How to Bring a Caregiver or Advocate to Medication Appointments

- Colin Hurd
- 15 January 2026
- 10 Comments
Getting your medications right isn’t just about picking up a prescription. It’s about making sure the right drug is prescribed at the right dose, that it doesn’t clash with what you’re already taking, and that you actually understand how and when to take it. But in a busy clinic, with a doctor rushing between patients and a patient overwhelmed by names, doses, and side effects, mistakes happen. Medication errors affect 1.5 million Americans every year. Bringing someone with you - a caregiver, family member, or professional advocate - can cut that risk dramatically.
Why You Need Someone With You
Think of your medication appointment like a business meeting where the stakes are your health. You’re not just getting a script. You’re negotiating a treatment plan that could involve five, ten, or more pills a day. You might have memory issues, hearing loss, anxiety, or simply not enough time to ask all the right questions. That’s where an advocate comes in. They’re not there to speak for you. They’re there to help you be heard. A 2023 study in Health Affairs found that patients with advocates had 28% fewer medication errors. That’s not a small number. It’s the difference between feeling okay and ending up in the ER because a new antibiotic canceled out your blood thinner. And it’s not just about catching mistakes. Advocates help you understand what’s being said. They write down instructions. They ask, “Can this pill be crushed?” or “Is there a cheaper version?” They remember the doctor said “once daily,” but you heard “twice a day.” They’re your backup brain.Who Can Be Your Advocate?
You don’t need a medical degree. You just need someone you trust.- Family members - Spouses, adult children, siblings. They know your routines, your habits, your fears. But they need to be prepared.
- Friends or neighbors - Someone reliable who can sit with you, take notes, and call later to double-check.
- Professional advocates - Certified through organizations like the Patient Advocate Certification Board. These are trained professionals who specialize in navigating healthcare systems. They cost $75-$200 an hour, but for complex cases - like managing five or more medications - they reduce errors from 58% to 22%.
How to Prepare - 72 Hours Before the Appointment
This is where most people fail. They show up with a list. But lists are wrong 23% of the time, according to the FDA. Pills get switched. Names get misspelled. Doses change without notice. Here’s what actually works:- Bring the actual bottles. Not a piece of paper. The real pills. That way, the doctor or pharmacist can see the label, the color, the shape. If you’re taking metoprolol 25mg, but the bottle says 50mg, that’s a red flag.
- Make a symptom log. Write down when you felt dizzy, tired, nauseous - and when you took each pill. Did the dizziness start after you took the new blood pressure med? That’s important.
- Check your insurance. Call your pharmacy or insurer 48 hours before. Is your medication covered? Is there a prior authorization needed? If you show up and they say “We can’t fill this,” you’ve wasted a trip.
- Write down your top 3 questions. Use the “Ask Me 3” framework: What is my main problem? What do I need to do? Why is it important? Keep it simple.
What to Do During the Appointment
Your advocate’s job during the visit is to listen, ask, and record.- Use SBAR. It’s a simple communication tool used in hospitals: Situation (I’m here because my mom is having dizziness), Background (She’s on warfarin, metoprolol, and a new antibiotic), Assessment (We think the antibiotic is interacting), Recommendation (Can we switch to something else?). This increases understanding by 52%.
- Ask about alternatives. “Is there a generic?” “Can this be taken once a day?” “Is there a liquid form?”
- Confirm the instructions. Don’t just nod. Say, “So, to be clear - take one tablet with breakfast, and don’t crush it?” Then repeat it back.
- Ask about side effects. “What should I watch for in the first week?” “Which ones mean I need to call you right away?”
What Happens After the Appointment
The work doesn’t end when you walk out the door.- Compare what the doctor said to what the pharmacy says. Sometimes the script says “take one daily,” but the pharmacist says “take one every other day.” That’s a red flag.
