Generic vs Brand-Name Drugs: Long-Term Safety Studies Explained

- Colin Hurd
- 4 February 2026
- 14 Comments
Generic drugs are medications that contain the same active ingredients as brand-name versions but are sold at a lower cost. In 2022, generics accounted for 92% of all prescriptions filled in the United States while representing only 23% of total drug spending, according to IQVIA data. This massive cost savings has made generics a cornerstone of modern healthcare. But as millions rely on these medications daily, a critical question remains: are they as safe as brand-name drugs over the long term?
How the FDA Ensures Generic Drug Safety
The U.S. Food and Drug Administration (FDA) the federal agency responsible for regulating drugs and medical products established the modern generic drug approval pathway through the Hatch-Waxman Act of 1984. This law requires generics to prove bioequivalence to their brand-name counterparts. Bioequivalence means the 90% confidence interval for the ratio of geometric means (generic to brand) for both area under the curve (AUC) and maximum concentration (Cmax) must fall entirely within the 80-125% range. This standard, documented in the FDA's Orange Book, ensures that the drug is absorbed similarly in the body. For example, a generic version of a blood pressure medication must deliver the same active ingredient into the bloodstream at a rate and extent comparable to the brand-name version.
What Long-Term Studies Reveal
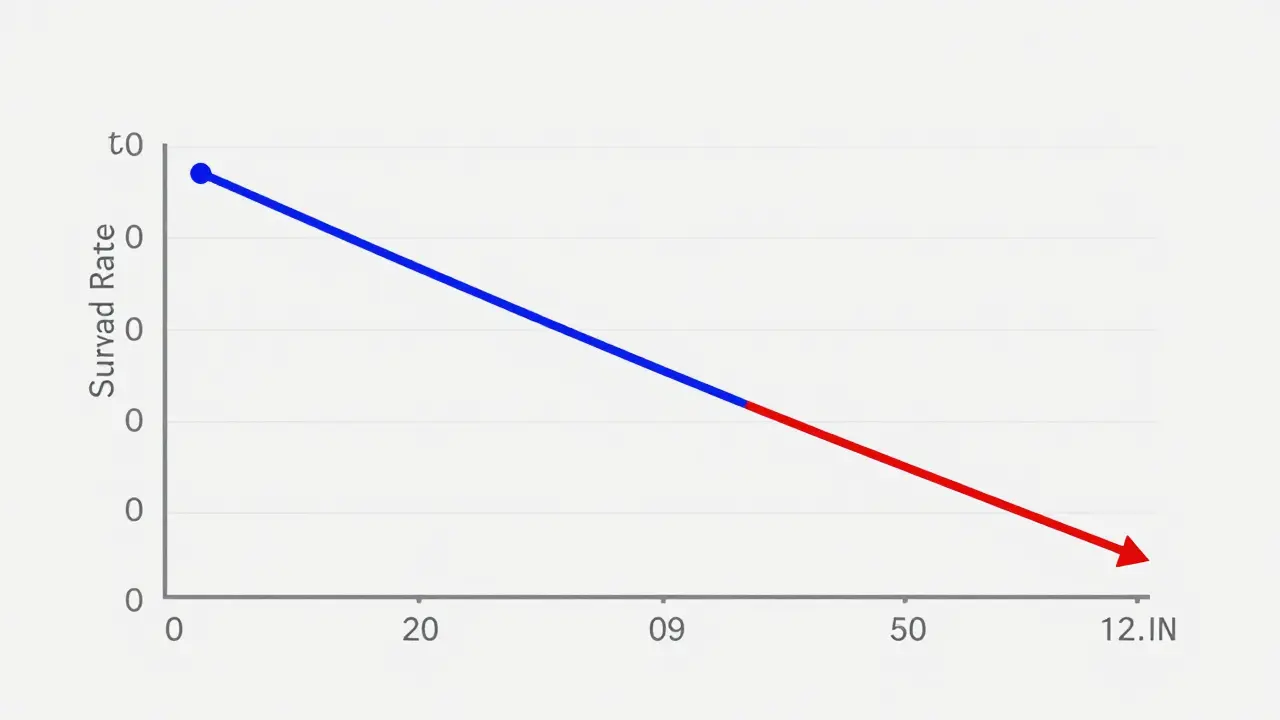
While bioequivalence testing focuses on short-term absorption, long-term safety studies paint a more complex picture. A landmark 2020 study published in Scientific Reports analyzed nearly all insured persons in Austria from 2007-2012. For antihypertensive medications specifically, the study found branded drugs were associated with 53.8 deaths per 1,000 patient-years compared to 30.2 deaths for generics. Five-year cumulative survival rates were 77.8% for branded versus 85.9% for generic users. The authors concluded that 'generic medications were at least similar, and in some cases superior, to their branded counterparts regarding mortality and major adverse cardiac events.' However, other studies tell a different story. Case reports documented in the PMC (2013) article 'Safety and efficacy of generic drugs with respect to brand formulation' described patients who experienced clinical deterioration after switching from brand to generic. One patient taking generic ciprofloxacin had persistent symptoms that resolved after switching back to the brand version. Another saw worsening fever until returning to the brand-name drug.
