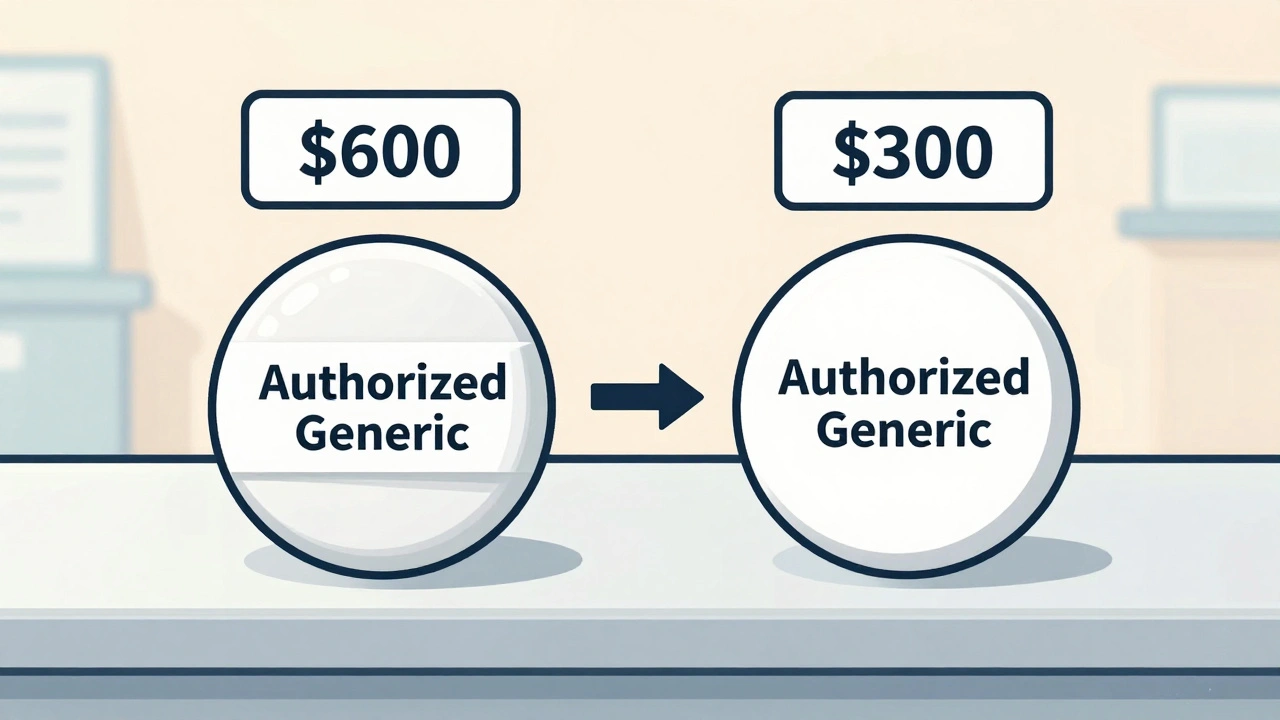
Authorized Generic Pricing: Why They Cost Less Than Brand Name Drugs
Authorized generics cost less than brand-name drugs because they're the exact same medication made by the original manufacturer-just without the brand name. Learn why they're cheaper and how to save on prescriptions.