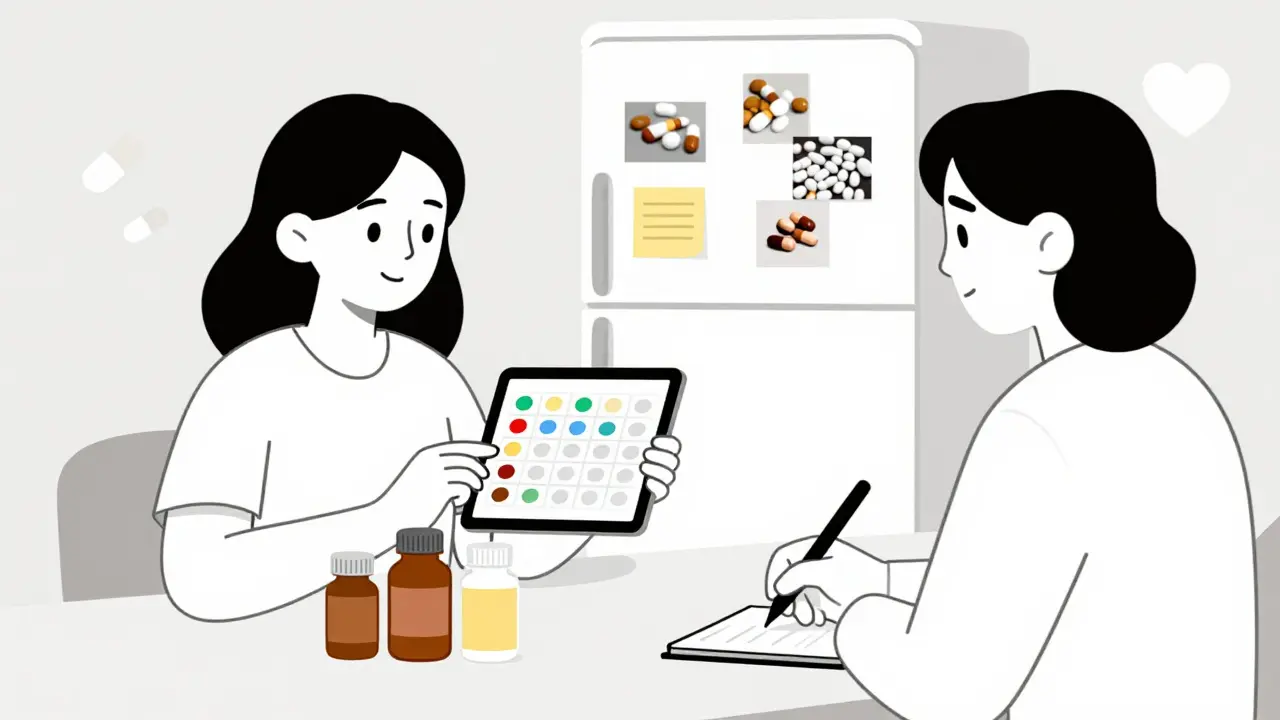
- Create a visual schedule. Take pictures of each pill. Print them out. Tape them to the fridge. Label them with times: “7 a.m. - Blue pill,” “8 p.m. - White pill.” A GoodRx study showed this cuts identification errors by 67%.
- Set up a “medication buddy.” Have someone check your pillbox once a week. A simple “Did you take your blood thinner today?” can prevent a stroke.
- Follow up in 24 hours. If anything was unclear, call the doctor’s office. Say, “I’m reviewing the notes from yesterday and wanted to confirm - was the dose for the new med 5mg or 10mg?”
What If the Doctor Says No?
You have a legal right to bring someone. The American Medical Association’s 2022 policy update says providers must allow advocates during consultations. Yet 31% of older adults report being turned away, often with excuses like, “HIPAA doesn’t allow it.” That’s false. HIPAA doesn’t stop you from bringing someone. It only stops the provider from sharing your info without your permission. All you need to do is sign a simple form - often called a “HIPAA authorization” - giving your advocate permission to be involved. Bring it with you. If you’re denied, ask to speak to the office manager. Say: “I’m exercising my right under AMA policy H-280.955.1 to have an advocate present. Can we get that form filled out now?” Most clinics will comply once you know your rights.
When to Consider a Professional Advocate
You don’t need one for every appointment. But if you’re managing five or more medications, have memory issues, or your family can’t help consistently, it’s worth it. Professional advocates can:- Review your entire medication history across multiple providers
- Find lower-cost alternatives based on your insurance
- Coordinate with pharmacies and home delivery services
- Attend appointments with you and take detailed notes
What’s Changing in 2026
Medication advocacy is no longer a nice-to-have. It’s becoming part of standard care.- Medicare Advantage plans now include advocacy support for 62% of members - up from 38% in 2020.
- Medicare providers must now document advocate involvement in all high-risk cases, or they lose reimbursement.
- AI tools like MediCheck Pro are being used in clinics to flag drug interactions during appointments - and advocates are the ones who help interpret the results.
