Why Generic Drugs Cost 80-85% Less Than Brand-Name Drugs

- Colin Hurd
- 14 November 2025
- 15 Comments
Ever looked at your prescription receipt and wondered why your generic pill costs $4 while the brand-name version is $500? It’s not a trick. It’s not a scam. It’s the system working exactly as designed. Generic drugs aren’t cheaper because they’re weaker, older, or lower quality. They’re cheaper because they don’t carry the massive debt of invention.
Same Medicine, Different Price Tag
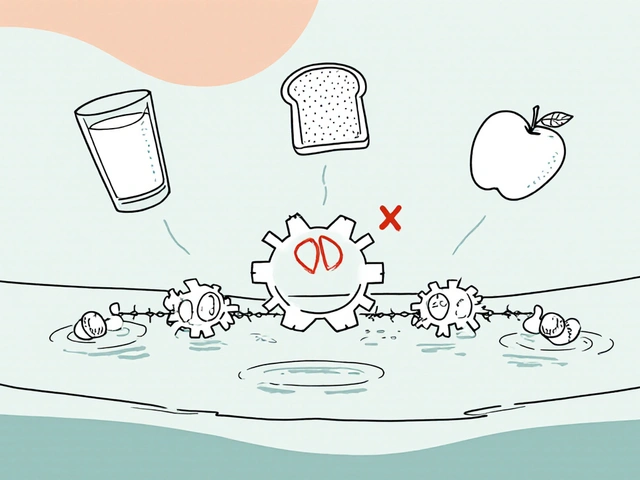
A generic drug isn’t a copycat. It’s a chemical twin. The FDA requires that every generic drug contain the exact same active ingredient, in the same strength, same dosage form, and same route of delivery as the brand-name version. That means if you take generic atorvastatin, you’re getting the same molecule that’s in Lipitor. Same for omeprazole and Prilosec, metformin and Glucophage, sertraline and Zoloft. The FDA calls this bioequivalence-meaning the drug enters your bloodstream at the same rate and to the same extent as the brand. No guesswork. No compromise.Why Brand-Name Drugs Cost So Much
Brand-name drugs aren’t expensive because they’re better. They’re expensive because they had to be invented from scratch. Developing a new drug takes 8 to 12 years. It costs about $2.6 billion on average, according to the Tufts Center for the Study of Drug Development. That money pays for thousands of lab experiments, animal tests, and clinical trials involving tens of thousands of people. Most drugs fail along the way. Only one in ten that enter testing ever gets approved. The company has to recoup all that loss-and make a profit-during the 20-year patent window they get from the moment they file. That’s why, for those first 10 to 15 years, you’re paying for the dream of a cure, not just the pill.How Generics Skip the Billions
Once the patent expires, any company can make the same drug. But they don’t start from zero. They don’t need to repeat the animal studies or the massive human trials. Instead, they file an Abbreviated New Drug Application (ANDA). The FDA only asks them to prove one thing: that their version behaves the same in your body as the original. That’s it. No need to prove safety again. No need to prove effectiveness again. Just prove bioequivalence. That cuts development time from a decade to about 1 to 3 years-and slashes costs from billions to just $1 million to $5 million per drug.The Hatch-Waxman Act: The Rule That Changed Everything
