Why ACE Inhibitors Are Contraindicated in Renal Artery Stenosis
- Colin Hurd
- 4 January 2026
- 15 Comments
ACE Inhibitor Risk Calculator for Renal Artery Stenosis
How This Calculator Works
Based on clinical guidelines, this tool estimates the potential impact of ACE inhibitors on kidney function based on stenosis type and kidney health factors. Remember: This is a general estimate and should not replace clinical judgment.
Enter Your Information
Key Facts to Know
Research shows:
- 18.7% of patients with undiagnosed bilateral stenosis develop acute kidney injury when starting ACE inhibitors
- 25-30% GFR drop typically occurs within 7-10 days of starting treatment
- Up to 20% of patients with bilateral stenosis experience significant kidney damage
Risk Assessment Results
When your kidneys don’t get enough blood flow, your body tries to compensate by ramping up a hormone system called the renin-angiotensin-aldosterone system (RAAS). This system tightens blood vessels and raises blood pressure to keep the kidneys working. But if you’re taking an ACE inhibitor - a common blood pressure drug - and you have narrowed arteries leading to one or both kidneys, this natural compensation gets shut down. And that’s when things can go wrong, fast.
What Happens When Blood Flow to the Kidneys Is Low?
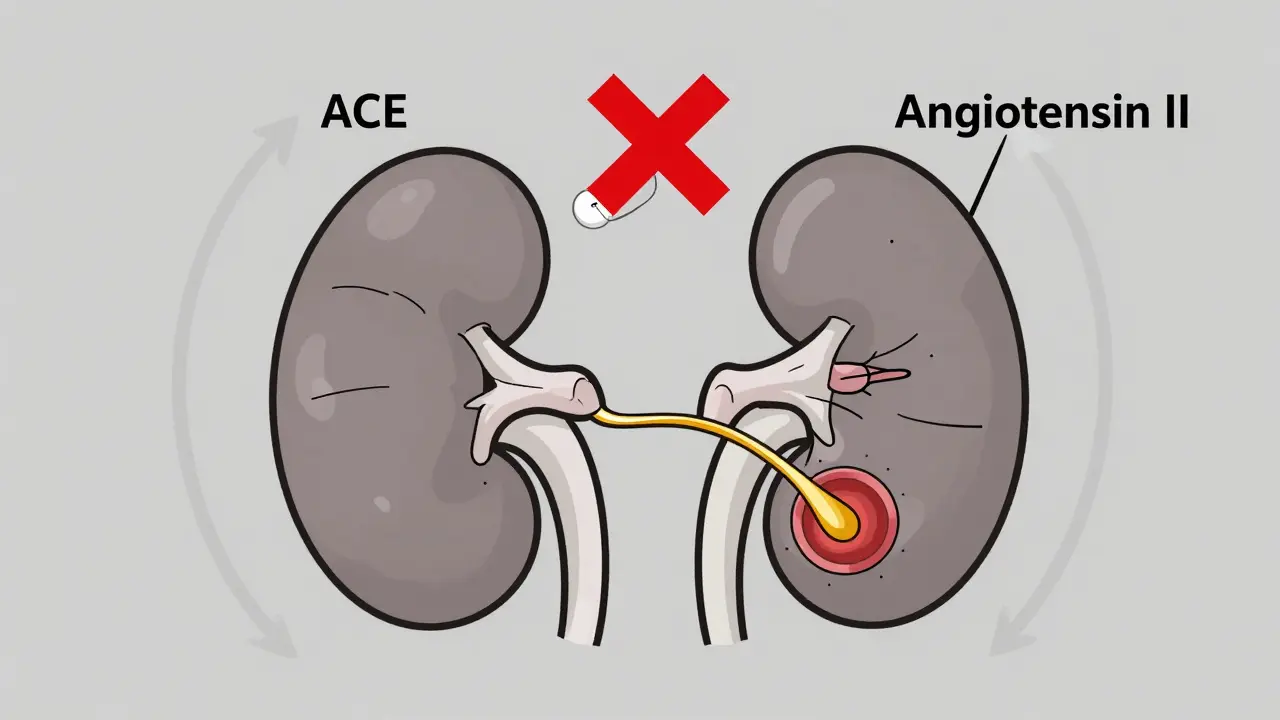
Renal artery stenosis means one or both of the arteries supplying your kidneys are narrowed, often by plaque buildup (atherosclerosis) or fibromuscular dysplasia. When this happens, the kidney thinks your whole body is low on blood pressure. In response, it releases renin, which triggers a chain reaction: angiotensin I turns into angiotensin II, a powerful vasoconstrictor. Angiotensin II doesn’t just raise blood pressure - it specifically tightens the efferent arteriole, the tiny blood vessel that drains blood from the filtering unit of the kidney (the glomerulus).
