Benzodiazepines: What They Do, Why They're Risky, and How to Use Them Safely
- Colin Hurd
- 2 February 2026
- 8 Comments
What benzodiazepines actually do in your brain
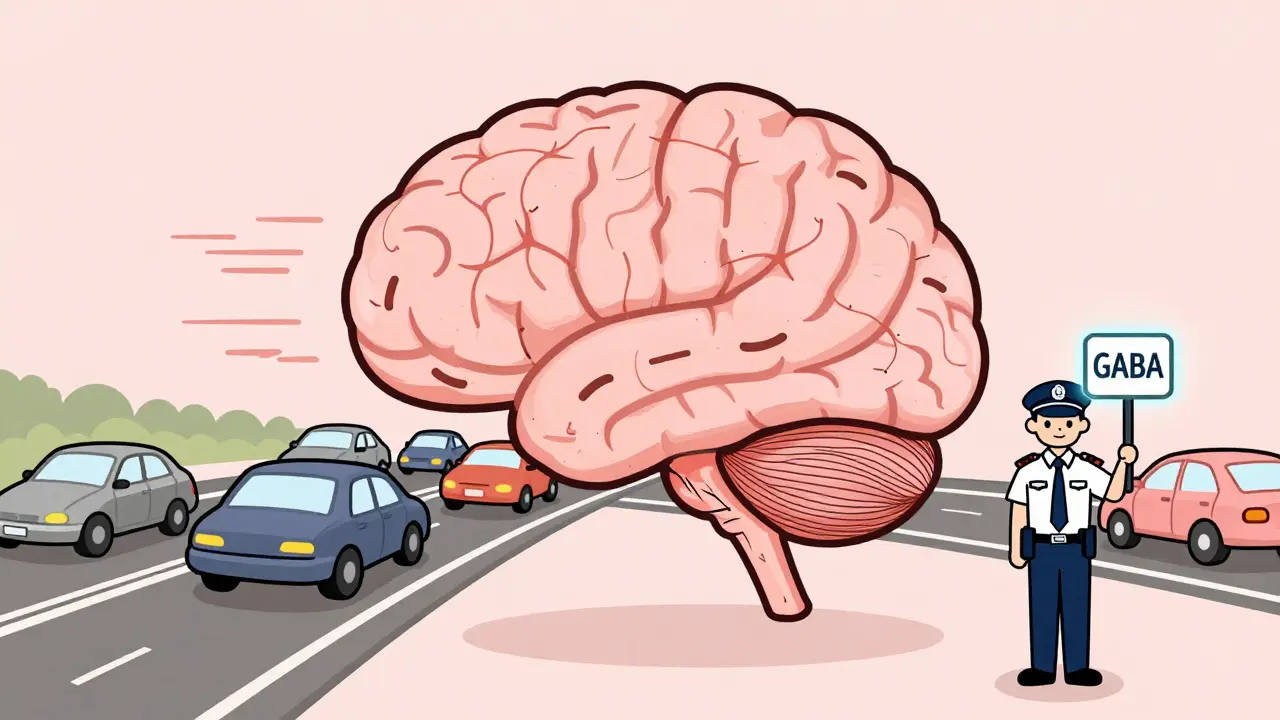
Imagine your brain is a busy highway. Too many cars, too much noise, too much stress-that’s what anxiety or panic feels like. Benzodiazepines act like traffic cops, slowing everything down by boosting a calming chemical called GABA. This isn’t magic. It’s chemistry. These drugs bind to specific receptors in your brain, making GABA work harder. The result? Faster calm. Within 30 to 60 minutes, a panic attack can ease. A racing heart slows. Muscles relax. That’s why doctors still reach for them when someone is in crisis.
But here’s the catch: they don’t fix the cause. They just mute the symptoms. And that’s fine-for a few days. Not for months. Not for years. The body adapts. The brain says, “Hey, we don’t need to make as much GABA anymore because the drug’s doing it for us.” That’s how dependence starts. Quietly. Slowly. Often without the patient even realizing it.
