How Food Affects Medication Side Effects: What Patients Need to Know
- Colin Hurd
- 16 January 2026
- 9 Comments
When you take a pill, you might think the medicine works the same no matter what you’ve eaten. But that’s not true. What you eat - or don’t eat - can change how your body handles medication. Sometimes food makes a drug work better. Other times, it turns a mild side effect into a dangerous one. This isn’t theoretical. It’s happening right now to millions of people who don’t realize their breakfast is fighting their heart pill or their grapefruit juice is making their cholesterol drug too strong.
Why Food Changes How Medicines Work
Food doesn’t just fill your stomach. It changes your body’s chemistry. When you eat, your stomach acid levels shift, your blood flow to the gut changes, and enzymes that break down drugs get turned on or off. These changes can make a medication absorb too slowly, too quickly, or not at all.There are three main ways food messes with meds:
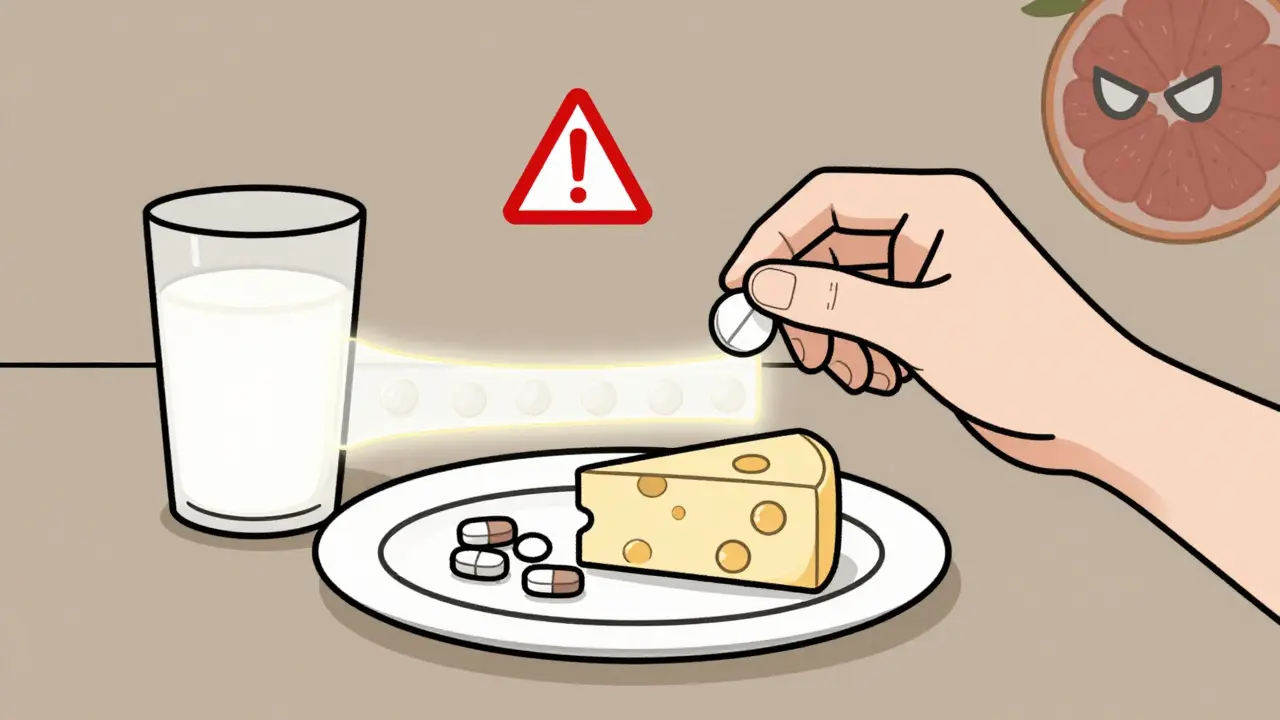
- Absorption problems: Food can block a drug from entering your bloodstream. Calcium in dairy, for example, binds to antibiotics like tetracycline and cuts absorption by half.
