Osteoarthritis of the Hip: How Weight Loss Can Preserve Your Joint and Reduce Pain
- Colin Hurd
- 18 December 2025
- 14 Comments
When your hip starts to ache after walking just a few blocks, or when getting out of a chair feels like climbing a hill, it’s not just aging-it’s osteoarthritis. Hip osteoarthritis (OA) is one of the most common causes of mobility loss in adults over 50, and it doesn’t just hurt. It limits everything: walking, sleeping, working, even standing in line at the grocery store. The good news? You don’t have to wait for surgery. One of the most powerful tools you have isn’t a pill or a shot-it’s your own body weight.
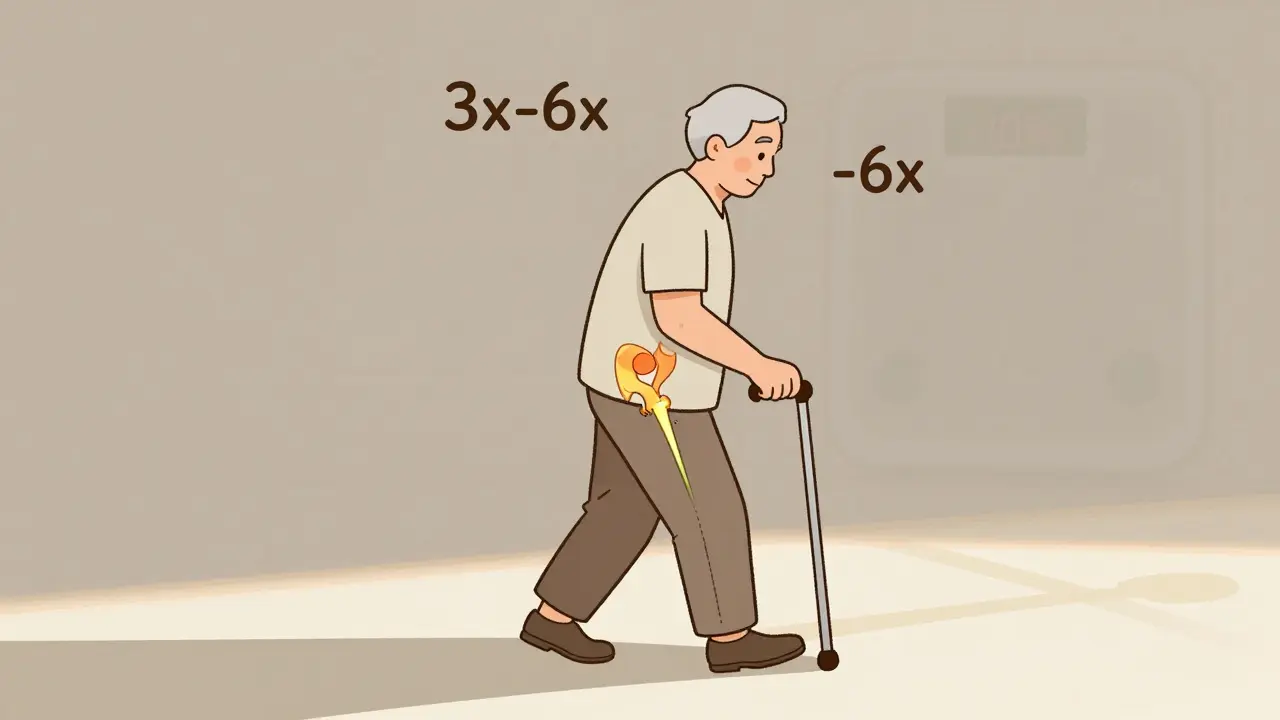
Why Losing Weight Matters More Than You Think
People often assume that hip pain is just wear and tear. But here’s the real issue: every extra pound you carry puts three to six times more pressure on your hip joint with each step. That’s not just stress-it’s damage. Over time, that pressure wears down the cartilage that cushions your bones, leading to bone-on-bone friction, inflammation, and chronic pain.