The real benefits: when they still make sense
Let’s be clear: benzodiazepines aren’t obsolete. They’re essential in specific situations. For example, if you’re having a seizure in the ER, midazolam can stop it in under a minute. If you’re going into surgery and your heart is pounding from fear, a dose of lorazepam can help you stay calm. For alcohol withdrawal, diazepam prevents dangerous tremors and seizures. In these cases, there’s no better tool.
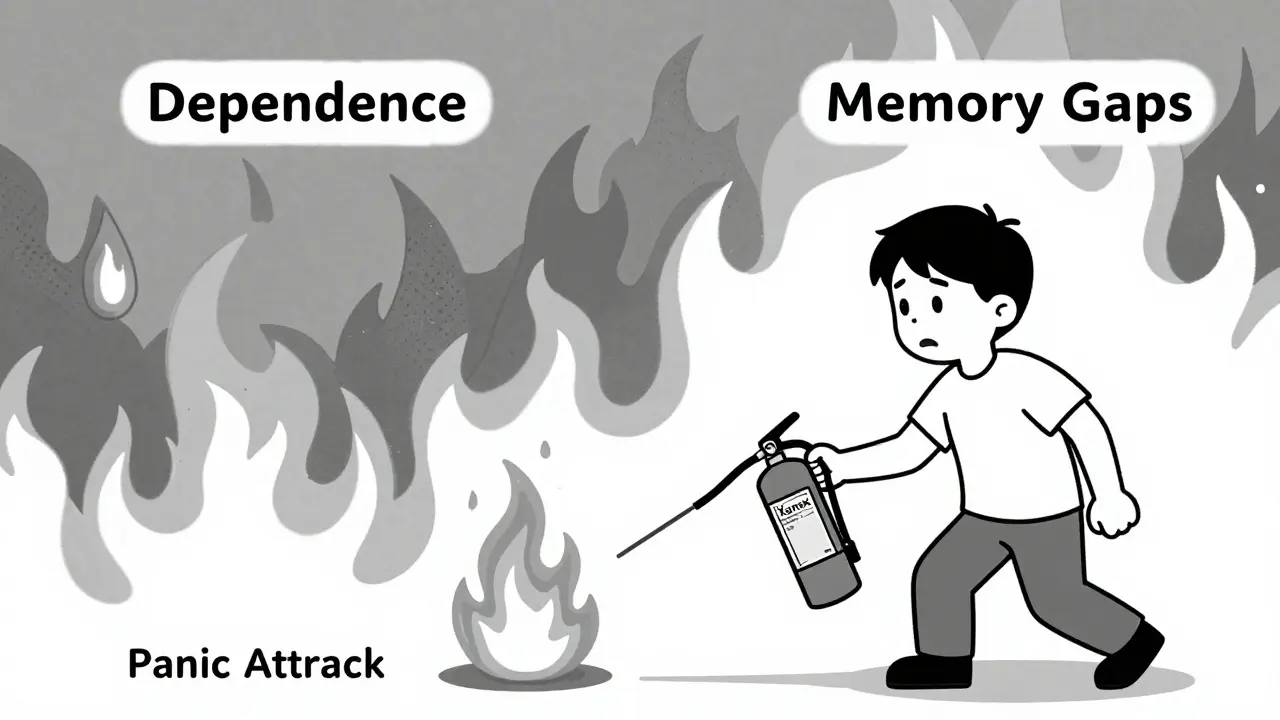
For panic attacks, alprazolam (Xanax) can be life-changing. People on Reddit’s r/Anxiety forum report that a single pill stopped their worst episodes-some for the first time in years. That’s real. That’s valuable. But only if used like a fire extinguisher: quick, targeted, and then put away.
Compare that to SSRIs like sertraline or escitalopram. Those take 4 to 6 weeks to work. But they don’t make you drowsy. They don’t cause memory gaps. And they don’t trap you in a cycle of needing more to feel the same. For long-term anxiety, antidepressants are the smarter play. Benzodiazepines? They’re the emergency backup.