- Telehealth advocates are rising. By 2026, 68% of medication consultations will include a virtual advocate via video.
Final Thought: It’s Not About Being a Hero - It’s About Being Smart
You don’t have to be perfect. You don’t have to memorize every drug interaction. You just have to show up prepared. Bring the bottles. Ask the questions. Write it down. Bring someone who can help you remember. Medication errors don’t happen because doctors are careless. They happen because the system is overloaded - and patients are expected to navigate it alone. You’re not asking for special treatment. You’re asking for the care you’re entitled to. And you deserve that.Can I bring someone to my medication appointment even if they’re not a family member?
Yes. You can bring a friend, neighbor, or professional advocate. The key is that you give the provider written permission - usually a simple HIPAA authorization form - so they can legally discuss your health information with them. The person doesn’t need to be related to you. They just need to be someone you trust to help you understand and remember what’s said.
What if my doctor says they won’t talk to my advocate because of HIPAA?
That’s incorrect. HIPAA doesn’t prevent providers from talking to your advocate - it only prevents them from sharing your information without your permission. Ask to fill out a HIPAA authorization form. If they refuse, ask to speak with the office manager or patient services director. The American Medical Association’s policy H-280.955.1 requires providers to allow advocates, and 92% of large healthcare systems follow this rule.
Do I need to pay for a professional advocate?
Not always. Professional advocates cost $75-$200 per hour, but many are available for free or low cost through Federally Qualified Health Centers, Area Agencies on Aging, or Medicare Advantage plans. As of 2024, 62% of Medicare Advantage plans include some form of medication advocacy support. Check with your plan or local senior center - you may already have access.
How do I know if my medication list is wrong?
Compare your written list to the actual pill bottles. Look for mismatches in name, dose, frequency, or manufacturer. Also, check your portal or pharmacy records. If you’re taking metoprolol 25mg but your list says 50mg, or if a pill you don’t recognize is listed, that’s a red flag. The FDA found that 23% of medication errors happen because the list doesn’t match reality - never rely on memory or paper alone.
What’s the most important thing to ask at a medication appointment?
Ask: “What is the one thing I need to know about this medication that could save my life?” This forces clarity. It’s better than asking a dozen vague questions. It’s also the question that helped one patient avoid a fatal interaction between warfarin and a new antibiotic - her daughter asked it, and the doctor immediately changed the prescription.



Comments
Haley Graves
Bringing my mom to her last med appointment saved her from a dangerous interaction. She was on warfarin and the doctor added a new antibiotic without checking her full list. My sister had the bottles, the symptom log, and asked the exact question the article mentioned: 'What’s the one thing that could save her life?' The doctor paused, checked the database, and canceled it. No ER trip. No hospital stay. Just a prepared family member who knew how to speak up.
Don’t wait until something goes wrong. Start with the bottles. Write down the symptoms. Bring someone who won’t let you nod along when you’re confused.
January 15, 2026 AT 19:36
Diane Hendriks
The systemic failure of American healthcare is not mitigated by bringing a friend. It is exacerbated by it. The very notion that a layperson must serve as a human backup for a broken medical infrastructure reveals the rot at the core of our system. We have outsourced cognitive labor to untrained civilians because physicians are overworked, underpaid, and demoralized. This is not empowerment. It is institutional abandonment dressed in self-help rhetoric.
And yet, the article’s tone remains dangerously optimistic. No mention of the pharmaceutical lobbying that drives polypharmacy. No critique of the insurance-driven formularies that force patients into dangerous substitutions. No acknowledgment that the real solution is universal healthcare, not a checklist.
This is not advice. It is a Band-Aid on a severed artery.
January 16, 2026 AT 05:37
Sohan Jindal
They want you to bring someone? Sure. But who’s really behind this? The big pharma companies. They know if you bring someone, you’ll start asking about generics. You’ll check the bottles. You’ll find out the real cost. And then you’ll demand lower prices. So they make it seem like a good idea-like it’s your idea. But it’s not. It’s a trap. They want you to think you’re in control while they keep raising prices on the stuff you can’t afford anyway.
And don’t get me started on ‘professional advocates.’ Who funds them? Who trains them? Who’s paying for the certification? It’s all connected. The same people who run the hospitals. The same people who own the pharmacies. They’re just hiring people to make you feel better while they keep taking your money.
Don’t be fooled. This isn’t help. It’s distraction.
