Penile Lymphedema: Understanding Causes, Symptoms, and Care
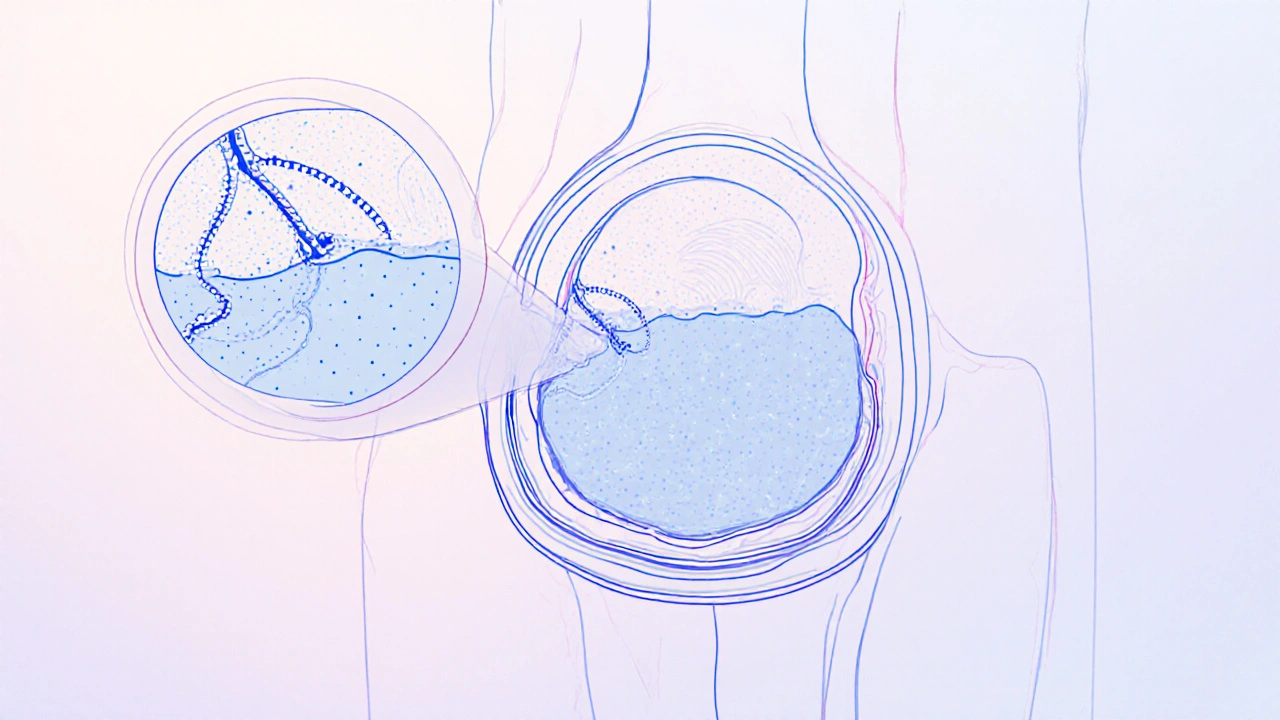
When dealing with Penile Lymphedema, a buildup of lymph fluid in the penile tissue that causes noticeable swelling, heaviness, and sometimes pain. Also known as penile swelling from lymphatic blockage, it reflects a failure in the lymphatic system, the network that transports fluid, proteins, and immune cells throughout the body. This condition is a localized form of lymphedema, which can affect arms, legs, or other areas when drainage pathways are damaged or overloaded. The core issue is that lymph cannot return to circulation, so it pools in the penile tissue, stretching the skin and creating a visible enlargement.
The most common triggers for penile lymphedema are surgical interventions in the pelvic region, especially radical prostatectomy or bladder surgery, where lymph nodes are removed or radiated. Trauma, infections such as cellulitis, or chronic venous insufficiency can also impair drainage. In rare cases, parasitic infections like filariasis block lymph channels, leading to persistent swelling. Recognizing the problem early matters: patients often notice a gradual increase in girth, a feeling of tightness, or difficulty with urination. Physical examination typically reveals non‑pitting edema—meaning the swollen area does not indent under pressure—which distinguishes lymphedema from simple fluid overload.
Treatment revolves around restoring lymph flow and preventing fibrosis. Manual lymphatic drainage (MLD) performed by a certified therapist is the cornerstone; gentle, rhythmical strokes stimulate the remaining pathways and move fluid toward healthy nodes. Compression therapy—using specially fitted wraps or garments—helps maintain the gains achieved by massage and reduces re‑accumulation. Adjuncts such as decongestive physiotherapy, low‑impact exercise, and pneumatic compression devices support the process. In cases linked to surgery, doctors may consider prophylactic lymphatic‑preserving techniques or prescribe short‑term diuretics to manage acute swelling, though diuretics alone rarely solve chronic lymphedema. Patient education on skin care is crucial; keeping the area clean prevents infections that could worsen the condition.
Accurate diagnosis often involves imaging studies like lymphoscintigraphy, which maps the flow of a radiotracer through the lymphatic channels, or MRI to rule out other masses. Blood tests may be ordered to check for infection or inflammatory markers. Once the underlying cause is identified, a personalized plan—combining MLD, compression, lifestyle tweaks, and, when needed, surgical debulking or lymphatic reconstruction—is put in place. The goal is to reduce swelling, improve comfort, and preserve sexual function. Below you’ll find a curated selection of articles that dive deeper into each of these aspects, from detailed guides on manual drainage techniques to the latest research on surgical options and patient‑reported outcomes. Explore the resources to get practical steps you can start using today.
- Colin Hurd
- Oct, 18 2025
- 12 Comments
Surgical Treatments for Penile Lymphedema: Options, Risks, and Recovery
Explore why surgery is often essential for penile lymphedema, the main procedures available, risks, recovery steps, and when non‑surgical options may suffice.