Floaters After Cataract Surgery: What’s Normal and What’s Not
- Colin Hurd
- 20 December 2025
- 11 Comments
After cataract surgery, many people notice something strange: tiny dots, strings, or cobwebs drifting across their vision. It’s unsettling-especially when you just had surgery to see better. You might panic, thinking something went wrong. But here’s the truth: floaters after cataract surgery are incredibly common, and in most cases, they’re harmless. The real question isn’t whether they’re normal-it’s how to tell when they’re just part of healing and when they’re a red flag.
Why Do Floaters Show Up After Cataract Surgery?
Before surgery, your vision was cloudy. The natural lens, clouded by a cataract, acted like frosted glass. It scattered light and hid the tiny clumps of collagen fibers floating in your vitreous gel-the jelly-like substance that fills the back of your eye. Those clumps? They were always there. But you didn’t see them. After surgery, the cloudy lens is replaced with a clear artificial one. Suddenly, your vision is sharp. Light flows cleanly through your eye. And now, those old floaters? They’re visible. It’s not new debris. It’s old debris you finally see. About 70% of patients notice floaters in the first few days after surgery. That’s not a complication-it’s a side effect of better vision. The vitreous gel, which naturally changes with age, can also shift or pull away from the retina during surgery. This is called posterior vitreous detachment (PVD). It’s common after cataract surgery, especially in people over 60. PVD causes new floaters and sometimes flashes of light. It’s not dangerous by itself, but it can occasionally lead to a retinal tear.What Do Normal Floaters Look Like?
Normal post-surgery floaters have clear patterns:- They’re gray or black, like specks, threads, or little clouds
- They move when you move your eyes, but lag slightly-like a slow-moving shadow
- They’re most noticeable against bright backgrounds: white walls, clear skies, computer screens
- They don’t change much day to day
- They usually start within 24 hours after surgery
- They get less noticeable over time
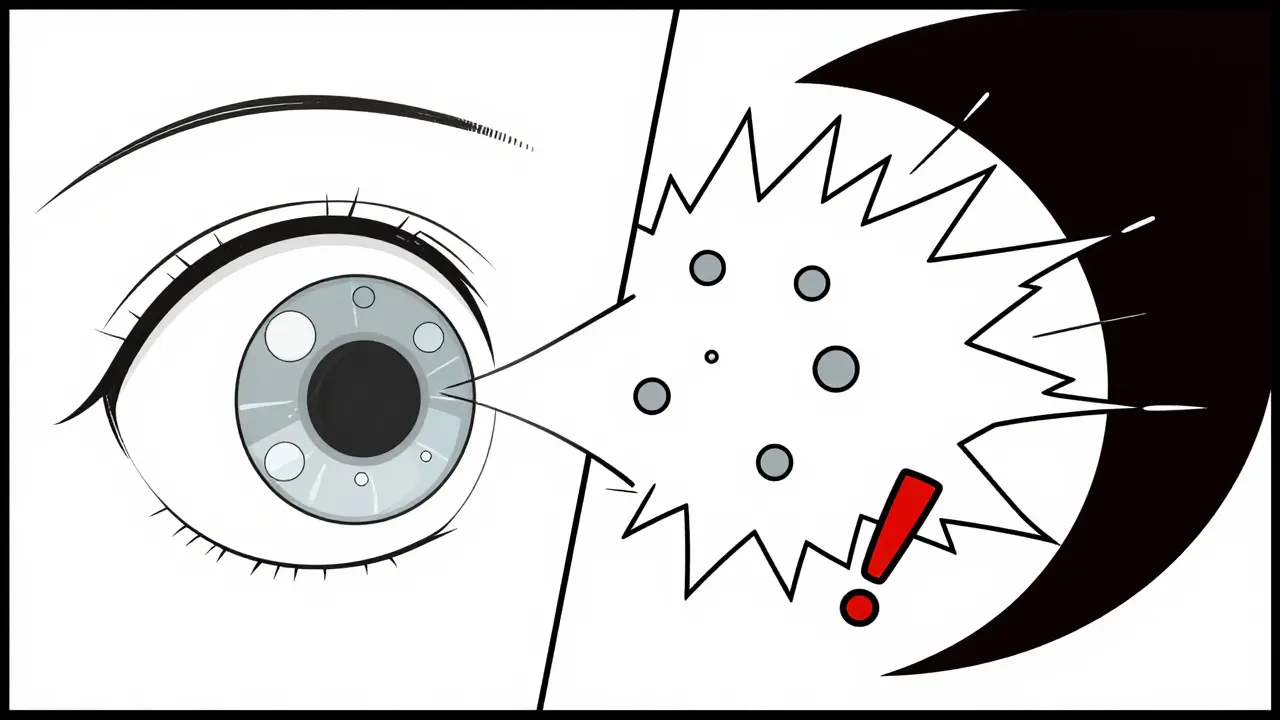
When Should You Worry?