January 16, 2026 AT 21:47
Frank Geurts
Allow me to extend my profound appreciation for the meticulous and deeply compassionate structure of this article. It is, without hyperbole, a masterclass in patient advocacy, and its alignment with contemporary healthcare ethics is both timely and indispensable.
One must commend the rigorous citation of empirical data-from the 28% reduction in medication errors to the 67% decrease in identification errors via visual scheduling-as these figures are not merely statistical, but represent tangible, life-preserving outcomes.
Furthermore, the inclusion of the SBAR framework and the ‘Ask Me 3’ methodology reflects an elegant synthesis of clinical communication theory and practical utility. The reference to AMA Policy H-280.955.1 is particularly vital, as it anchors patient rights in institutional policy rather than aspirational goodwill.
I implore all healthcare institutions to adopt this model as mandatory training. And I urge every patient, regardless of age or condition, to treat this not as an option, but as a non-negotiable standard of care.
January 17, 2026 AT 04:41
Annie Choi
My aunt’s neurologist refused to let her brother sit in. Said HIPAA. She cried in the parking lot. I called the clinic director. They had no idea about AMA policy. We filed a complaint. They changed their policy within a week.
Stop letting them gaslight you. You have rights. Bring your person. Bring your bottles. Bring your list. Bring your rage if you need to. This isn’t about being polite. It’s about staying alive.
And if you’re scared to speak up? Do it for the person who can’t. That’s the real advocacy.
January 18, 2026 AT 13:02
Mike Berrange
Everyone’s acting like this is some groundbreaking insight. Newsflash: people have been bringing relatives to doctor appointments since the 1950s. The fact that this needs to be spelled out in a 2000-word article says everything about how broken the system is.
And don’t even get me started on the ‘professional advocate’ hustle. You’re telling me someone’s going to charge $200/hour to read a pill bottle? That’s not advocacy. That’s predatory capitalism with a nice PowerPoint.
Meanwhile, the real problem-the lack of proper training for doctors, the insane caseloads, the profit-driven insurance models-is never addressed. You’re giving patients bandaids while the hospital burns down.
January 20, 2026 AT 09:11
Dan Mack
They’re making this sound like a miracle cure. But what if your advocate is the one causing the mistakes? My cousin brought his girlfriend to his appointment. She ‘helped’ by telling the doctor his meds were ‘making him too calm.’ The doctor cut his antidepressant in half. Two weeks later he tried to jump off a bridge.
Not everyone has a good advocate. Some have enablers. Some have drama queens. Some have people who just want to control the conversation.
And now we’re supposed to trust strangers with our medical info? No thanks. I’ll take my chances with the system.
January 20, 2026 AT 13:42
Amy Vickberg
I’ve been a caregiver for my dad for 8 years. He’s on 11 meds. We use the pill pictures, the fridge chart, the weekly check-in with my sister. We’ve caught 3 errors already. One was a wrong dose on a blood thinner. We almost didn’t notice because the bottle label was faded.
But here’s the thing-it’s not about being perfect. It’s about being present. Even if you forget the symptom log. Even if you don’t know SBAR. Just show up. Ask one question. Write one thing down.
You don’t need to be a hero. You just need to care enough to show up.
And if you’re reading this and thinking ‘I’m not qualified’-you are. You’re already qualified because you care.
January 21, 2026 AT 05:29
Nishant Garg
In India, we call this ‘family support system’-it’s not a strategy, it’s a cultural norm. Elders are never alone in clinics. Someone always comes: daughter, nephew, neighbor. We bring the bottles, we write notes on the back of grocery receipts, we ask the questions the patient is too shy to ask.
But here’s the twist: we don’t call it ‘advocacy.’ We call it love. We don’t need a certification. We don’t need a $200/hour consultant. We just need to show up.
Maybe the real lesson isn’t in the checklist. Maybe it’s in the fact that no one in our culture would dream of sending an elderly person to a doctor’s appointment alone. We don’t treat health like a solo sport. We treat it like a family affair.
What if the answer isn’t more tools-but more presence?
January 22, 2026 AT 05:42
Nicholas Urmaza
Finally someone says it. The system is designed to fail you. They give you a 10-minute window. They hand you a script. They don’t explain. They don’t listen. So you bring someone. Not because it’s nice. Because you have to.
And if you’re still letting them tell you it’s not allowed? You’re playing their game. Sign the form. Say the words. Demand the space. This isn’t a favor. It’s your right.
And if you’re waiting for permission? You’re already losing.
January 24, 2026 AT 01:49