Serotonergic Overlap: Understanding the Interplay of Serotonin‑Targeting Medications
When exploring serotonergic overlap, the situation where two or more drugs affect the brain’s serotonin system at the same time, you quickly see why it matters for everyday prescribing. Think of Selective Serotonin Reuptake Inhibitor (SSRI), a class of antidepressants that block serotonin re‑uptake like Paroxetine or Zoloft. Pair those with another serotonergic agent—say a migraine medicine, an anti‑nausea drug, or even a herbal supplement—and you land in the realm of serotonin syndrome, a potentially life‑threatening response caused by excess serotonin. The same principle drives many drug interactions, unintended effects when two substances influence each other’s metabolism or receptors. For patients with PTSD, where SSRIs are a first‑line therapy, understanding these overlaps can change the difference between relief and serious side effects.
Why the Overlap Happens: Pharmacology in Plain Terms
Serotonin is a messenger that helps regulate mood, pain, sleep, and gut function. Any drug that raises serotonin levels—whether by blocking re‑uptake (SSRIs), stimulating release (certain migraine treatments), or inhibiting breakdown (MAO‑B inhibitors)—contributes to the overall serotonergic load. When the load exceeds the brain’s capacity to manage it, the system tips into syndrome territory. This is a classic subject‑predicate‑object triple: Serotonergic overlap causes serotonin syndrome. Another triple links treatment intent: SSRIs treat PTSD, but SSRIs interact with other serotonergic drugs. Those connections are why clinicians ask patients about over‑the‑counter meds, herbal teas, and even diet supplements.
Genetic factors add another layer. Some people carry variants of the CYP2D6 or CYP3A4 enzymes that process many antidepressants. If a patient’s liver works slower, the drug stays in the bloodstream longer, raising serotonin levels even without a second drug. That explains why two patients on the same dose of Paroxetine can have totally different experiences—one might feel better, the other could develop a mild tremor or, in rare cases, full‑blown serotonin syndrome. The triple Genetic variation modulates serotonergic overlap outcomes captures this nuance.
Clinical guidelines therefore advise a “start low, go slow” approach when adding a new serotonergic agent to an existing SSRI regimen. Monitoring for early signs—agitation, hyperreflexia, sweating, diarrhea—can catch the problem before it escalates. This precautionary step mirrors the triple Physician monitoring prevents serotonin syndrome. It also highlights the role of patient education: knowing what symptoms to watch for turns a passive prescription into an active safety net.
Beyond the classic SSRI‑MAOI combo, several less obvious pairings show up in real‑world practice. For example, the anti‑emetic Ondansetron blocks serotonin receptors in the gut, yet it can still add to the serotonergic burden when used with an SSRI. Similarly, some herbal products like St. John’s Wort act as weak serotonin re‑uptake inhibitors and can tip the balance. These examples illustrate the triple Non‑prescription serotonergic agents contribute to serotonergic overlap. The key takeaway is that “prescription‑only” does not equal “safe‑only.”
Patients with chronic pain often receive tramadol, a weak opioid that also boosts serotonin and norepinephrine. When tramadol meets an SSRI, the combined effect can be enough to provoke syndrome, especially in older adults with reduced kidney function. The triple Tramadol + SSRI increases risk of serotonin syndrome is well documented in emergency department data. This is why many pain specialists now prefer non‑serotonergic opioids for patients already on antidepressants.
In the mental health arena, the overlap is a double‑edged sword. While SSRIs are first‑line for PTSD, they are also used off‑label for anxiety, obsessive‑compulsive disorder, and even certain sleep disorders. Adding a second serotonergic drug—like a supplement containing 5‑HTP—to address insomnia can unintentionally push serotonin levels into the dangerous zone. The triple Polypharmacy in mental health creates serotonergic overlap challenges captures this dilemma. Proper medication reconciliation at each visit helps clinicians untangle these webs.
All of these nuances set the stage for the collection of articles you’ll find below. We’ve gathered practical guides on Paroxetine for PTSD, safety tips for using Zoloft, drug‑interaction checklists, and real‑world case studies on serotonin syndrome. Whether you’re a patient looking to understand your prescription or a health‑care professional seeking a quick refresher, the posts ahead break down the science into actionable steps you can apply right away.
- Colin Hurd
- Oct, 25 2025
- 11 Comments
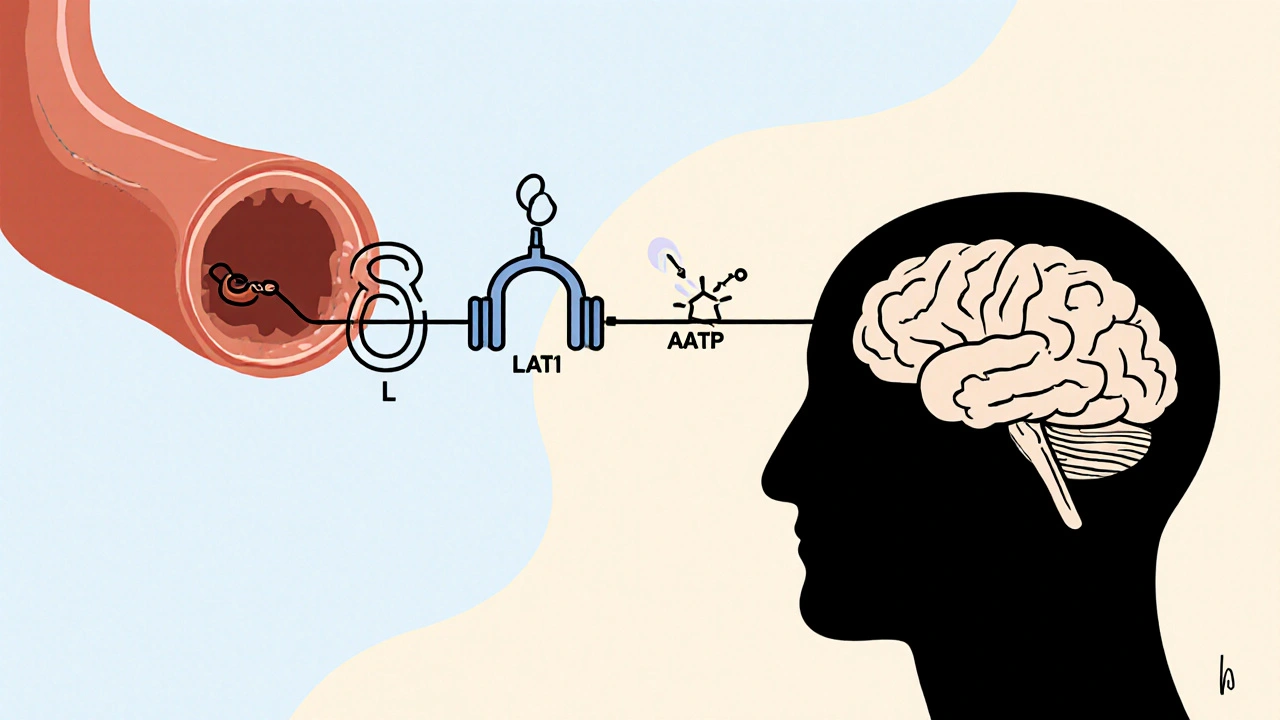
L‑Tryptophan & Antidepressants: Overlap, Risks & Safe Use
A clear guide on how L‑tryptophan interacts with antidepressants, covering serotonin overlap, safety limits, clinical evidence, and practical dosing tips.