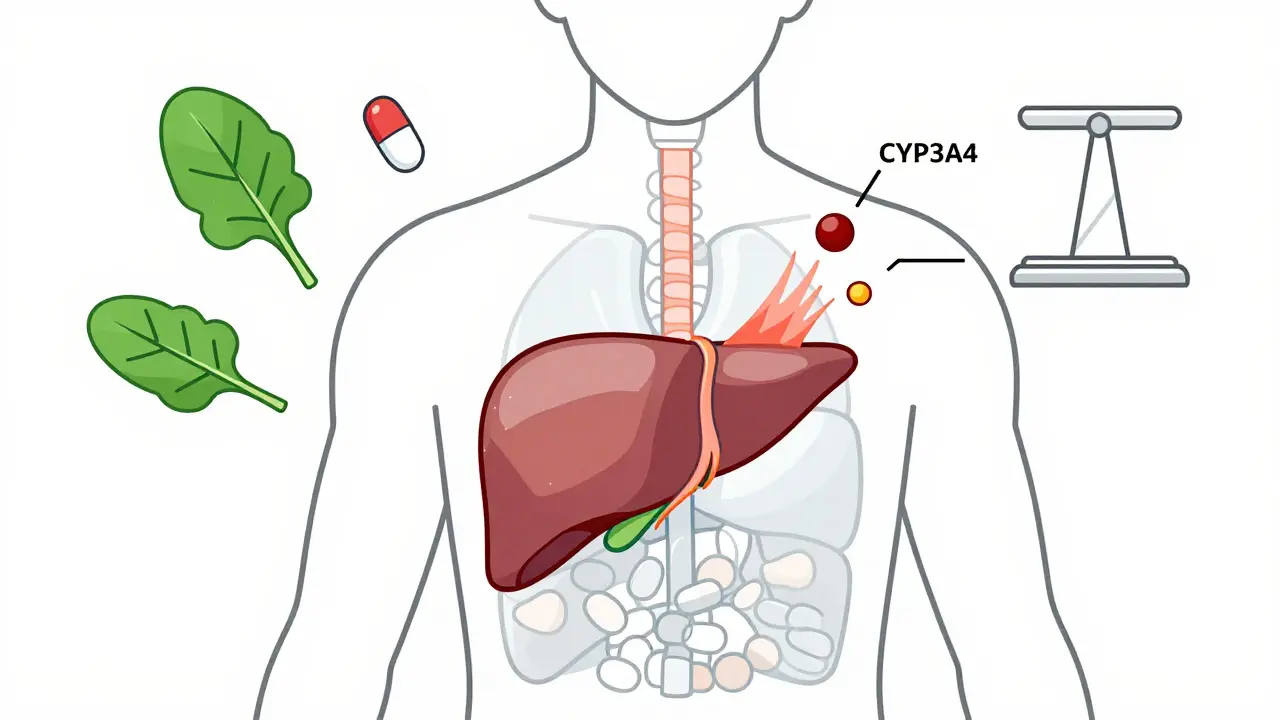
- Metabolism changes: Some foods, like grapefruit juice, shut down liver enzymes that normally break down drugs. That means the drug builds up in your blood - sometimes to toxic levels.
- Opposite effects: Vitamin K in spinach and kale directly counteracts warfarin, a blood thinner. If you eat a big salad one day and none the next, your blood can clot or bleed dangerously.
The FDA says 42% of serious drug reactions involve food. That’s not rare. It’s common. And most people have no idea.
Medications That Hate Food (And What to Do)
Some drugs need an empty stomach to work. If you take them with food, you might as well not take them at all.Levothyroxine (for thyroid): This drug needs to be taken at least 60 minutes before breakfast. A 2022 JAMA study found that taking it with food cuts its effectiveness by 34%. That means you could still feel tired, gain weight, or have high cholesterol - even if you’re taking your pill every day.
Antibiotics like ciprofloxacin and tetracycline: These are wiped out by calcium. Milk, yogurt, cheese, even calcium-fortified orange juice - if you have any of these within 2 hours before or after your pill, you’re getting maybe 10% of the dose. That’s not enough to kill bacteria. It just teaches them to fight back.
Proton pump inhibitors (omeprazole, esomeprazole): These drugs work best when taken 30 to 60 minutes before your first meal. If you take them after eating, they won’t block stomach acid as well. Your heartburn might come back harder.
Rule of thumb: If your prescription label says "take on empty stomach," wait at least one hour before eating - or two hours after eating. Don’t guess. Timing matters.
Medications That Need Food (And Why)
Not all drugs hate food. Some need it to work - or to keep you from getting sick.NSAIDs like ibuprofen and naproxen: These can irritate your stomach lining. A 5-year Mayo Clinic study showed 15% of people who took them on an empty stomach developed ulcers. That number dropped to 4% when they took the pill with food. Eating doesn’t make the painkiller stronger - it just protects your gut.
Statins like simvastatin and atorvastatin: These cholesterol drugs are absorbed better with food. But here’s the catch: grapefruit juice makes them absorb too well. One glass of grapefruit juice can spike simvastatin levels by 330%. That’s not just a side effect - it’s a risk of muscle damage, kidney failure, and even death.
Antifungals like griseofulvin and antivirals like ritonavir: These need fat to get into your system. Take them with a meal that has real fat - eggs, nuts, avocado, butter - not a bowl of rice.
Don’t assume food is always good. Some drugs need food to work. Others need food to be safe. You have to know which is which.