The hidden dangers: dependence isn’t optional
Here’s what most people don’t realize: if you take benzodiazepines every day for more than 4 weeks, there’s a 30% to 50% chance you’ll become physically dependent. That’s not addiction. That’s physiology. Your brain rewired itself to need the drug to function normally. Stop it suddenly, and your nervous system goes into overdrive. Tremors. Insomnia. Heart palpitations. Even seizures.
One study found that 23% of people on prescribed doses had memory gaps-forgetting conversations, driving routes, or even meals. That’s anterograde amnesia. It’s not rare. It’s documented. And it happens even when people take their pills exactly as directed.
Older adults are especially at risk. The American Geriatrics Society says anyone over 65 should avoid these drugs entirely. Why? They increase the chance of falling by 50%. And long-term use raises dementia risk by 32%. That’s not a small trade-off.
How people get stuck-and how to get out
Most people don’t start with the goal of becoming dependent. They take a pill for a stressful week. Then another. Then a month. Then six. Doctors sometimes prescribe them for “as needed,” but patients end up taking them daily because the relief is so strong. And when they try to stop? That’s when the real trouble begins.
Withdrawal isn’t just uncomfortable. It’s dangerous. The Ashton Manual-the gold standard for tapering-says most people need 3 to 6 months to safely come off after long-term use. Some need longer. You can’t just quit cold turkey. Your body doesn’t work that way.
Successful tapers usually drop the dose by 5% to 10% every 1 to 2 weeks. Sometimes, doctors switch patients from a short-acting drug like alprazolam to a longer-acting one like diazepam. Why? Because diazepam leaves the body slowly, smoothing out the withdrawal spikes. It’s not about replacing one drug with another. It’s about giving your brain time to relearn how to calm itself without help.
What alternatives actually work
There are better ways to manage anxiety and insomnia that don’t come with a risk of dependence. For insomnia, cognitive behavioral therapy for insomnia (CBT-I) is more effective long-term than any sleep pill. It teaches you how to break the cycle of lying awake, worrying about not sleeping, and then using drugs to force it. Studies show CBT-I works for over 70% of people-and the benefits last years after treatment ends.
For anxiety, therapy like CBT or acceptance and commitment therapy (ACT) helps rewire how you respond to stress. Medications like SSRIs are safer for ongoing use. Even mindfulness and regular exercise reduce anxiety symptoms as much as some benzodiazepines-without the memory loss or fall risk.
And here’s something surprising: combining low-dose benzodiazepines with CBT cuts long-term dependence risk by 58%, according to a 2023 JAMA study. That’s not a coincidence. It means the drug can be part of the solution-if it’s not the whole solution.

Who shouldn’t take them-and why
Some people should never start benzodiazepines. That includes anyone with a history of substance abuse, including alcohol. It includes people over 65. It includes pregnant women. It includes anyone with sleep apnea-these drugs can shut down breathing during sleep.
And if you’re already taking them long-term? Don’t panic. But do talk to your doctor. Ask: “Is this still necessary?” “What’s my exit plan?” “Can we try therapy first?” Many clinics now use electronic alerts to flag prescriptions longer than 90 days. Kaiser Permanente cut long-term use by 37% just by making doctors pause and reconsider.
The big picture: are they still worth it?
Benzodiazepines aren’t going away. They’re still used in emergency rooms, ICUs, and for people with severe, treatment-resistant panic. But their role is shrinking. In France, doctors prescribe them at nearly 6 times the rate of the U.S. In the UK, NICE guidelines now say don’t start them for anxiety at all. The FDA added a boxed warning in 2020-its strongest alert-about abuse, dependence, and withdrawal.
The market is still growing, but the trend is clear: doctors are getting more cautious. Patients are asking more questions. And the science is telling us: use them briefly, wisely, and never alone.
What to do if you’re on them now
- If you’ve been taking them for less than 2 weeks: talk to your doctor about stopping. You likely won’t have withdrawal.
- If you’ve been taking them for more than a month: don’t quit on your own. Ask for a taper plan.