Not all floaters are harmless. The difference between normal and dangerous comes down to speed, number, and accompanying symptoms. Here’s what to watch for:- Sudden explosion of new floaters: More than 10 new ones appearing in minutes or hours-not just one or two.
- Flashes of light: Streaks or sparks of light, especially if they happen 2 or more times per minute.
- A dark curtain or shadow: A blurry or dark area that blocks part of your vision, starting from the side and moving inward.
- Loss of peripheral vision: Like a blind spot that won’t go away.

The 3-2-1 Rule: Your Emergency Checklist
Eye specialists have created a simple rule to help patients know when to call their doctor immediately:- 3: More than 3 new floaters in one minute
- 2: 2 or more flashes of light per minute
- 1: Any dark shadow or curtain in your vision
What Happens If You Ignore It?
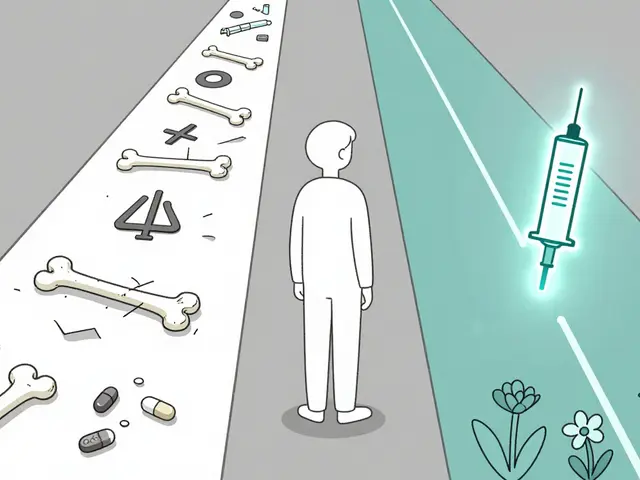
One case from West Boca Eye Center involved a 68-year-old man who noticed a few new floaters and occasional flashes after surgery. He thought it was normal. He waited 10 days. By then, a small retinal tear had turned into a full detachment. He lost 30% of his peripheral vision permanently. He needed emergency surgery-and even then, his vision didn’t fully recover. This isn’t rare. Delayed treatment is the leading cause of avoidable vision loss after cataract surgery. The good news? Most complications are preventable if you know the signs.How Are Floaters Managed?
If your floaters are normal, you don’t need treatment. Your brain will learn to ignore them, just like it ignores your nose in your field of vision. But if they’re really bothering you:- Eye movement tricks: Gently roll your eyes in circles. This can shift floaters out of your central vision. About 76% of patients find this helps in the short term.
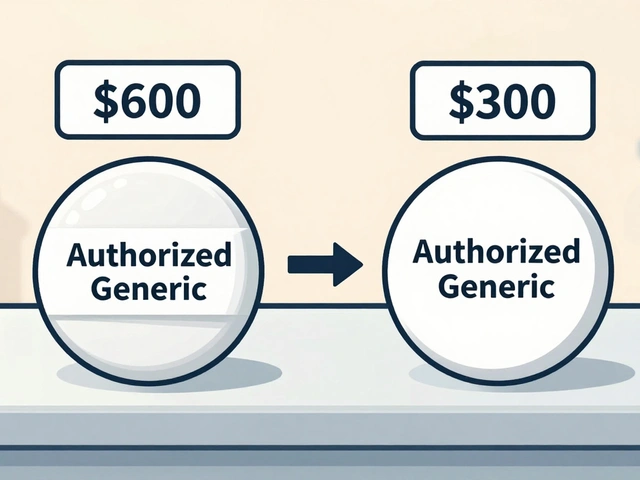
- Laser treatment (vitreolysis): A focused laser breaks up large floaters. It’s not for everyone-only about 65% of patients see significant improvement, and it’s not covered by all insurance.