Before 1984, generic drugs faced a legal gray zone. The Hatch-Waxman Act fixed that. It created a clear path for generics to enter the market without re-doing every test. In exchange, it gave brand-name companies extra time to recover costs if a generic challenge delayed their patent expiration. But the real win was for patients. The law made it possible for multiple companies to compete on the same drug. And competition? That’s where the real price drop happens.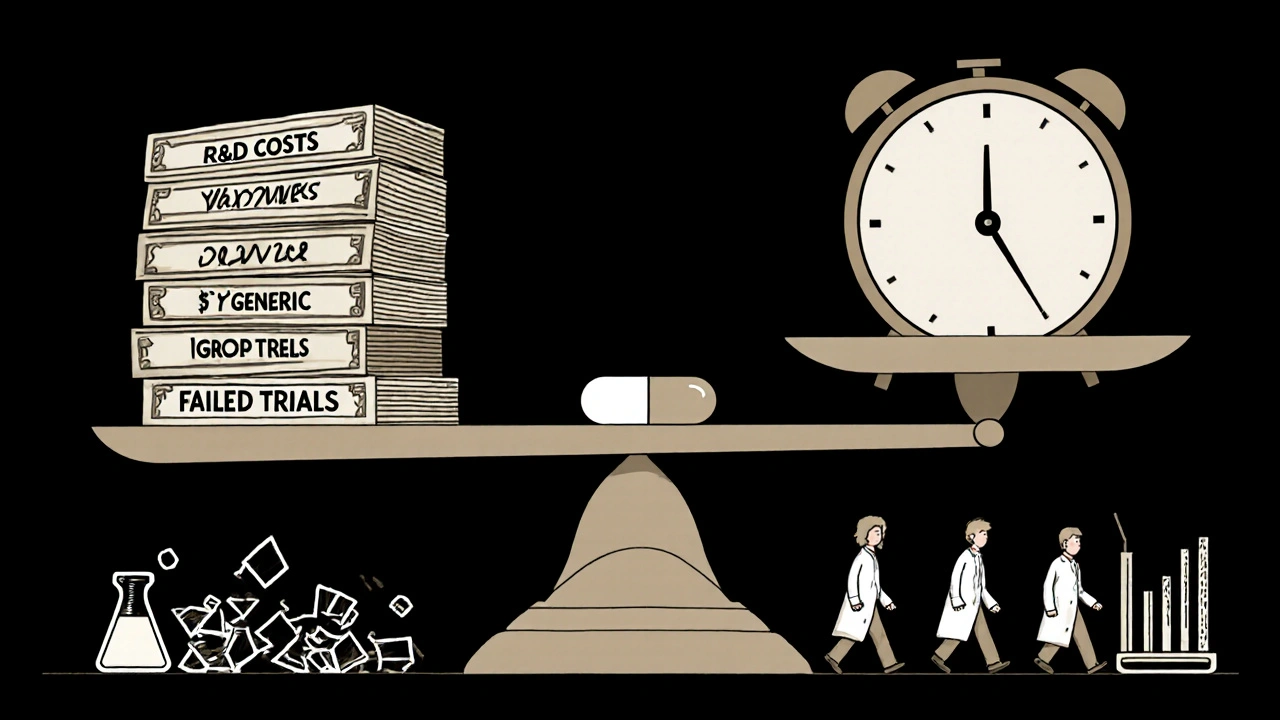
Competition Drives Prices Down-Fast
The moment the first generic hits the market, prices start falling. By the time five or six companies are selling the same generic, prices drop by 80% to 90%. The Congressional Budget Office found that within a year of generic entry, the average price of a drug falls by 80%. By the time 10 manufacturers are involved-common for popular drugs like metformin or lisinopril-the price can be less than 5% of the brand’s original cost. Tebra’s 2023 survey found that generics cost 79% less on average. That’s not a rounding error. That’s $400 a month saved on cholesterol meds. $300 saved on heartburn pills. That’s not a luxury. For many, it’s the difference between taking the medicine and skipping doses.Same Rules, Same Factory Standards
Some people worry that generics are made in sketchy factories. They’re not. The FDA inspects every manufacturing site-brand and generic alike-about 12,000 times a year worldwide. Both must follow the same Current Good Manufacturing Practices (CGMP). The pills must stay potent within 90% to 110% of the labeled amount for their entire shelf life. The same quality controls apply. The only differences you might notice? Color, shape, or flavor. Those are just trademarks. The FDA doesn’t allow generics to look identical to the brand, so you can’t confuse them on the shelf. But the active ingredient? Identical.Who Uses Generics? Almost Everyone
You might think generics are for people on Medicaid or without insurance. But that’s not true. Ninety percent of all prescriptions filled in the U.S. are for generics. Yet they make up only 18% of total drug spending. That’s because brand-name drugs, though only 10% of prescriptions, cost 82% of the money. Generic drugs saved the U.S. healthcare system $293 billion in 2022 alone. That’s more than the entire budget of the Department of Education. And it’s not just saving money-it’s keeping people healthy. A 2023 study by RxOutreach found patients who switched to generics had 28% higher adherence rates because they could actually afford to take them.