This tightening is critical. It keeps pressure high inside the glomerulus, so even with low blood flow, the kidney can still filter waste. Without that pressure, filtration drops. Think of it like a garden hose with a kink. If you squeeze the end, water still sprays out with force. But if you release the squeeze, the spray stops. That’s what angiotensin II does - it keeps the squeeze on.
How ACE Inhibitors Disrupt This Balance
ACE inhibitors block the enzyme that turns angiotensin I into angiotensin II. That’s great for most people - it lowers blood pressure, protects the heart, and slows kidney damage in diabetes. But in someone with renal artery stenosis, blocking angiotensin II removes that vital squeeze on the efferent arteriole. The result? A sudden drop in pressure inside the glomerulus. Glomerular filtration rate (GFR) plummets - often by 25% to 30% - within days.
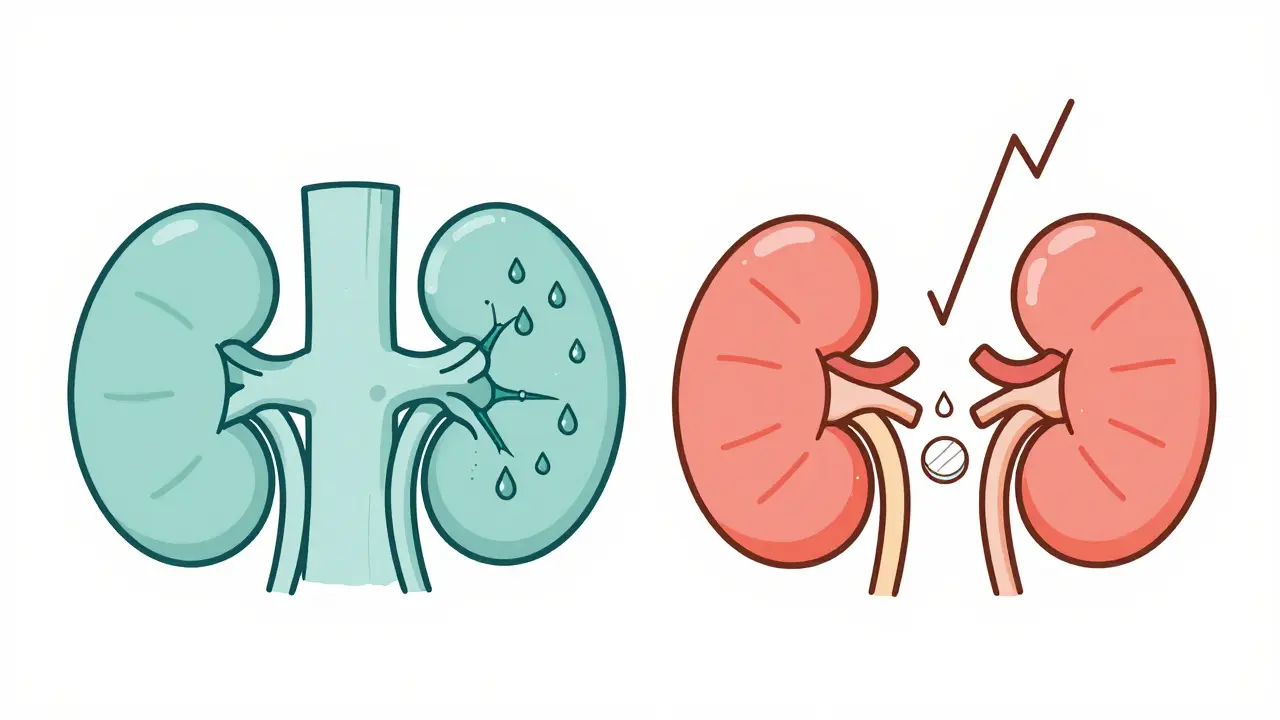
This isn’t just a lab number. It shows up as a sharp rise in serum creatinine, usually within 7 to 10 days of starting the drug. If creatinine jumps more than 30% from baseline, it’s a red flag. In some cases, especially with bilateral stenosis, kidney function can crash so hard that dialysis becomes necessary.