The Grapefruit Trap
Grapefruit juice is the most dangerous food-drug interaction most people don’t know about. It’s not just grapefruit. Seville oranges, pomelos, and even some limes can do the same thing.This juice blocks an enzyme called CYP3A4 in your gut. That enzyme normally breaks down dozens of drugs before they enter your blood. When it’s blocked, the drug floods your system.
Medications affected include:
- Statins: simvastatin, lovastatin, atorvastatin
- Blood pressure drugs: felodipine, nifedipine
- Immunosuppressants: cyclosporine, tacrolimus
- Anti-anxiety meds: buspirone
- Erectile dysfunction drugs: sildenafil (Viagra)
The FDA reports grapefruit interactions cause over 1,100 emergency room visits every year in the U.S. alone. And it’s not just juice. Eating half a grapefruit can do the same thing. The effect lasts more than 24 hours. So even if you drink grapefruit juice at breakfast and take your pill at night - you’re still at risk.
If you’re on any of these meds, skip grapefruit completely. No exceptions. No "just a little."
Warfarin and Vitamin K: The Balancing Act
Warfarin (Coumadin) is one of the most common blood thinners. It’s also one of the most sensitive to diet.Vitamin K helps your blood clot. Warfarin blocks it. So if you eat a lot of vitamin K - like cooked spinach (483 mcg per cup), kale, broccoli, or Brussels sprouts - warfarin can’t work as well. Your blood might clot. If you suddenly eat almost no vitamin K, warfarin works too well. You could bleed internally.
The fix? Don’t avoid vitamin K. Just keep it steady. The American Heart Association says patients who keep their daily vitamin K intake within 10-15% of their usual amount have 32% fewer dangerous INR fluctuations.
That means: if you usually eat spinach twice a week, keep doing it. Don’t swap it out for lettuce one week and then go back to spinach the next. Consistency beats perfection. Use a food diary. Or use an app like MyMedSchedule - it tracks your meals and flags vitamin K spikes.
What You Should Do Right Now
You don’t need to memorize every food-drug interaction. But you do need a system.- Read the label. Look for "take on empty stomach," "take with food," or "avoid grapefruit." If it’s not clear, ask your pharmacist.
- Ask your pharmacist. Pharmacists are trained for this. They see your full list of meds and your diet. They can spot conflicts your doctor might miss.
- Keep a food and med log. Write down what you eat and when you take your pills. Even for a week. You might notice a pattern - like headaches after eating cheese with your blood pressure pill.
- Use a pill organizer with times. Many people miss interactions because they take meds at random times. A simple organizer with AM/PM slots helps you stick to timing.
- Check new prescriptions. Every new drug you start could have a food interaction. Don’t assume it’s safe just because your last one was.
A 12-hospital study found that patients who used visual medication schedules cut food-drug interaction errors by 47%. That’s not magic. That’s clarity.
What’s Changing in 2026
The rules are getting stricter. Since January 1, 2025, Medicare Part D requires pharmacists to counsel every senior starting a high-risk medication on food interactions. That’s 12.7 million people a year.Also, the FDA now requires all new drug labels to include specific food interaction instructions - not vague warnings, but exact timing: "Take 1 hour before breakfast," "Avoid dairy for 4 hours," "Do not consume grapefruit."
And new tools are coming. Apps like MyMedSchedule use AI to build custom schedules based on your meals, sleep, and meds. In a 2023 trial, users had 35% fewer interactions.
This isn’t about being perfect. It’s about being aware. You don’t have to become a nutritionist. You just need to know: food isn’t neutral. It’s part of your treatment.
Common Myths About Food and Meds
- Myth: "All meds should be taken with food to protect my stomach."
Truth: Only some. Levothyroxine, antibiotics, and thyroid meds can fail if taken with food. - Myth: "I can drink grapefruit juice if I wait a few hours."
Truth: The enzyme block lasts over 24 hours. Waiting doesn’t help. - Myth: "If I don’t feel side effects, the interaction isn’t happening."
Truth: Many interactions build up slowly. Warfarin levels can be off for weeks before you bleed. Grapefruit can damage muscles without pain. - Myth: "Natural supplements are safe with my meds."
Truth: St. John’s Wort, garlic, ginkgo, and even high-dose vitamin E can interfere with blood thinners, antidepressants, and heart meds.
Don’t trust assumptions. Trust facts. Ask your pharmacist.
Can I take my medication with coffee?
Coffee can interfere with some medications. It slows the absorption of thyroid meds like levothyroxine and can raise blood pressure when taken with certain antidepressants or stimulants. For most people, waiting 30-60 minutes after taking your pill before drinking coffee is safe. But if you’re on a blood thinner, an antibiotic, or a psychiatric med, ask your pharmacist. Caffeine isn’t always harmless.
What if I forget to take my pill on an empty stomach?