Why Some People Still Don’t Trust Them
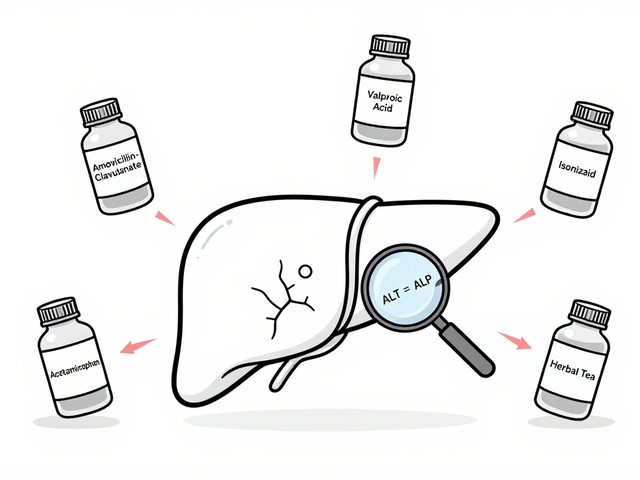
Despite the science, skepticism lingers. Tebra’s survey found 62% of Americans trust brand-name drugs more-even though 84% admit generics are just as effective. Why? Because of appearances. A pill that looks different feels different. Some patients report side effects after switching, but studies show it’s often the placebo effect-or a change in inactive ingredients like dyes or fillers, not the active drug. For most drugs, it doesn’t matter. But for narrow therapeutic index drugs like warfarin, levothyroxine, or phenytoin, even tiny variations in absorption can matter. That’s why some doctors prefer to stick with one brand or generic manufacturer for these. But even then, the FDA says all approved generics meet the same standard. If you notice a change after switching, talk to your pharmacist. Don’t assume it’s the drug.What You Can Do
Ask your doctor if a generic is available. Ask your pharmacist if they can substitute. Most states allow automatic substitution unless the doctor writes “dispense as written.” Check your insurance formulary-generics are almost always Tier 1, meaning $0 to $15 copay. Brand-name drugs? Often $50 or more. If your insurance won’t cover a generic, ask for a prior authorization exception. If you’re paying out of pocket, use GoodRx or SingleCare. You can often find generics for under $5 at Walmart, Costco, or CVS. And if you’re struggling to afford your meds, programs like RxOutreach offer discounts of up to 80% on both brand and generic drugs.The Bigger Picture
The generic drug industry isn’t perfect. Supply chains are fragile-70% of active ingredients come from China and India. Pandemics and political tensions can cause shortages. And some brand-name companies pay generics to delay entry-so-called “pay-for-delay” deals-which cost consumers $3.5 billion a year. But the system still works. It’s designed to reward innovation, then let the market drive prices down. And for the 90% of prescriptions filled with generics? It’s working brilliantly.Generic drugs aren’t a compromise. They’re the smartest part of modern medicine. You get the same result, the same safety, the same science-for a fraction of the cost. And that’s not just good for your wallet. It’s good for your health.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict safety, strength, quality, and purity standards as brand-name drugs. Every generic must prove bioequivalence-meaning it delivers the same amount of active ingredient into your bloodstream at the same rate as the brand. The FDA inspects manufacturing facilities for both brand and generic drugs equally, conducting around 12,000 inspections worldwide each year.
Why do generic pills look different from brand-name pills?
By law, generic drugs can’t look exactly like the brand-name version because of trademark rules. So manufacturers change the color, shape, size, or flavor. These differences are only in inactive ingredients like dyes or fillers. The active ingredient-the part that works-is identical. If you’re concerned about a change in appearance, talk to your pharmacist. It doesn’t mean the drug is less effective.
Can I trust generics for chronic conditions like high blood pressure or thyroid disease?
For most people, yes. Generics are used safely every day for conditions like hypertension, diabetes, and hypothyroidism. For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-small changes in absorption can matter. Some doctors prefer to keep patients on one brand or generic manufacturer to avoid any variability. But the FDA confirms all approved generics meet the same standard. If you notice a change in how you feel after switching, tell your doctor. It’s not common, but it’s worth checking.
Do insurance plans cover generics better than brand-name drugs?
Yes. Most insurance plans have three tiers: Tier 1 is generics, Tier 2 is brand-name drugs, and Tier 3 is specialty medications. Generics usually have the lowest copay-often $0 to $15. Brand-name drugs can cost $25 to $50 or more. Some plans won’t cover a brand-name drug at all if a generic is available, unless your doctor requests an exception. Always check your formulary before filling a prescription.
How long does it take for a generic to become available after a brand-name drug’s patent expires?
It typically takes 3 to 4 years from patent expiration for the first generic to hit the market. That’s because companies need time to file their application, go through FDA review (which averages 10 months), and set up manufacturing. But once the first generic arrives, others follow quickly. The average generic drug has 14 manufacturers competing by the time it’s been on the market for a year, driving prices down even further.
Are there any risks in switching from a brand-name drug to a generic?
For the vast majority of medications, no. The FDA and the American Medical Association both confirm that generic substitution is safe and appropriate for 95% of drugs. Rarely, patients report side effects after switching-often due to changes in inactive ingredients or psychological factors. If you feel different after switching, don’t assume the generic is ineffective. Talk to your pharmacist or doctor. They can help determine if it’s the drug, the filler, or something else.
Why are some generic drugs still expensive?
Some generics stay expensive because there’s little competition. If only one or two companies make a drug, prices don’t drop much. This happens with older drugs, complex formulations like inhalers or injectables, or drugs with low profit margins. The FDA is working to speed up approval for these complex generics. You can also use discount programs like GoodRx or RxOutreach to find lower prices even on these drugs.


Comments
Kihya Beitz
So let me get this straight-we pay $500 for a pill because some pharma bro spent 12 years and $2.6 billion to invent it, but the second it’s off-patent, some factory in India makes the exact same thing for $4 and we’re supposed to be grateful? 🤡
November 15, 2025 AT 04:31
Jennifer Walton
The system rewards invention, then abandons it. That’s capitalism. Not evil. Just inevitable.