Bilateral vs. Unilateral: Why It Matters
Not all renal artery stenosis is the same. If you have stenosis in both kidneys - or just one kidney because the other is gone - ACE inhibitors are a hard no. Your body has no backup. The moment you block angiotensin II, your kidneys lose their last tool to maintain filtration.
But if you have stenosis in just one kidney and the other one is healthy, things are different. The good kidney can pick up the slack. Studies like the 2017 ASTRAL trial follow-up show that in this group, ACE inhibitors don’t cause significant long-term harm. One study found the average decline in eGFR was just -2.1 mL/min/1.73m² in patients on ACE inhibitors, nearly identical to those not taking them.
That’s why doctors might still prescribe ACE inhibitors if you have unilateral stenosis - but only if they’re watching your kidney function closely. The key is knowing which kidney is affected.
What the Guidelines Say
Every major guideline agrees: ACE inhibitors are contraindicated in bilateral renal artery stenosis or stenosis in a solitary kidney. The FDA, the American Heart Association, the European Society of Cardiology, and KDIGO all list it as a black-box warning. The Enalapril package insert says it outright: “Significant bilateral renal artery stenosis or renal artery stenosis in a single functioning kidney” is a contraindication.
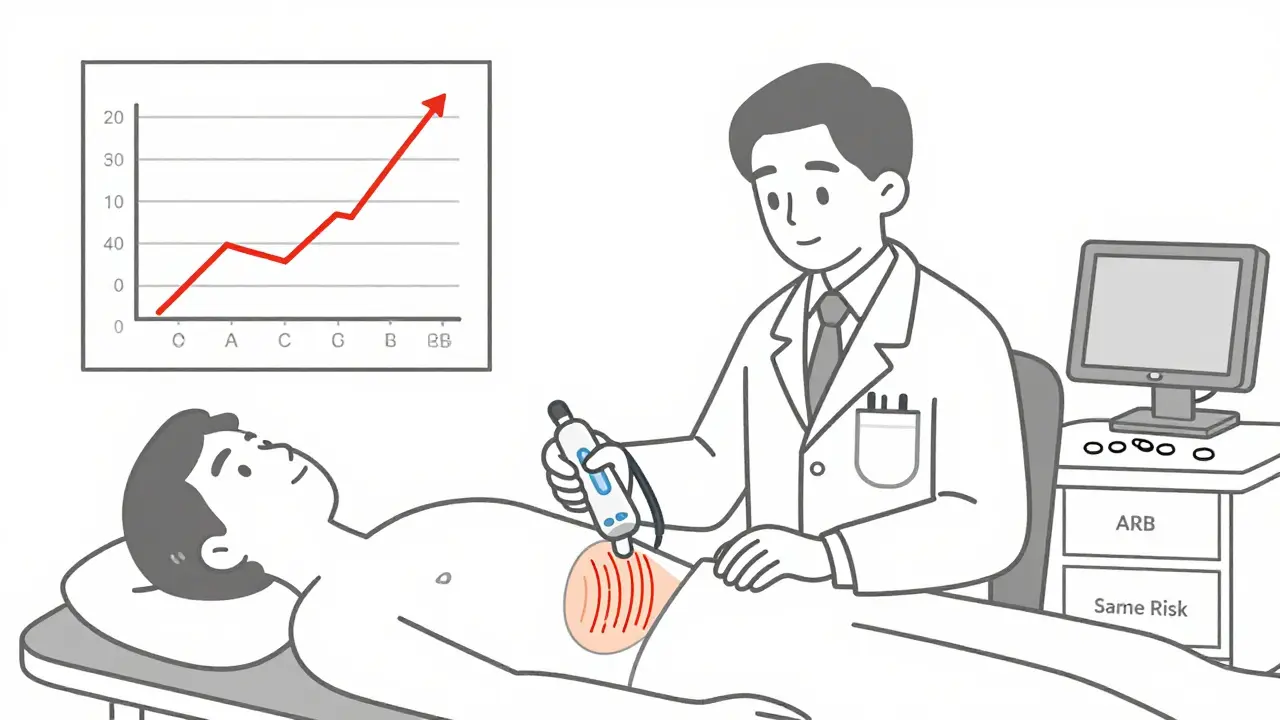
But here’s the problem - it’s still happening. A 2020 study found that over 22% of patients with known bilateral renal artery stenosis were still being prescribed ACE inhibitors in primary care. Why? Because the warning isn’t always in the front of the doctor’s mind. Or because the stenosis was never diagnosed.
Who’s at Risk?
You’re at higher risk for renal artery stenosis if you’re over 50, have a history of atherosclerosis, smoke, have high cholesterol, or have unexplained kidney problems. Other red flags:
- Sudden, severe high blood pressure that’s hard to control
- Abdominal bruit - a whooshing sound heard with a stethoscope over the belly
- Unexplained decline in kidney function after starting blood pressure meds