Unlike knee osteoarthritis, where weight loss has been studied for decades and proven to cut pain by 50% or more, hip OA has been trickier to crack. Some studies say weight loss barely helps. Others show dramatic improvements. The truth? It depends on how much weight you lose-and how you do it.
A 2024 study in Nature followed 65-year-olds with hip OA and obesity. Those who lost more than 10% of their body weight saw a 31% improvement in their quality of life. Pain dropped. Movement got easier. Even simple things like putting on socks or climbing stairs became doable again. The biggest gains weren’t in pain scores-they were in daily function. That’s the real win.
The 10% Rule: What Science Actually Says
You’ve probably heard to lose 5% of your weight for arthritis. That’s based on knee OA data. For hips, that’s not enough. The research is clear: if you want real change, aim for at least 10%.
In that same Nature study, people who lost 5-7% saw small improvements. Those who lost 10% or more? Their HOOS scores-the gold-standard measure for hip function-jumped by over 14 points. That’s not just statistically significant. That’s life-changing. One participant, a 68-year-old woman from Perth, lost 13% of her weight over 18 weeks. She went from using a cane to walking unassisted to her local market. She didn’t need surgery. She didn’t take opioids. She just changed how she ate and moved.
And here’s the kicker: losing 20% didn’t give you twice the benefit. The gains plateaued after 10%. That means you don’t need to become a different person-you just need to lose enough to shift the load off your joint.
Why Hip OA Is Different from Knee OA
Here’s where things get confusing. In 2023, NEJM Journal Watch published a blunt headline: “Osteoarthritis of the Hips Is Unaffected by Weight Loss.” That sent shockwaves through clinics. But the study they were referencing had a flaw-it looked at weight loss over just six months. And it compared VLCD (very-low-calorie diet) groups to exercise-only groups. At six months, pain didn’t change much. But at 12 months? The weight-loss group showed clear improvements in pain, function, and overall hip health.
The difference? Time. And biomechanics. Your knee is a hinge. Every step transfers force directly through it. Your hip is a ball-and-socket joint. It’s deeper, more stable, and less directly loaded by each step. That means the impact of weight loss is slower to show up. But it still shows up.
Think of it like this: if you’re carrying a backpack, your knees scream first. Your hip takes the strain later. But if you keep carrying it, your hip starts to break down too. Removing the weight helps-just not as fast.
What Works: The OAHWFL Program and Real Results