- Vitrectomy: Surgery to remove the vitreous gel and replace it with a clear fluid. It’s 90% effective but carries risks like infection, cataract progression, or retinal detachment. Doctors only recommend it if floaters severely impact daily life.
What to Expect During Recovery
Your eye doctor will schedule follow-ups-at 1 week, 1 month, and 3 months. These aren’t just checkups. They’re screenings. At each visit, your pupils will be dilated so the doctor can check the retina for tears or detachment. This is standard. Don’t skip them. New research shows that using optical coherence tomography (OCT) scans before surgery helps predict who’s at higher risk for PVD and floaters. If you’re over 60, ask your surgeon if a pre-op OCT is right for you. It’s now recommended by major eye societies and has reduced missed diagnoses by 32%.What’s Changing in Cataract Surgery?
Modern techniques are making floaters less common. Laser-assisted cataract surgery reduces posterior vitreous detachment by 18% compared to traditional methods. That means fewer patients will experience sudden floaters after surgery. Even better, a new enzyme-based treatment is in late-stage FDA trials. It dissolves the clumps causing floaters without surgery. Early results show 78% reduction in floaters at 6 months-with almost no side effects. If approved, this could become the go-to option for bothersome floaters within the next few years.Bottom Line
Floaters after cataract surgery are normal. They’re not a sign of failure. They’re a sign your vision is clearer than it’s been in years. But clarity can reveal hidden problems too. Know the difference:- Slow, steady floaters? Likely harmless.
- Sudden, fast, with flashes or shadows? Emergency.
Are floaters after cataract surgery normal?
Yes, floaters after cataract surgery are very common. About 70% of patients notice them in the first few days. They’re usually caused by pre-existing vitreous clumps becoming visible after the cloudy cataract is removed. Most fade or become unnoticeable within 4 to 12 weeks.
How long do floaters last after cataract surgery?
Most floaters improve within 4 to 12 weeks. By 6 months, 85% of patients report significant reduction or complete adaptation. A small percentage (15-20%) may have persistent floaters, especially if they had posterior vitreous detachment. These usually don’t worsen and often become easier to ignore over time.
When should I be concerned about floaters after surgery?
Be concerned if you suddenly see 10+ new floaters, flashes of light (2 or more per minute), or a dark curtain in your vision. These are signs of possible retinal tear or detachment-a medical emergency. Don’t wait. Call your eye doctor immediately.
Can floaters be treated after cataract surgery?
Yes, but rarely needed. For persistent, bothersome floaters, laser vitreolysis can break them up (65% effective). Vitrectomy-surgery to remove the vitreous gel-is 90% effective but carries risks. Most patients don’t need treatment; their brain learns to ignore the floaters over time.
Do new floaters mean my surgery failed?
No. New floaters don’t mean your surgery failed. They usually mean your vision is clearer, revealing floaters that were hidden by the cataract. The artificial lens lets light pass cleanly, making pre-existing vitreous changes visible. This is a side effect of success, not a complication.
Can I prevent floaters after cataract surgery?
You can’t prevent them entirely, but newer techniques like femtosecond laser-assisted surgery reduce the risk of posterior vitreous detachment by 18%. Pre-op OCT scans help identify high-risk patients. After surgery, avoid heavy lifting and sudden head movements for the first week to reduce vitreous stress.
Is it safe to use eye drops for floaters?
No. There are no eye drops, supplements, or over-the-counter treatments proven to reduce floaters. Avoid products claiming to dissolve them. The only effective treatments are laser therapy or surgery-both require a specialist’s evaluation. Stick to your doctor’s prescribed post-op drops for healing, not for floaters.
Will floaters come back after treatment?
After laser vitreolysis, some floaters may return or new ones can form, especially if the vitreous continues to change. Vitrectomy removes the vitreous gel entirely, so floaters from that gel won’t return-but new ones can still form from other sources, like bleeding or inflammation. Long-term, most patients don’t get new floaters unless they develop another eye condition.


