Anxiety Disorders: Types, Symptoms, and Evidence-Based Treatments

- Colin Hurd
- 17 February 2026
- 0 Comments
When your heart races for no reason, or you can't stop worrying about things that most people wouldn't even think twice about, it's not just stress. It might be an anxiety disorder. These aren't just "feeling nervous" moments - they're persistent, overwhelming, and often disabling conditions that affect nearly 1 in 5 adults in the U.S. every year. And while anxiety is a normal part of life, when it becomes constant, intense, and starts controlling your daily routine, it's time to recognize it for what it is: a medical condition with real, proven treatments.
What Are the Main Types of Anxiety Disorders?
Anxiety isn't one thing. It shows up in different forms, each with its own pattern of symptoms and triggers. The DSM-5, the standard guide used by mental health professionals, recognizes seven main types, though some overlap in symptoms.
Generalized Anxiety Disorder (GAD) is the most common. People with GAD don't just worry - they worry constantly about everyday things: work, health, bills, even minor decisions. This isn't occasional stress. It's a background hum of dread that lasts six months or more, often without any clear trigger. About 3.1% of U.S. adults live with GAD, and many don't even realize they have a disorder - they just think they're "always the anxious type."
Panic Disorder hits like a lightning strike. You're sitting at your desk, driving home, or even sleeping, and suddenly - your chest tightens, your heart pounds at 130 beats per minute, your hands shake, and you feel like you're dying. These panic attacks come out of nowhere, and the fear of the next one becomes its own prison. About 2.7% of adults experience this, and many avoid places or situations where they've had an attack before.
Social Anxiety Disorder (also called social phobia) turns everyday interactions into minefields. Talking to a cashier, giving a presentation, or even eating in public can trigger intense fear of being judged, embarrassed, or humiliated. It's not shyness. It's a deep, physical dread of social scrutiny. Around 7.1% of U.S. adults struggle with this, and many turn down jobs, skip events, or isolate themselves to avoid the anxiety.
Specific Phobias are intense, irrational fears of specific things - spiders, heights, flying, needles, even clowns. The fear is so strong it leads to avoidance, even when the object poses no real danger. About 8.7% of adults have at least one specific phobia. What's surprising? Many people with phobias can function normally - except when they're near the trigger.
Obsessive-Compulsive Disorder (OCD) used to be grouped under anxiety disorders, but now it's separate in the DSM-5. Still, the anxiety link is strong. People with OCD get stuck in loops of intrusive thoughts (obsessions) and feel compelled to perform rituals (compulsions) to reduce the distress - washing hands until they bleed, checking locks 20 times, or mentally counting to prevent harm. About 1.2% of adults have OCD.
Separation Anxiety Disorder isn't just for kids anymore. Adults can develop it too, especially after a major loss or life change. The fear isn't just sadness - it's terror that something terrible will happen to a loved one if they're apart. About 4.1% of adults experience this, often after divorce, death, or moving away from family.
Selective Mutism mostly affects children, but it can carry into adulthood. It's not shyness or rebellion. It's a freeze response in social situations where speaking feels physically impossible - even though the person can talk normally at home. Prevalence is low (under 2%), but it's often missed or misdiagnosed as autism or oppositional behavior.
What Do the Symptoms Actually Feel Like?