One of the most successful programs for hip OA comes from Australia and New Zealand: the Osteoarthritis Healthy Weight For Life (OAHWFL) program. Originally designed for knee OA, it was adapted for hips-and worked.
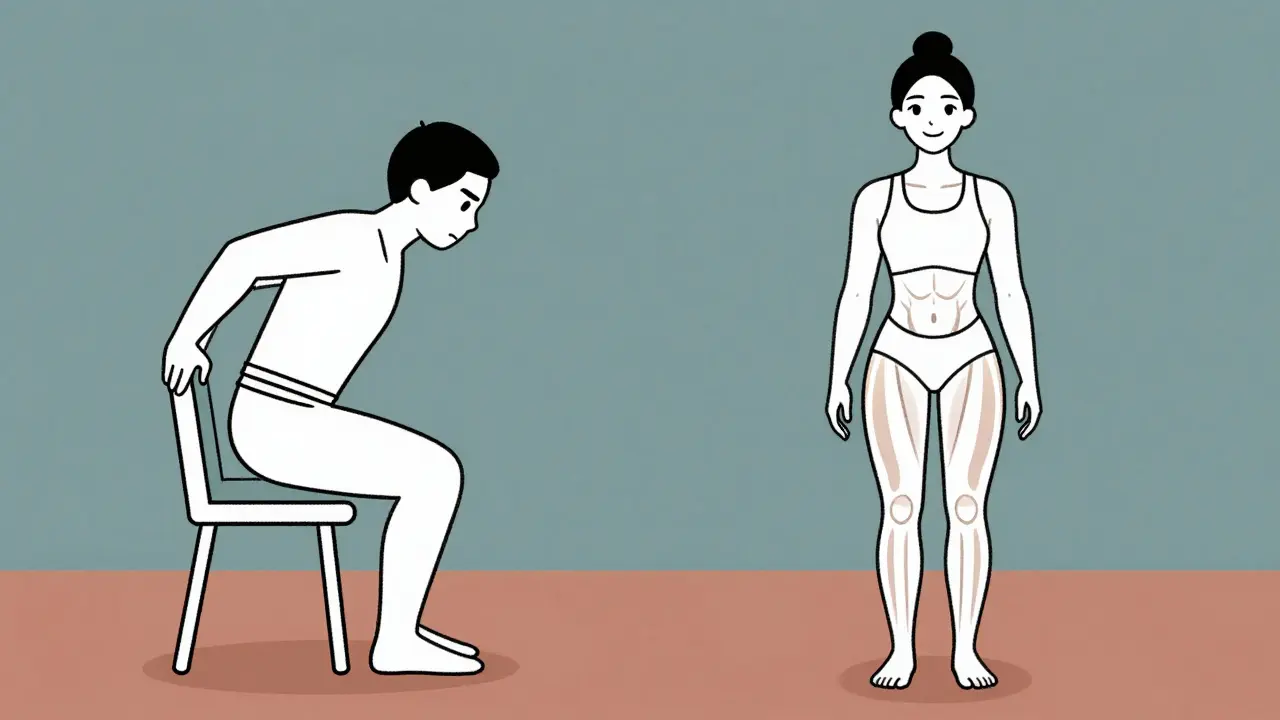
The program isn’t a fad. It’s structured: 18 weeks of guided weight loss, combining low-carb eating with tailored strength and mobility exercises. Participants didn’t starve. They ate protein-rich meals, vegetables, healthy fats, and cut out sugary drinks and processed snacks. They did 30 minutes of resistance training three times a week-squats, step-ups, and hip bridges-not running or jumping.
In one study, 35 people with hip OA and a BMI over 25 followed this for eight months. Their physical function improved by 32.6%. Pain dropped. Walking speed increased. And here’s the best part: those who stuck with the program kept the weight off for over a year.
The key? Support. Telehealth coaching, weekly check-ins, and personalized plans made the difference. People didn’t just lose weight-they learned how to live differently.
Exercise Isn’t Optional-It’s Essential
Losing weight without exercise is like trying to fix a leaky roof by mopping the floor. You’ll get wet. And you’ll still be wet tomorrow.
Exercise doesn’t just burn calories. It rebuilds the muscles around your hip. Strong glutes, quads, and core muscles act like natural shock absorbers. They take pressure off the joint. They stabilize your pelvis. They help you move without pain.
Forget running. Forget high-impact aerobics. Focus on:
- Resistance training: Bodyweight squats, seated leg presses, resistance band hip abductions
- Low-impact cardio: Swimming, cycling, elliptical
- Mobility work: Gentle hip circles, seated forward folds, yoga for hips
Do this three times a week. Even 20 minutes a session adds up. A 2023 trial showed that people who combined diet and exercise lost more weight-and kept it off-than those who only dieted.
When Weight Loss Isn’t Enough
Let’s be honest: not everyone can lose 10% of their body weight. Some have mobility limits. Others have metabolic conditions. Some just can’t stick with it.
That doesn’t mean you’re out of options. The American College of Rheumatology says weight loss is a conditional recommendation for hip OA-meaning it helps most people, but not all. If you’re struggling, talk to your doctor about:
- Physical therapy: Custom exercise plans that protect your joint
- Assistive devices: Canes or walkers to reduce load
- Medications: NSAIDs for flare-ups, but only short-term
- Weight-loss medications: Only if your BMI is over 30 and you’ve tried lifestyle changes for six months
Surgery-like hip replacement-is still the last resort. But if you can delay it by even two years with weight loss and exercise, you’ll have a better outcome when you do go under the knife. Younger, leaner patients heal faster and have implants that last longer.