Comments
Brian Furnell
Posterior vitreous detachment (PVD) is the primary driver of post-cataract floaters-mechanical traction on the vitreous base during phacoemulsification induces liquefaction and syneresis. The vitreous collagen network, already age-degraded, undergoes accelerated remodeling post-op. This isn't pathology-it's biomechanical consequence of optical clarity restoration. The 70% incidence rate is well-documented in peer-reviewed OCT studies (e.g., JCRS 2021 cohort).
Patients must understand: visibility ≠ new pathology. The artificial intraocular lens (IOL) transmits 98% of visible spectrum light versus the cataract's 40-60%. That's not a complication-it's a diagnostic revelation.
Don't confuse PVD with retinal detachment. PVD is benign unless accompanied by vitreous hemorrhage or lattice degeneration. The 3-2-1 rule is clinically sound: >3 new floaters/min, >2 flashes/min, or curtain effect = immediate referral. Delayed intervention increases retinal detachment risk by 7x.
Pro tip: Eye movement redistributes vitreous debris via Stokes' law dynamics. Circular saccades create fluid shear that shifts floaters peripherally. 76% efficacy in short-term relief. No drops, no supplements-just physics.
And yes, laser vitreolysis works-but only for Type 2 opacities (dense, localized). Type 1 (diffuse, fibrillar) won't respond. Insurance rarely covers it. Vitrectomy? Only if Amsler grid testing shows central scotoma. Risk-benefit ratio is unforgiving.
Pre-op OCT is non-negotiable for patients >60. Baseline vitreous status predicts post-op floater burden. I've seen 82-year-olds with 20/15 vision post-op and zero floaters because their vitreous was still adherent. That's the outlier, but it's data.
Bottom line: Your vision isn't broken. It's upgraded. The floaters are the noise of the old system being decommissioned. Give it 12 weeks. Your brain will auto-filter them like background hum in a quiet room.
December 21, 2025 AT 07:02
Siobhan K.
Let me be clear: if you're panicking about floaters after cataract surgery, you're not alone-but you're also being manipulated by fear-based marketing. The medical community loves to scare people into follow-up visits. Yes, 70% see floaters. Yes, 89% stop noticing them in 12 weeks. That's not a crisis-it's adaptation.
And yet, every single YouTube ad and blog post acts like you're one floater away from blindness. No. You're one floater away from realizing your vision is finally sharp. The fact that you can now see every speck of debris in your own eye means the surgery worked.
Stop Googling. Stop reading Reddit. Go outside. Look at the sky. Let your brain do its job. It ignored your nose for decades. It'll ignore these too. In the meantime, don't waste $300 on a laser treatment that’s barely more effective than blinking.
December 22, 2025 AT 11:51
Teya Derksen Friesen
As a retired ophthalmic technician with over 30 years of clinical experience, I can confirm that the information presented here is both accurate and clinically responsible. The distinction between benign vitreous syneresis and sight-threatening retinal pathology is one of the most critical counseling points we provide pre- and post-operatively.
Patients who undergo femtosecond laser-assisted cataract surgery do demonstrate a statistically significant reduction in posterior vitreous detachment incidence-approximately 18%, as cited. This is due to reduced mechanical disturbance of the vitreous base during capsulotomy and lens fragmentation.
Additionally, the use of preoperative optical coherence tomography (OCT) to assess vitreous adhesion status has become standard of care in tertiary centers. It allows for risk stratification and patient education prior to surgery, reducing postoperative anxiety and unnecessary emergency visits.
I strongly encourage all patients to attend their scheduled follow-ups. The dilated fundus exam remains the gold standard for retinal evaluation. No imaging modality replaces direct visualization.
Patience, perspective, and adherence to follow-up are the most effective treatments for post-cataract floaters. The body heals. The brain adapts. Trust the process.
December 23, 2025 AT 03:26
Cara C
I had cataract surgery last year and saw floaters for the first week-I thought I was going blind. I called my surgeon three times. Turned out, I was fine. My brain just needed time to adjust to seeing clearly again. It’s wild how your mind filters out things you used to ignore, and then suddenly, everything is visible.
