Lymphovenous Anastomosis – What It Is and Why It Matters
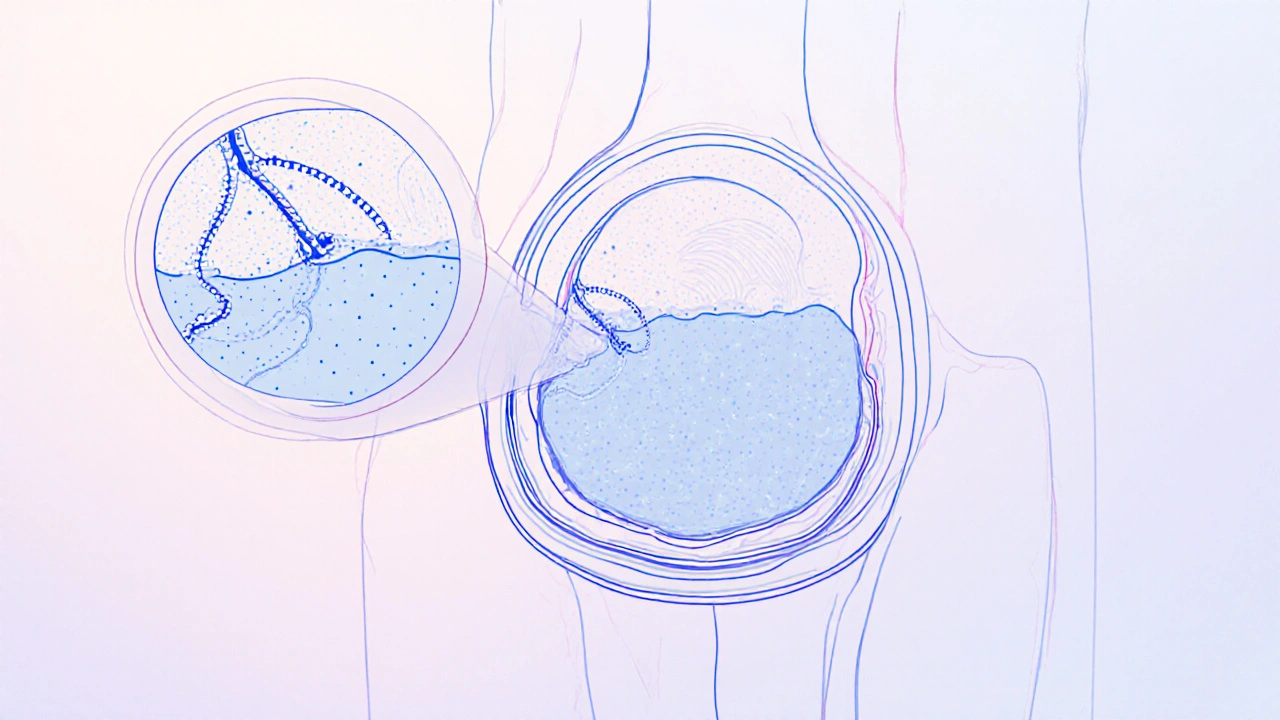
When working with lymphovenous anastomosis, a microsurgical technique that connects lymphatic vessels directly to nearby veins to reroute excess fluid. Also known as LVA, it targets the root cause of lymphedema, a chronic swelling condition caused by impaired lymph drainage. By creating these tiny bypasses, surgeons aim to reduce swelling, prevent skin changes, and improve quality of life. Lymphovenous anastomosis therefore bridges the gap between the lymphatic and venous systems, offering a minimally invasive alternative to compression garments and extensive physiotherapy.
Key Players and Techniques Behind Successful LVA
A successful LVA program relies on several supporting concepts. First, supermicrosurgery, the use of ultra‑fine instruments and high‑magnification optics to handle vessels under 0.8 mm is the skill set that makes LVA possible. Without supermicrosurgical expertise, the anastomoses would be too fragile to stay open. Second, lymphatic mapping, imaging methods such as indocyanine green (ICG) fluorescence to locate functional lymphatics guides the surgeon to the best vessels for connection. Third, the procedure often incorporates microsurgical instruments, specialized microscopes, micro‑forceps, and sutures designed for sub‑millimeter work, ensuring precision and durability of the new pathways. Together, these entities form a workflow where LVA requires supermicrosurgery skill, depends on accurate lymphatic mapping, and is executed with dedicated microsurgical tools.
Patients considering LVA typically have chronic lymphedema that hasn’t responded to compression or manual therapy. They can expect a brief outpatient operation, followed by a short recovery period and a gradual reduction in limb volume over weeks to months. Because the procedure restores natural fluid flow, many report fewer infections and less reliance on bandaging. The literature shows that when LVA is combined with post‑operative physiotherapy, the reduction in swelling can exceed 30 % in some cases. As the field evolves, clinicians are also exploring hybrid approaches that pair LVA with vascularized lymph node transfer for even greater outcomes. Below you’ll find a curated list of articles that dive deeper into each of these aspects – from the science behind supermicrosurgery to practical tips for post‑op care – giving you a comprehensive view of what lymphovenous anastomosis can achieve.
- Colin Hurd
- Oct, 18 2025
- 12 Comments
Surgical Treatments for Penile Lymphedema: Options, Risks, and Recovery
Explore why surgery is often essential for penile lymphedema, the main procedures available, risks, recovery steps, and when non‑surgical options may suffice.