- Flash pulmonary edema with no clear heart cause
If you have any of these, your doctor should check for renal artery stenosis before starting an ACE inhibitor. The go-to test is a renal artery duplex ultrasound. It’s non-invasive, cheap, and accurate - sensitivity of 86%, specificity of 92%.
What About ARBs?
Many patients ask: “If I can’t take ACE inhibitors, can I take an ARB like losartan or valsartan?” The answer is no. ARBs block the same final pathway - angiotensin II’s action on its receptor. They don’t fix the problem; they just use a different door to get there. The 2019 KDIGO guidelines and the 2002 AHA statement both say ARBs carry the same risk. If you develop acute kidney injury from an ACE inhibitor due to stenosis, switching to an ARB won’t save you. It might make it worse.
Monitoring Is Non-Negotiable
Even if you don’t have known stenosis, guidelines require monitoring when starting an ACE inhibitor. NICE recommends:
- Check creatinine and potassium before starting
- Repeat blood tests 7 to 10 days after starting
- Repeat after each dose increase
- If creatinine rises over 150 micromol/L, stop and refer to a specialist
Most kidney damage from ACE inhibitors in this setting is reversible - if caught early. A 2023 review in Primary Care Notebook found that stopping the drug usually restores kidney function within days. But if low blood flow lasts more than 72 hours, permanent damage can occur.
What Happens If You Ignore the Warning?
A 2018 study of 1,247 patients starting ACE inhibitors found that 18.7% of those with undiagnosed bilateral renal artery stenosis developed acute kidney injury - defined as a 30% or greater rise in creatinine. That’s nearly 1 in 5. Only 2.3% of patients without stenosis had the same reaction. That’s not a small risk. That’s a red alert.
In one case series from 2019, patients with undiagnosed bilateral stenosis who kept taking ACE inhibitors for over a week developed irreversible scarring in their kidneys. Some needed long-term dialysis. These aren’t rare outliers. They’re predictable outcomes of ignoring a well-documented mechanism.
What Should You Do?