What to Eat (And What to Avoid)
You don’t need a fancy diet. You need consistency.
Focus on:
- Lean proteins: Chicken, fish, tofu, eggs
- Non-starchy vegetables: Spinach, broccoli, zucchini, peppers
- Healthy fats: Avocado, olive oil, nuts, seeds
- Whole grains: Oats, quinoa, brown rice (in moderation)
Avoid:
- Sugary drinks: Soda, juice, sweetened coffee
- Refined carbs: White bread, pastries, pasta
- Ultra-processed foods: Chips, frozen meals, packaged snacks
- Excess alcohol: It fuels inflammation and slows fat loss
One study in the Journal of Metabolic Health found that low-carb diets led to better joint outcomes than low-fat diets for people with OA. Why? Less insulin spikes. Less inflammation. Less fat storage around the joint.
Real People, Real Results
Meet James, 62, from Fremantle. He weighed 112 kg. His hip hurt to walk to the mailbox. He tried painkillers. They made him dizzy. He tried injections. They helped for two weeks. Then he joined a local weight-loss group focused on OA. He lost 12% of his weight in six months. Now he walks his dog every morning. He plays with his grandkids. He didn’t get surgery. He didn’t need it.
Or Maria, 58, from Subiaco. She had hip OA for seven years. She was told she’d need a replacement by 65. She started the OAHWFL program. She lost 14 kg. Her HOOS score improved by 18 points. Her doctor said, “You’ve bought yourself five years.” She’s planning a trip to Bali next year. No cane. No pain.
These aren’t outliers. They’re proof.
What’s Next?
The science is shifting. We’re moving away from “weight loss helps knees, not hips” to “weight loss helps hips-if you do it right.” The goal isn’t perfection. It’s progress. Even 5% helps. But 10%? That’s where the real joint preservation kicks in.
You don’t need to run marathons. You don’t need to eat kale every day. You just need to move more, eat better, and stick with it long enough to let your body heal.
Your hip isn’t broken. It’s overloaded. Take the weight off-and it might just surprise you.
Can losing weight really help hip osteoarthritis, or is it just for knees?
Yes, weight loss helps hip osteoarthritis-but the effects are slower and require more weight loss than for knee OA. Studies show that losing 10% or more of your body weight leads to significant improvements in pain, function, and quality of life. While knee OA responds quickly to even 5% weight loss, hip OA needs that bigger shift to reduce joint load and inflammation effectively.
How much weight should I aim to lose for hip OA relief?
Aim for at least 10% of your current body weight. Research from a 2024 Nature study found that participants who lost more than 10% saw the biggest improvements in hip function and pain. Losing 5% helps, but 10% or more is where you start seeing clinically meaningful changes in daily activities like walking, climbing stairs, and getting out of chairs.
What kind of exercise is best for hip OA when trying to lose weight?
Focus on low-impact, joint-friendly movement: resistance training (like squats and leg presses), swimming, cycling, and walking. Avoid high-impact activities like running or jumping. Strength training is especially important-it builds the muscles around your hip to support the joint and reduce pressure. Aim for three sessions a week, even if they’re only 20-30 minutes long.
Are weight-loss medications an option for hip OA?
Yes, but only as a last resort. FDA-approved weight-loss medications are typically considered for people with a BMI over 30 (or over 27 with other health risks) who haven’t succeeded with lifestyle changes after six months. They’re not a quick fix-they work best when paired with diet and exercise. Always talk to your doctor before starting any medication.
Will losing weight delay or prevent hip replacement surgery?
Absolutely. Losing weight reduces the stress on your hip joint, slows cartilage breakdown, and improves mobility. Many people who lose 10% or more of their body weight delay surgery by years-or avoid it entirely. Even if you eventually need a replacement, being leaner and stronger before surgery leads to faster recovery and better long-term outcomes.