- If you’re feeling anxious when you try to skip a dose: that’s dependence. It’s not weakness. It’s biology.
- If you’re using them for sleep: consider CBT-I. It’s more effective and lasts longer.
- If you’re using them for anxiety: ask if therapy or an SSRI could replace them.
The goal isn’t to scare you. It’s to give you real information. Benzodiazepines can help. But they can also trap you. The difference is in how you use them-and when you decide to stop.




Comments
Prajwal Manjunath Shanthappa
Let’s be brutally honest: if you’re still prescribing benzos for ‘anxiety’ like it’s 2003, you’re not a doctor-you’re a pharmacy’s best friend. GABA modulation isn’t therapy; it’s chemical sedation masquerading as care. And don’t even get me started on the ‘as-needed’ myth-patients don’t take one pill, they take one pill, then another, then a whole damn box because the silence feels like victory. The Ashton Manual? Brilliant. But it’s a funeral dirge for people who trusted their prescribers. We’ve turned human suffering into a pharmacological buffet-and then acted shocked when the guests got addicted.
February 3, 2026 AT 15:26
Wendy Lamb
Important read. I’ve seen patients on benzos for years because no one offered CBT-I or SSRIs first. It’s not malpractice-it’s systemic neglect. The system rewards quick fixes. Therapy takes time. Insurance doesn’t cover it well. And doctors? They’re overworked. But that doesn’t excuse it. We can do better. Start with CBT. Always.
February 4, 2026 AT 04:13
Antwonette Robinson
Oh wow. A 32% increased dementia risk? Shocking. Next you’ll tell me oxygen causes lung cancer. 😏 Also, ‘don’t quit cold turkey’-what, did someone try to stop after one pill and start levitating? Please. If your brain can’t handle a 5% weekly taper, maybe you weren’t supposed to be on it in the first place. Also, ‘safety’ is just a word people use when they’re scared to feel their own emotions.
February 4, 2026 AT 09:48
Ed Mackey
Im not a doc but i had a friend who went through withdrawal from xanax after 8 months. it was brutal. insomnia, heart racing, felt like her brain was on fire. she switched to diazepam like they said and it helped a ton. but man, the mental fog? it took 6 months to clear. i wish someone had told her about CBT before she started. she didnt even know it was a thing.
February 4, 2026 AT 16:51
Jhoantan Moreira
This is one of the clearest, most compassionate summaries I’ve read on this topic. 🙏 The point about combining benzos with CBT is HUGE-most people don’t realize they can be a bridge, not a cage. Also, big shoutout to Kaiser Permanente for actually changing their systems. That’s the kind of institutional courage we need more of. Let’s stop treating symptoms and start treating people. 💪
February 4, 2026 AT 18:59
Justin Fauth
So now we’re telling Americans they can’t have a pill to chill out? Great. Let’s just send everyone to therapy in a country where therapy costs $200/hour and you wait 3 months for an appointment. Meanwhile, in Europe, they’re handing out benzos like candy and they’re still standing. Maybe instead of banning the tool, fix the system. Also, ‘dementia risk’-so what? I’m not dying of anxiety, I’m dying of bureaucracy.
February 6, 2026 AT 09:53
Meenal Khurana
My mom was on lorazepam for 12 years. She didn’t realize she was dependent until she tried to stop. She fell three times. Never got CBT. Now she’s off them, slowly. But she’s still scared. This info should be mandatory.
February 6, 2026 AT 14:55
Joy Johnston
Thank you for this meticulously referenced, clinically accurate, and ethically grounded exposition. The data on anterograde amnesia and the Ashton Manual’s tapering protocols are not merely informative-they are life-preserving. Clinicians who overlook the 30–50% dependence statistic are not practicing medicine; they are practicing negligence. The integration of CBT-I and SSRIs as first-line interventions is not a suggestion-it is the standard of care. This post should be required reading for all prescribers, pharmacists, and patients. The future of psychiatric care depends on this paradigm shift.
February 8, 2026 AT 06:43