If you’re on an ACE inhibitor and have high blood pressure, especially if you’re over 50 or have other vascular disease:
- Ask your doctor if you’ve ever been screened for renal artery stenosis
- Know your baseline creatinine - write it down
- Don’t skip the follow-up blood test after starting the medication
- If your creatinine jumps, don’t wait. Call your doctor immediately
- If you have a history of kidney problems or sudden hypertension, insist on an ultrasound before starting any RAAS-blocking drug
This isn’t about avoiding medication. It’s about using it safely. ACE inhibitors save lives - when used in the right people. In the wrong ones, they can trigger a silent, reversible, but dangerous collapse of kidney function.
The science behind this contraindication has been solid since the 1980s. We’ve seen it in dogs, in humans, in micropuncture studies, and in real-world clinics. The warning hasn’t changed because the physiology hasn’t changed. Your kidneys need that angiotensin II squeeze. If you’re missing one kidney, or both arteries are narrowed - you can’t afford to lose it.
Can ACE inhibitors cause kidney failure in people with renal artery stenosis?
Yes, especially in bilateral renal artery stenosis or in people with only one functioning kidney. ACE inhibitors block angiotensin II, which is critical for maintaining kidney filtration pressure in narrowed arteries. This can cause a rapid drop in kidney function, sometimes leading to acute kidney injury. Studies show up to 18-20% of patients with undiagnosed bilateral stenosis develop significant kidney damage within days of starting the drug.
Is it safe to take ACE inhibitors if I have stenosis in only one kidney?
It may be safe, but only if your other kidney is healthy and functioning normally. In this case, the good kidney can compensate for the reduced function in the affected one. Studies like the ASTRAL trial show minimal kidney function decline in these patients. However, close monitoring of creatinine levels is still required. Never start or continue ACE inhibitors without checking kidney function before and after starting.
Can I switch to an ARB if I can’t take ACE inhibitors due to renal artery stenosis?
No. ARBs (like losartan or valsartan) work on the same pathway - they block angiotensin II from acting on its receptor. Even though they’re a different class of drug, they carry the same risk of causing acute kidney injury in renal artery stenosis. Guidelines from KDIGO and the American Heart Association explicitly state ARBs are not a safe alternative in this situation.
How soon after starting an ACE inhibitor should I get my kidney function checked?
According to NICE and other major guidelines, you should have a blood test for creatinine and potassium 7 to 10 days after starting an ACE inhibitor. This is the window when kidney function changes become detectable. If your creatinine rises more than 30% from baseline, the drug should be stopped and your doctor should evaluate for renal artery stenosis.
Is renal artery stenosis common in people with high blood pressure?
It’s not common overall, but it’s more frequent in certain groups. About 6.8% of people with high blood pressure and unexplained kidney impairment have significant renal artery stenosis. The risk goes up with age, smoking, diabetes, and a history of heart disease. If you’re over 50 and your blood pressure suddenly got worse or is hard to control, screening with a renal ultrasound is recommended.


Comments
Jacob Milano
Man, I never realized how delicate that efferent arteriole squeeze really is. It’s like your kidneys are running on a tiny, high-pressure garden hose and ACE inhibitors just yank the nozzle off. Scary stuff. I’ve got a grandpa on lisinopril - gonna send him this article ASAP.
January 6, 2026 AT 03:57
saurabh singh
Bro, this is gold. In India, we see so many older patients on these drugs without any screening. One uncle ended up on dialysis after his doc just prescribed ramipril for 'high BP'. No ultrasound. No creatinine check. Just 'take this'. We need awareness, not just guidelines.
January 7, 2026 AT 02:12
Dee Humprey
My mom’s creatinine jumped 40% after starting enalapril. They thought it was just aging. Turns out she had unilateral stenosis. They stopped it, she bounced back in 10 days. This post saved her kidneys. Thank you.
January 8, 2026 AT 03:08
Allen Ye
There’s a metaphysical elegance here - the body’s desperate attempt to preserve function through vasoconstriction, and the pharmaceutical intervention that, while benevolent in intent, becomes a violator of homeostasis. We treat hypertension as a villain, yet we ignore that the kidney’s RAAS activation is not pathology - it’s a noble, evolutionary survival mechanism. To suppress it without understanding the context is not medicine - it’s hubris dressed in white coats.