If you realize within 30 minutes of eating, wait until your stomach is empty again - usually 2 hours after your last meal - then take it. If it’s been longer than 2 hours, don’t double up. Skip the dose and take your next one at the regular time. Taking two pills at once can cause overdose. Always call your pharmacist if you’re unsure. They’ll tell you what’s safe.
Do herbal supplements count as food?
Yes. Supplements like St. John’s Wort, garlic pills, ginkgo biloba, and even high-dose fish oil can interact with medications just like food. St. John’s Wort can make birth control, antidepressants, and heart meds fail. Garlic and ginkgo can thin your blood and increase bleeding risk with warfarin. Always tell your pharmacist what supplements you take - even if you think they’re "natural."
Can alcohol make medication side effects worse?
Absolutely. Alcohol can increase drowsiness with painkillers, sedatives, and antidepressants. It can spike blood pressure with some heart meds. With metronidazole (an antibiotic), alcohol causes severe nausea and vomiting. Even one drink can be risky. If your med label says "avoid alcohol," it’s not a suggestion. It’s a warning.
Is it safe to take all my pills at once with breakfast?
No. Many medications can’t be taken together. Calcium in dairy can block antibiotics. Fiber can trap blood pressure drugs. Grapefruit juice can overload statins. Taking everything at once doesn’t save time - it creates dangerous mixtures. Use a pill organizer with separate slots for morning, afternoon, and night. Follow timing instructions for each one. Safety isn’t about convenience.
Final Thought: Your Body, Your Meds, Your Rules
You’re not just taking pills. You’re managing a system. Food, drink, timing, and habits all play a role. The goal isn’t to eat perfectly. It’s to be consistent. To know what matters. To ask questions.One patient I know took her blood pressure pill with grapefruit juice for years. She didn’t feel sick. She didn’t know she was risking muscle damage. When her pharmacist pointed it out, she switched to orange juice. Her blood pressure stabilized. Her muscle pain disappeared. She didn’t change her diet. She just changed one thing.
That’s all it takes.




Comments
Bobbi-Marie Nova
I took my levothyroxine with my oatmeal for 3 years. Turns out I was just paying $200/month to make expensive pee. 🤦♀️ Now I take it with a glass of water at 5 AM before the dog even wakes up. Life changed.
January 17, 2026 AT 10:26
Stephen Tulloch
Bro. Grapefruit juice is basically liquid biohack sabotage. I took my simvastatin with it because "it’s healthy". Ended up in the ER with rhabdo. Now I drink water. Or juice that doesn’t try to kill me. 🍊☠️
January 19, 2026 AT 06:55
Corey Chrisinger
It’s wild how we treat medicine like candy but food like sacred scripture. We’ll eat 3 bags of chips and call it self-care, but a 30-minute window before a pill? That’s "too rigid." We’ve normalized ignorance as convenience.
January 19, 2026 AT 23:42
kanchan tiwari
THE GOVERNMENT IS HIDING THIS. WHY IS GRAPEFRUIT JUICE STILL SOLD WITH WARNINGS ON THE BOTTLE BUT NOT ON THE MEDICATION LABELS? THEY WANT US SICK SO WE BUY MORE DRUGS. I’VE BEEN TAKING MY BP MED WITH ORANGE JUICE SINCE 2020 AND I’M STILL ALIVE. THEY’RE LYING TO YOU.
January 21, 2026 AT 21:23
Christina Bilotti
I’m sorry, but if you can’t follow a 60-minute window between food and levothyroxine, maybe you shouldn’t be trusted with a pill organizer. This isn’t rocket science. It’s biology. And if you’re still asking if coffee is okay, you’re not ready for adulthood.
January 23, 2026 AT 12:14
vivek kumar
The FDA data is solid - 42% of serious drug reactions involve food. But the real issue is systemic: pharmacists are overworked, doctors don’t prioritize counseling, and patients are expected to self-educate on complex pharmacokinetics. This isn’t patient failure. It’s healthcare infrastructure collapse.
January 24, 2026 AT 13:38
Henry Ip
My mom had a stroke from warfarin fluctuations because she ate kale salad one week and nothing the next. We started using MyMedSchedule. Now she takes her meds with the same amount of greens every day. No drama. No ER trips. Just consistency. You don’t need to be perfect - just steady.
January 25, 2026 AT 16:59
Ryan Hutchison
This is why America’s healthcare is broken. We give people pills and expect them to be nutritionists, pharmacists, and time managers all at once. Meanwhile, Big Pharma profits while we scramble. The real fix? Single-dose combo pills with built-in food guidelines. Not more apps. Not more labels. Better design.
January 27, 2026 AT 08:04
Riya Katyal
Wait, so if I take my statin with avocado toast, I’m fine? But if I take it with grapefruit, I’m dead? So avocado is the new hero? I’m confused. And also, why do I feel like this is just a fancy way to sell pill organizers?
January 28, 2026 AT 22:13