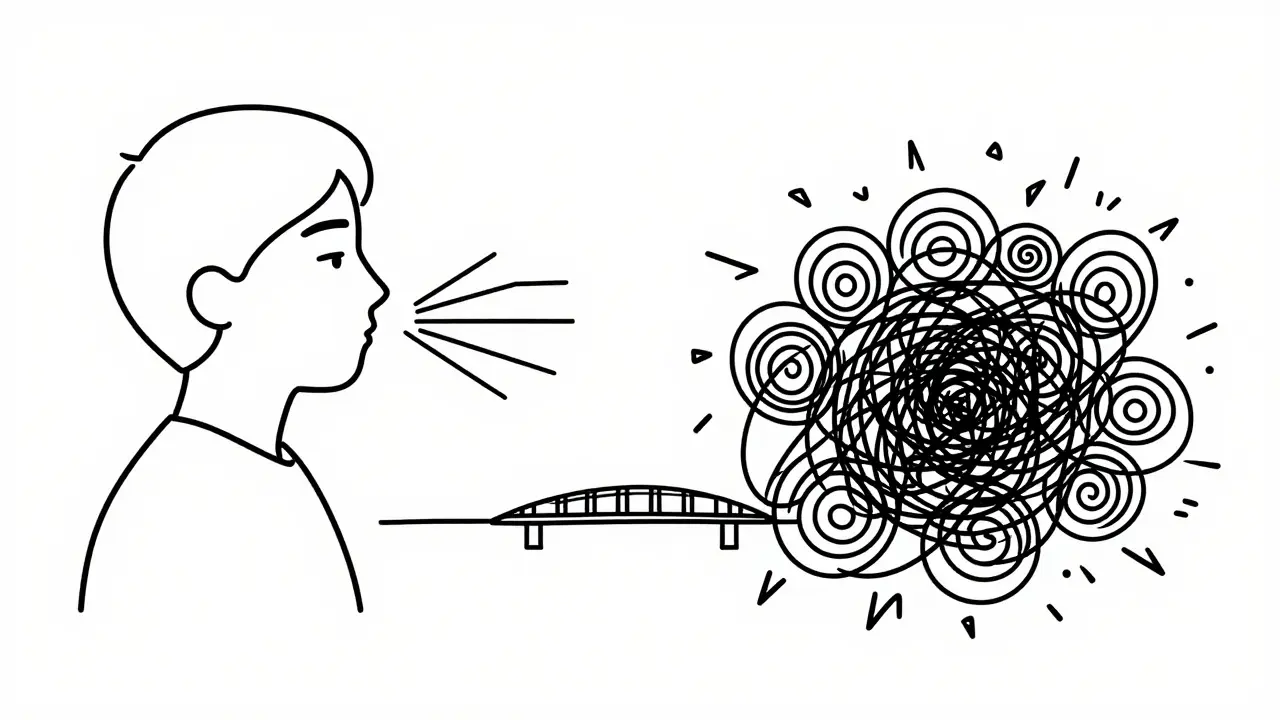
Anxiety doesn't just live in your head. It lives in your body. If you've ever had a panic attack, you know: your chest feels like it's being crushed, your throat tightens, your hands tremble, and your mind races like a runaway train. These aren't "just nerves." They're biological responses gone off track.
Physically, anxiety triggers the fight-or-flight system - even when there's no real danger. Studies show 92% of people with panic disorder report sweating during attacks, 87% experience trembling, 83% feel short of breath, and 76% get dizzy. Your heart rate can spike from 70 to over 130 beats per minute. Nausea, headaches, and muscle tension are common. Many people visit emergency rooms thinking they're having a heart attack.
Cognitively, it's a mental hamster wheel. You can't stop thinking about what might go wrong. Eighty-nine percent of people with GAD say they struggle to concentrate because their mind is flooded with "what ifs." Rumination - replaying the same anxious thought over and over - affects 91% of those with chronic anxiety. Catastrophic thinking is rampant: "If I make a mistake, I'll lose my job, my partner will leave, I'll end up homeless."
Emotionally, it's exhausting. Ninety-five percent of panic attack survivors describe a crushing sense of impending doom. Eighty-eight percent fear they're losing control - either mentally, physically, or both. And for many, there's a deep shame. "Why can't I just snap out of it?" That guilt makes it harder to ask for help.

What Treatments Actually Work?
The good news? Anxiety disorders are among the most treatable mental health conditions. Decades of research have shown that two approaches - cognitive behavioral therapy (CBT) and certain medications - are the most effective. And they work better together.
Cognitive Behavioral Therapy (CBT) is the gold standard. It's not talk therapy where you just vent. It's structured, goal-oriented, and skill-based. You learn to identify distorted thoughts (like "I'll fail and everyone will laugh") and replace them with more realistic ones ("I might feel nervous, but I've handled this before"). You also learn exposure techniques - slowly, safely facing the things you fear. For social anxiety, that might mean ordering coffee in front of someone. For panic disorder, it might mean letting your heart race without fleeing. Studies show 50-60% of people see major symptom reduction after 12-20 sessions. And the effects last. Unlike medication, CBT teaches you lifelong skills.