Manufacturing Location and Safety
Where a drug is manufactured matters significantly for safety. A 2018 Ohio State University study found generic drugs made in India had 54% higher rates of severe adverse events (including hospitalization and death) compared to equivalent drugs produced in the United States. For instance, Indian-manufactured generic ciprofloxacin showed a 62% higher rate of severe adverse events leading to hospitalization. This wasn't due to the generic status itself but the manufacturing location. The FDA's Adverse Event Reporting System (FAERS) data shows similar patterns-drugs from certain countries consistently report higher adverse events. This highlights that not all generics are created equal; the manufacturer's location and quality control practices play a crucial role.
Expert Opinions on Safety
Experts remain divided on the long-term safety of generics. The FDA and major medical organizations like the American Medical Association maintain that generics are therapeutically equivalent to brands. However, Dr. Aaron Kesselheim of Harvard Medical School, lead author of multiple studies on generic drug safety, notes that 'while most generics perform equivalently to brands, there are documented cases where critical differences exist, particularly for narrow therapeutic index drugs like warfarin, levothyroxine, and certain anti-epileptics.' A 2017 study of levothyroxine generics showed 12.3% higher rates of thyroid-stimulating hormone (TSH) level fluctuations compared to brand Synthroid. This matters because even small variations in these drugs can have serious health consequences. For example, a patient taking a generic version of levothyroxine might experience uncontrolled hypothyroidism or hyperthyroidism due to slight differences in absorption.

Real-World Patient Experiences
Real-world user experiences reflect this complexity. Reddit discussions on r/pharmacy (April 2023) contain numerous anecdotes. One highly-upvoted post (1,842 upvotes) described a patient whose seizure frequency increased from 1-2 per month to 8-10 per month after switching from brand Lamictal to generic lamotrigine, returning to baseline after switching back. Conversely, a thread on PatientsLikeMe (2022) analyzing 3,842 patient reports on hypertension medications found 78.4% of users reported identical effectiveness between brand and generic versions, with only 12.6% reporting decreased effectiveness with generics and 9.0% reporting improved effectiveness. The FDA's FAERS database shows 1,247 adverse event reports mentioning 'generic drug ineffective' between 2018-2022 compared to 289 for brand-name drugs, though this must be interpreted with caution given the vastly higher volume of generic prescriptions.
Current Consensus and Recommendations
Current consensus among regulatory agencies maintains that generics are therapeutically equivalent to brands for most medications, but acknowledges challenges with 'complex generics' including drug-device combinations (like inhalers), long-acting injectables, and topical products where traditional bioequivalence testing may be inadequate. The FDA issued new guidance for 'complex generic drug development' in January 2022 addressing these challenges. Meanwhile, healthcare systems globally continue to prioritize generics for cost savings. For patients, the key takeaway is to monitor how your body responds to generics, especially for medications with narrow therapeutic indices. If you notice changes in effectiveness or side effects after switching, consult your healthcare provider immediately. For critical medications like warfarin or levothyroxine, staying on the same manufacturer's version (even if generic) can minimize variability.
Are generic drugs as safe as brand-name drugs?
For most medications, yes. Regulatory agencies like the FDA require generics to meet strict bioequivalence standards. However, long-term safety studies show nuanced differences. For example, a 2020 Austrian study found generics had lower mortality rates for antihypertensive drugs, while other studies show certain individuals experience issues with specific generics. The key is that most generics are safe, but vigilance is needed for narrow therapeutic index drugs.
Why do some people experience issues after switching to generics?
Differences in inactive ingredients, manufacturing processes, or bioavailability can cause reactions in sensitive individuals. For example, a patient switching from brand-name Ciproxin to generic ciprofloxacin might experience persistent symptoms due to variations in how the drug is absorbed. This is especially true for drugs with narrow therapeutic indices where small changes in blood levels can have significant effects.