November 15, 2025 AT 04:37
John Foster
It’s not just about the cost of development-it’s about the moral weight of innovation. When you take a generic, you’re not just saving money. You’re participating in the erosion of incentive. If no one can profit from discovery, who will risk everything to cure Alzheimer’s? Or a new antibiotic? The system isn’t broken-it’s being starved by short-term thinking. We treat medicine like a commodity, not a covenant.
November 15, 2025 AT 13:18
Edward Ward
I appreciate the breakdown, but I think we’re missing the bigger picture: the FDA’s bioequivalence standard is actually incredibly rigorous, and the fact that 90% of prescriptions are generics speaks volumes about how much trust patients have in them. The real issue isn’t efficacy-it’s perception. People associate the color, shape, and branding with quality, even when it’s irrelevant. That’s psychological, not pharmacological. And the price drop? That’s pure market efficiency. When five companies are fighting to sell the same molecule, the only thing left to compete on is price-and that’s good for everyone except the shareholders.
November 16, 2025 AT 12:11
Andrew Eppich
It's irresponsible to suggest that cost savings should override the integrity of pharmaceutical innovation. Without patent protection, there is no incentive to develop life-saving drugs. The current system, while imperfect, ensures that medical progress continues.
November 17, 2025 AT 07:37
Jessica Chambers
My mom switched from Zoloft to sertraline and swore she ‘felt different.’ Turns out, the generic had a different filler. She got migraines. Now she pays $50 extra. 🤷♀️
November 18, 2025 AT 05:08
Shyamal Spadoni
you think this is about science? nah. the fda is owned by big pharma. they let the generics in but only after the brand made their billions. also 70% of ingredients come from china-do you really think they’re not messing with the dose? they’re controlling the medicine supply. this is how they keep us docile. wake up. the pills are fine. the system is rigged.
November 18, 2025 AT 07:10
Ogonna Igbo
Why do Americans think they own medicine? We make 70% of the world’s generics in India and China. You cry about $500 pills while we take our $3 pills and still live longer. Your system is broken because you pay for marketing, not medicine. Your doctors are salesmen. Your insurance is a pyramid scheme. We don’t need your patents. We need your humility.
November 19, 2025 AT 13:59
BABA SABKA
Let’s be real: the generic industry is a supply chain marvel. You’ve got API synthesis in China, formulation in India, blister packaging in Mexico, and distribution via Amazon logistics. The cost isn’t $1M-it’s $100k if you’re smart. The real bottleneck? Regulatory latency. The FDA takes 10 months to approve a generic because they’re still using fax machines. The real villain isn’t Pfizer-it’s bureaucracy.
November 20, 2025 AT 00:41
Chris Bryan
Generics are fine for the working class. But if you’re serious about your health, you get the brand. You don’t gamble with your liver, your heart, your brain. This isn’t about price. It’s about dignity. I don’t buy store-brand insulin. I don’t buy store-brand heart meds. Why? Because I’m not a statistic.
November 20, 2025 AT 18:28
Jonathan Dobey
They call it bioequivalence, but what they really mean is ‘close enough for government work.’ The FDA doesn’t test for long-term effects, epigenetic drift, or gut microbiome interactions. They test blood levels on 24 healthy college kids. That’s not science-it’s a loophole dressed in a lab coat. Meanwhile, the real drugs-those with real innovation-are being buried under a mountain of generics that look identical but aren’t identical at the quantum level. The system isn’t designed to heal. It’s designed to maximize shareholder value under the guise of public good.
November 21, 2025 AT 10:44
ASHISH TURAN
My dad’s on metformin. Switched from Glucophage to generic. No issues. Cost went from $90 to $4. He’s alive because of it. Don’t overthink it. The science is solid. The system works.
November 22, 2025 AT 23:38
Ryan Airey
Stop romanticizing generics. The price drop isn’t because of competition-it’s because the FDA lets manufacturers cut corners on fillers and stability testing. I’ve seen lab reports. The dissolution profiles vary wildly. The ‘same molecule’ doesn’t mean the same delivery. And when you’re on warfarin? That difference kills people. This isn’t healthcare. It’s risk redistribution.
November 24, 2025 AT 17:42
Hollis Hollywood
I’ve been on levothyroxine for 12 years. I’ve switched generics five times. Sometimes I feel off for a week. Other times, nothing. I’ve learned to stick with the same pharmacy and ask for the same manufacturer. It’s not about the drug-it’s about consistency. The system isn’t perfect, but it’s the best we’ve got. And honestly? I’m just glad it exists at all. I know people who can’t afford either. That’s the real tragedy.
November 26, 2025 AT 07:16
Aidan McCord-Amasis
Generics = 🚀💸
November 27, 2025 AT 06:20