Exposure therapy, a core part of CBT, is especially powerful. For specific phobias and social anxiety, it works 60-80% of the time when done right. Yes, it's hard. Seventy-five percent of people feel worse before they feel better. But that temporary discomfort is the price of long-term freedom.
Medication helps too - especially for moderate to severe cases. SSRIs (like sertraline and fluoxetine) are first-line choices. They don't work instantly. It takes 4-8 weeks to build up in your system. But once they do, 40-60% of people see significant improvement. They're not "happy pills." They help regulate the brain chemicals that keep anxiety in check. Side effects? Nausea, insomnia, or emotional blunting - but these often fade after a few weeks.
SNRIs like venlafaxine are similar and often used if SSRIs don't help. Benzodiazepines (like Xanax) work fast - within 30 minutes - but they're not recommended for long-term use. They're addictive. Up to 30% of people who use them for more than a few months develop dependence. They're best for crisis situations, not daily management.
A 2023 NAMI survey found that 58% of people who combined CBT and medication reported symptom improvement. Only 42% improved with medication alone. And just 38% improved with therapy alone. The combination isn't just additive - it's synergistic.
What Gets in the Way of Treatment?
Even with proven treatments, many people don't get better. Why? Barriers are real.
First, access. In many places, including rural Australia and parts of the U.S., there's a shortage of therapists trained in CBT. Wait times for specialists can be 6-8 weeks. Some people give up before they even start.
Second, side effects. Some people stop taking SSRIs because they feel "numb" or lose their emotional edge. Others can't tolerate the nausea or sleep issues. Switching medications takes time - and patience.
Third, stigma. Even today, some people believe anxiety is "just in your head" or a sign of weakness. But anxiety disorders are biological. Brain scans show differences in the amygdala and prefrontal cortex - the parts that handle fear and decision-making. This isn't laziness. It's neurology.
Fourth, cost. Therapy isn't always covered well by insurance. A single session can cost $150 or more. Many people can't afford 12-20 sessions.
But alternatives are growing. Digital tools like nOCD and Wysa - FDA-cleared apps that deliver CBT techniques - show 35-45% symptom reduction in just 8 weeks. And Medicare now covers two CBT-based platforms. Online support groups (like r/anxiety on Reddit) offer community, validation, and practical tips from people who've been there.
What’s New in Treatment?
The field is moving fast. In 2023, the FDA approved zuranolone (Zurzuvae), the first oral neuroactive steroid for postpartum anxiety, with a 54% remission rate in trials. It works in days, not weeks.
Research into ketamine-assisted therapy is promising. In 2022, JAMA Psychiatry found it produced rapid relief in treatment-resistant anxiety - sometimes within hours. It's still experimental, but it's a breakthrough for people who haven't responded to anything else.
And then there's precision medicine. A 2023 study in Nature Medicine identified three distinct anxiety "biotypes" using brain scans. Each responds differently to treatment. This means in the future, your doctor might use a brain scan to pick the best therapy for you - no more trial and error.
AI is helping too. Stanford researchers built an algorithm that predicts panic attacks 24 hours in advance with 87% accuracy by analyzing voice patterns, heart rate, and sleep data. Imagine getting a warning on your phone: "You're at high risk for an attack tomorrow. Try this breathing exercise."
What Can You Do Right Now?
If you recognize these symptoms in yourself:
- Don't wait. Anxiety doesn't get better on its own - it usually gets worse.
- Start with your GP. They can rule out physical causes (like thyroid issues) and refer you to a mental health specialist.
- Look for a therapist trained in CBT. Ask: "Do you use exposure therapy?" If they say no, keep looking.
- Try a digital CBT app. They're affordable, private, and evidence-based.
- Practice diaphragmatic breathing: inhale for 5 seconds, hold for 2, exhale for 6. Do this 5 times, 3 times a day. It calms your nervous system fast.
- Join a support group. You're not alone. The Anxiety and Depression Association of America runs over 300 weekly groups.
Anxiety disorders are common. They're treatable. And they don't define you. With the right tools, people recover - not just manage, but truly recover. You don't have to live in fear. There's a path out, and it starts with one step.