Which medications should I be cautious about when choosing generics?
Medications with narrow therapeutic indices require extra caution. These include anticoagulants like warfarin, thyroid medications like levothyroxine, and anti-seizure drugs like phenytoin. Even small variations in blood concentration can lead to serious health issues. Always consult your doctor before switching generics for these medications.
How does manufacturing location affect generic drug safety?
Manufacturing location significantly impacts safety. A 2018 Ohio State University study found Indian-made generics had 54% higher rates of severe adverse events compared to U.S.-made versions. For instance, Indian ciprofloxacin showed 62% higher hospitalization rates. This is due to differences in quality control and manufacturing standards between countries. Always check the manufacturer's location on your prescription label.
What should I do if I think my generic medication isn't working?
Contact your healthcare provider immediately. Do not stop taking the medication without medical advice. Your provider may switch you back to the brand-name version or a different generic manufacturer. For critical medications like warfarin or levothyroxine, blood tests may be needed to check therapeutic levels. Document any side effects or changes in symptoms to help your doctor make an informed decision.




Comments
Bella Cullen
Yeah, whatever. I've never had a problem.
February 6, 2026 AT 07:29
Sam Salameh
American generics are the best. Period.
February 6, 2026 AT 10:52
Cullen Bausman
The FDA's requirements ensure safety. End of discussion.
February 6, 2026 AT 13:50
Dina Santorelli
Another lazy take. Studies show mixed results, but you wouldn't know that.
February 7, 2026 AT 13:00
Carol Woulfe
The FDA is just a puppet of big pharma. They don't want you to know the truth.
February 8, 2026 AT 23:57
Georgeana Chantie
I don't care what the studies say, brand names are better. 😎
February 9, 2026 AT 03:58
Arjun Paul
Brand names are always better. Generics are just a rip-off.
February 9, 2026 AT 04:01
Danielle Vila
Hey everyone, I've been researching this a lot. Did you know that the FDA's bioequivalence standards are based on short-term studies? Long-term effects aren't always covered. For example, some generics might have different inactive ingredients that cause issues over time. I've read about patients who had seizures after switching to generic Lamictal. The FDA's data shows adverse events, but they're not transparent. Big pharma is pushing generics to save money, not for patient safety. The manufacturing process for Indian generics is often subpar. They have higher rates of adverse events. The FDA should require more rigorous testing for long-term safety. People need to be aware of the risks. I've seen too many cases where patients suffered because of generics. It's a conspiracy. The government and drug companies are in cahoots. We need to demand better standards. This is a public health crisis. Don't trust the FDA. They're not looking out for us.
February 10, 2026 AT 10:40
Thorben Westerhuys
I've seen so many cases where generics failed!
They're not safe!
People are getting hurt!
We need to do better!
The FDA is failing us!
It's a disaster!
I can't believe this is happening!
We need to hold them accountable!
This is a public health emergency!
Don't trust the system!
It's all a lie!
The pharmaceutical companies are lying to us!
We need to fight for our health!
This is unacceptable!
It's time to take action!
February 11, 2026 AT 17:56
Laissa Peixoto
While some cases exist, most generics are safe. The FDA's standards are strict for most drugs. However, for narrow therapeutic index drugs like warfarin or levothyroxine, vigilance is needed. Always consult your doctor before switching. Most people won't have issues, but it's important to monitor your health. The key is informed choice. Don't let fear drive decisions; use data and professional advice. Studies show generics are effective for the vast majority. But for certain medications, consistency matters. Check with your pharmacist about the manufacturer. Stay informed, but don't panic. The FDA has rigorous testing for bioequivalence. Most generics are as safe as brands. But for critical drugs, stick to the same manufacturer. It's about balancing cost and safety. Always communicate with your healthcare provider.
February 12, 2026 AT 04:08
Joyce cuypers
I've used generics for years and they work great! No issues at all. Always check with your doc tho. They're reliable and save money. Don't worry too much!
February 13, 2026 AT 23:29
anjar maike
👍 Good point! Studies show some differences though.
February 15, 2026 AT 00:18
Lana Younis
Genetics vs brand names-need to know the difference. For example, levothyroxine generics can vary a bit. Always check with your doc. The FDA has guidelines for complex generics. But for most meds, generics are fine. Just be aware of your body's response.
February 16, 2026 AT 22:14
divya shetty
Indian-manufactured generics are often unsafe. The FDA should ban them.
February 17, 2026 AT 15:20