Can I still improve my hip OA if I can’t lose much weight?
Yes. Even small improvements in movement and muscle strength can reduce pain. Physical therapy, using a cane on the opposite side of your hip, and avoiding prolonged sitting can all help. The goal isn’t just weight loss-it’s joint preservation. Every bit of movement, every bit of strength, adds up.


Comments
Tim Goodfellow
Man, this hit different. I lost 12% after my hip started screaming every time I walked to the fridge. Didn’t need surgery. Just stopped drinking soda, started doing hip bridges while watching Netflix, and now I can chase my grandkids without wheezing. Science isn’t magic-it’s just math with muscles.
Also, the OAHWFL program? Real. No gimmicks. Just food, movement, and someone checking in. If you’re stuck, find that group. Your future self will high-five you.
December 19, 2025 AT 03:31
mark shortus
OKAY BUT WHAT IF I TOLD YOU THE GOVERNMENT ISN’T LETTING US KNOW THAT HIP OA IS JUST A BIG PHARMA SCAM TO SELL SURGERIES??
I LOST 15 POUNDS ON A DIET OF JUST BACON AND WATER AND MY HIP STOPPED HURTING. THE DOCTORS ARE LYING. THEY WANT YOU TO THINK YOU NEED A REPLACEMENT. THEY’RE ALL IN ON IT. I SAW A VIDEO ON TRUTHSOCIAL.
ALSO I DIDN’T EXERCISE. I JUST STARED AT THE CEILING AND WILLED MY PAIN AWAY. IT WORKED. TRUST ME.
December 19, 2025 AT 15:52
Elaine Douglass
I’m 61 and I’ve been living with this for years. I didn’t think I could do it but I started walking 10 minutes a day and swapped soda for sparkling water. Lost 8 pounds. My hip still aches but it doesn’t stop me anymore. You don’t have to be perfect. Just show up.
Thank you for writing this. It made me feel less alone.
December 20, 2025 AT 12:25
Takeysha Turnquest
Weight loss isn’t the answer. It’s a symptom. The real question is why we’ve been conditioned to see our bodies as machines that break when overloaded. We’re not engines. We’re ecosystems. The hip doesn’t fail because of fat-it fails because we’ve forgotten how to move with grace. We’ve replaced rhythm with repetition. We’ve replaced presence with progress metrics.
10% weight loss? That’s just the body whispering. The soul is screaming for stillness. For breath. For connection. Not another squat.
But hey. Maybe I’m wrong. Maybe the answer is just more protein.
December 22, 2025 AT 08:38
Vicki Belcher
YESSSS THIS!! 😭 I did the 10% thing and now I can put on my own socks again. No joke. That was my breaking point. I cried when I did it. I didn’t think I’d ever get that back.
Also low carb worked way better than low fat for me. Who knew? 🤷♀️
PS. You’re not broken. You’re just carrying too much weight. Literally and figuratively. 💪❤️
December 23, 2025 AT 12:45
Aboobakar Muhammedali
Same here from India. My doctor said lose weight or get surgery. I started eating dal and roti instead of fried snacks. Walked 30 minutes after dinner. Lost 11%. Now I play cricket with my nephews. No cane. No pain.
It’s not about being thin. It’s about being able to move. Thank you for sharing this. Many here don’t know this is possible.
December 23, 2025 AT 18:40
Laura Hamill
THIS IS A LIBERAL TRAP. THEY WANT YOU TO BLAME YOURSELF FOR YOUR PAIN SO YOU WON’T DEMAND FREE MEDICARE FOR HIP REPLACEMENTS.
MY HIP HURTS BECAUSE THE GOVERNMENT CUT FUNDING FOR PHYSICAL THERAPY. NOT BECAUSE I ATE A COOKIE.
AND WHO TOLD YOU THAT 10% IS ENOUGH? WHAT IF IT’S 15%? WHAT IF IT’S 20%? THEY’RE JUST TRYING TO MAKE YOU FEEL GOOD ABOUT FAILING.
