Functional Bowel Disorder: Causes, Symptoms, and What You Can Do
When your gut acts up—bloating, cramps, diarrhea, or constipation—but tests come back normal, you might be dealing with a functional bowel disorder, a group of digestive conditions where the gut doesn’t work right, even though no structural damage is found. Also known as irritable bowel syndrome (IBS), it’s not in your head, and it’s not just "stress." It’s a real, measurable disruption in how your gut and brain talk to each other.
This isn’t just about occasional upset stomachs. People with functional bowel disorder often live with symptoms for years, and many get misdiagnosed as having food allergies, celiac disease, or even anxiety. The truth? It’s a disorder of gut-brain interaction. Your nervous system overreacts to normal digestion. Food moves too fast or too slow. Your intestines become hypersensitive. And while stress doesn’t cause it, it sure makes it worse. You might notice flare-ups after big life events, poor sleep, or even certain foods—like dairy, beans, or artificial sweeteners.
What’s interesting is how closely this connects to other conditions you might not expect. For example, restless legs syndrome, a condition tied to low iron levels, often shows up alongside digestive issues. Same with ferritin levels, a key marker for iron storage—low levels can worsen both gut motility and nerve sensitivity. And while we’re talking about the gut, it’s worth noting that many people with functional bowel disorder also struggle with medication adherence, because symptoms make daily routines unpredictable. Taking pills on time gets harder when you’re not sure when you’ll need the bathroom.
There’s no single test to confirm functional bowel disorder. Doctors rule out other things first—like infections, celiac disease, or colon cancer. That’s why so many people go years without answers. But once you know what you’re dealing with, you can start managing it. Simple changes—like tracking triggers, adjusting fiber intake, or trying low-FODMAP diets—help more than most people realize. And unlike some chronic conditions, this one doesn’t require lifelong drugs. Many find relief through gut-directed hypnotherapy, regular movement, or even probiotics that actually work.
What you’ll find in the posts below isn’t a list of miracle cures. It’s real talk from people who’ve been there: how to spot hidden triggers, what supplements actually help (and which ones are a waste), how gut health ties into sleep and mood, and why some medications make it worse. You’ll see how functional bowel disorder connects to things like stress, iron levels, and even how you store your pills at home. No fluff. No jargon. Just what works—and what doesn’t—based on real experience and science.
- Colin Hurd
- Dec, 4 2025
- 11 Comments
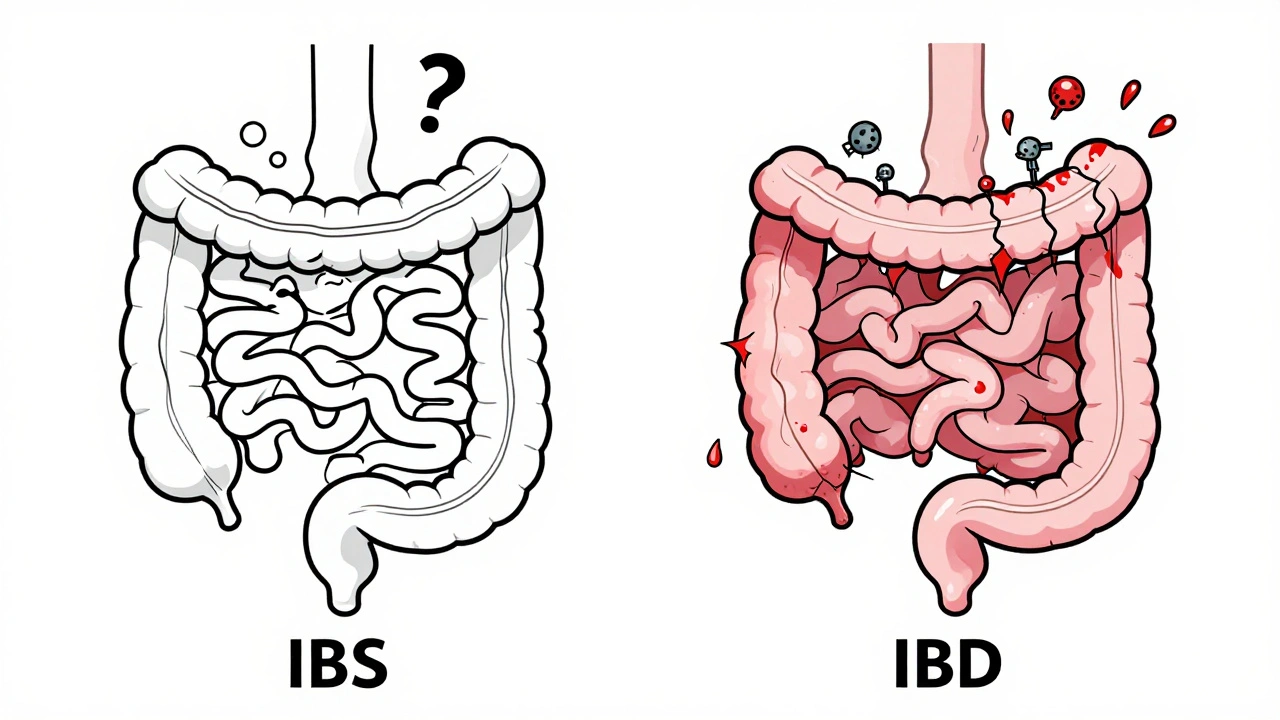
IBS vs. IBD: What’s the Real Difference Between Functional and Inflammatory Bowel Disorders?
IBS and IBD look similar but are completely different. IBS is a functional disorder with no physical damage; IBD causes chronic inflammation and bowel damage. Learn the key symptoms, tests, and treatments that set them apart.