And yet, we are told to 'follow guidelines' as if they were scripture. But guidelines are written by committees who’ve never seen a patient’s creatinine spike in real time, never held the hand of someone who woke up unable to urinate because their kidneys gave up. The science is clear, but the system is blind.
It’s not about whether ACE inhibitors are 'bad'. It’s about whether we’re willing to see the patient before the protocol. The efferent arteriole isn’t a diagram - it’s a lifeline. And when we cut it, we don’t just lower GFR. We lower dignity.
January 8, 2026 AT 10:52
mark etang
It is imperative to underscore that the contraindication of ACE inhibitors in the setting of renal artery stenosis is not merely a clinical suggestion - it is a well-documented, evidence-based, and universally endorsed medical imperative. Deviation from this standard constitutes a breach of the duty of care and may result in irreversible renal damage. All practitioners must adhere to pre-prescription renal function assessment and vigilant post-initiation monitoring.
January 9, 2026 AT 22:55
jigisha Patel
Let’s be honest - 22% of patients with bilateral stenosis are still getting ACE inhibitors? That’s not negligence. That’s malpractice. If your doctor doesn’t check for renal artery stenosis before prescribing an ACE inhibitor, they’re either lazy, untrained, or dangerously complacent. And yes, I’ve seen it. In my hospital. Twice last month.
January 11, 2026 AT 07:47
Jason Stafford
EVERYONE knows Big Pharma pushed these drugs. They knew the risk. They buried the studies. The FDA? Complicit. The guidelines? Written by consultants who own stock in pharma. That 'renal artery duplex ultrasound'? It’s cheap - but it doesn’t make money. The real profit? Lifelong dialysis. They want you dependent. This isn’t medicine - it’s a slow genocide disguised as prevention.
January 11, 2026 AT 18:04
Justin Lowans
Really well-structured breakdown. The garden hose analogy alone should be in every med school lecture. I’ve had patients ask me why they can’t just switch to ARBs - now I’ve got a clear, concise way to explain why that’s like swapping one lock on the same door. Solid work.
January 12, 2026 AT 21:56
Michael Rudge
Oh wow, so you’re telling me that doctors who don’t screen for renal artery stenosis are basically playing Russian roulette with people’s kidneys? And we call this 'standard of care'? I’m starting to think my nephrologist is just a pharmacy sales rep with a stethoscope.
January 13, 2026 AT 05:41
Rory Corrigan
Life is just a series of delicate balances… and we’re the ones holding the scalpel. ACE inhibitors? They’re like cutting the last thread of a hammock - you think you’re relaxing, but you’re just falling. The kidney doesn’t scream. It just… stops. Quietly. Like a candle in a hurricane.
January 14, 2026 AT 12:05
Stephen Craig
Unilateral stenosis? Fine with monitoring. Bilateral? Absolute no. ARBs? Same risk. Check creatinine at 7-10 days. That’s it.
January 14, 2026 AT 17:25
Connor Hale
It’s wild how one tiny blood vessel can hold up an entire system. The body’s so smart - and we’re so clumsy with our drugs. Glad this got laid out plainly. I’ll be sharing this with my dad’s cardiologist.
January 16, 2026 AT 03:31
Jack Wernet
Thank you for this comprehensive and clinically accurate summary. The emphasis on pre- and post-initiation monitoring is critical. As a practitioner, I can attest that adherence to NICE guidelines has significantly reduced iatrogenic renal injury in our population. This is precisely the kind of education that saves lives.
January 16, 2026 AT 06:02
Charlotte N
I just started lisinopril last week… my creatinine was 1.1… should I be worried? I didn’t know I needed a follow-up… I thought it was just a 'take daily' thing… oh god…
January 17, 2026 AT 13:05
Dee Humprey
Charlotte - if you’re reading this: call your doctor today. Don’t wait. Tell them you just read this and you’re scared. Ask for a creatinine test. Do it now. You’re not overreacting. You’re being smart.
January 18, 2026 AT 02:57