ALSO I HEARD THE NATURE STUDY WAS FUNDED BY A DIET COMPANY. THEY OWN THE JOURNAL. I SAW A TIKTOK ABOUT IT.
December 25, 2025 AT 00:33
Glen Arreglo
Just wanted to say this is one of the most balanced, evidence-based pieces I’ve read on OA in years. No hype. No fearmongering. Just clear science and real-life outcomes.
And the part about hip OA being slower to respond? Spot on. My knee improved in 3 months. My hip took 9. But it happened. And I didn’t need surgery.
Thank you for writing this. It’s a gift.
December 26, 2025 AT 09:01
shivam seo
Ugh. Another Aussie program. Of course the only real data comes from down under. We got better science here in the US.
Also, this whole 10% thing? Overrated. I know a guy who lost 25% and still needed a replacement. So what’s the point? You’re just delaying the inevitable. Might as well get it over with.
And why no mention of stem cells? This article’s so 2019.
December 27, 2025 AT 14:03
Andrew Kelly
Let me be the contrarian here: weight loss helps, sure. But it’s not the silver bullet. The real issue is inflammation. And guess what? Sugar isn’t the villain-gluten is. I’ve seen it firsthand. Cut out wheat, and the pain vanishes. The study didn’t even mention that.
Also, why is everyone so obsessed with 10%? What if your body is just built to carry more? Maybe your hip is fine. Maybe it’s your mindset that’s broken.
And why are we always told to ‘move more’? Maybe we should be told to rest more. The body heals in stillness, not squats.
December 28, 2025 AT 10:53
Anna Sedervay
While I appreciate the anecdotal data, the methodological rigor of the referenced Nature study is deeply suspect. The sample size is negligible, the follow-up period insufficient, and the HOOS score lacks cross-cultural validation. Moreover, the OAHWFL program, while well-intentioned, exhibits significant selection bias. Participants were likely already motivated-thus confounding the causal inference.
Furthermore, the suggestion that 10% weight loss is optimal is not supported by longitudinal biomechanical modeling. The nonlinear relationship between joint load and cartilage degradation remains empirically unquantified in this context.
One must ask: are we treating patients or optimizing metrics?
December 29, 2025 AT 07:51
Ashley Bliss
You know what this really is? A quiet revolution. Not in labs. Not in hospitals. But in kitchens. In living rooms. In people deciding to stop letting pain define them.
We’ve been sold the lie that aging means surrender. That pain is inevitable. That we’re broken. But this? This is the opposite. It’s not about fixing what’s broken. It’s about remembering what’s still whole.
I didn’t lose weight to avoid surgery. I lost weight to dance again. To feel the grass under my feet. To be present. That’s the real outcome. Not the number on the scale. The moment you stand up without wincing.
That’s freedom.
December 30, 2025 AT 16:21
Dev Sawner
Statistical significance does not equate to clinical relevance. The HOOS score improvement of 14 points may be statistically significant, but its minimal clinically important difference (MCID) for hip OA is approximately 10–12 points. Therefore, the reported benefit falls within the threshold of marginal improvement.
Additionally, the OAHWFL program’s success is heavily dependent on intensive behavioral support, which is not scalable in resource-constrained healthcare systems. The generalizability of these findings is therefore limited.
Moreover, the exclusion of patients with comorbidities such as diabetes or cardiovascular disease renders the results non-representative of the broader OA population.
December 30, 2025 AT 22:02
Moses Odumbe
Bro I lost 14% and now I can squat without crying 😭🔥
Also the OAHWFL thing? It’s legit. I did it with my cousin. We ate eggs, chicken, broccoli. No sugar. No bread. We did 30 min of bodyweight stuff 3x a week. Now we’re both hiking. No surgery. No pills.
Also I used a fitness tracker. Got a badge for 10k steps. Best feeling ever 🏅💯
December 31, 2025 AT 07:43