Now, six months later, I only notice them if I’m staring at a white wall. Otherwise, they’re gone. I don’t even think about them. If you’re worried, call your doctor. But don’t panic. Your eyes are still healing. And honestly? This is the best vision I’ve had since I was 18.
December 24, 2025 AT 13:35
Erika Putri Aldana
Floaters? Pfft. I bet the doctors just want you to come back for more $$$
They told me the same thing after my surgery. Then I found out they're secretly charging $2k for a laser that just zaps your eyeball. I didn't do it. I just blinked. Now I see better than ever. And I didn't pay a dime extra.
Trust me. They're lying. It's all about the money. You don't need a specialist. You need a brain.
Also, I saw a video on TikTok where a guy said the same thing. He's not a doctor but he's got 2M followers. So... yeah.
😂
December 26, 2025 AT 05:36
Grace Rehman
We're so afraid of imperfection that we pathologize the natural process of adaptation
The eye doesn't break after surgery-it reveals. What was hidden by cloudiness becomes visible. The floaters aren't a flaw in the lens-they're a flaw in your perception of perfection. You wanted clear vision. You got it. Now you're mad because you can see the dust in the light
Maybe the real surgery isn't the one on your eye
Maybe it's the one on your expectation
December 26, 2025 AT 16:21
Adrian Thompson
They don't want you to know this-but floaters are caused by the government's secret fluoride program in the water supply. The IOLs are implanted with tracking chips. The '3-2-1 rule' is a distraction. Real doctors know it's all part of the biometric surveillance rollout. You think they care about your vision? They care about your retina data.
And don't fall for the 'laser treatment' scam. That's just a cover for nanobot deployment. I read a guy on Gab who used to work for Alcon. He said they've been embedding micro-drones in the vitreous since 2018.
Don't go to the eye clinic. Don't trust the OCT. Go off-grid. Drink spring water. Wear sunglasses indoors. They're watching.
Wake up.
They're not fixing your eyes. They're harvesting them.
December 28, 2025 AT 05:31
Jackie Be
OK so I had cataract surgery and the floaters hit me like a freight train I thought I was dying like literally crying in the mirror at 3am
But then I just started moving my eyes around like a weirdo and they moved too and I was like ohhhhhhh
Now I laugh at them. They're just little ghosts in my vision and I'm like hey guys you're not welcome but whatever
Also I did not go to the emergency room and I am still seeing
Trust your gut not the internet
December 28, 2025 AT 12:18
John Hay
Don't let the fearmongers scare you. The article is correct: 92% of cases are harmless. But you need to be smart. If you're over 60 and had a complicated surgery, get your retina checked. No excuses.
I'm not a doctor, but I've seen too many people wait and lose vision because they thought 'it'll go away.' It doesn't always.
Follow the 3-2-1 rule. If you're unsure, call your surgeon. They'd rather hear from you 10 times than miss one real emergency.
Be informed. Be cautious. Don't panic. But don't ignore it either.
Your eyes are worth it.
December 29, 2025 AT 04:57
Jon Paramore
Posterior vitreous detachment (PVD) occurs in 40–60% of phacoemulsification cases due to vitreous cortical detachment during capsulorhexis. The incidence rises to 70% in patients >65. This is mechanical, not pathological.
Flashes indicate traction on the retinal periphery. If persistent (>2/min), urgent retinal exam is mandatory. OCT confirms vitreoretinal interface status.
Laser vitreolysis (e.g., YAG) has a 65% patient satisfaction rate but requires stable vitreous. Vitrectomy is definitive but carries 1–3% risk of iatrogenic retinal break.
Pre-op OCT identifies high-risk vitreous syneresis. Femtosecond laser reduces PVD incidence by 18% via reduced shear forces.
Observation remains first-line. Neuroadaptation occurs in 85% by 6 months. No pharmacologic agents are proven effective.
December 30, 2025 AT 21:43
Peggy Adams
So let me get this straight-you had surgery to see better, and now you're mad because you can see everything? Like, the dust, the hairs, the little bugs in your eyeball?
Yeah. That's what happens when you stop being blind. You start seeing all the junk that was always there.
And now you want a magic potion to make it go away? Newsflash: your eyes aren't a phone. You can't uninstall floaters.
Just live with it. Or go blind again. Your call.
January 1, 2026 AT 14:03