How to Get Clear Medication Instructions When Directions Are Confusing

- Colin Hurd
- 17 January 2026
- 12 Comments
It’s not uncommon to walk away from the pharmacy with a prescription in hand and a sinking feeling: medication instructions don’t make sense. Maybe the label says "take as needed" but doesn’t say how often. Or it uses "q.d." instead of "daily," and you’re not sure if that’s once a day or twice. Maybe the doctor scribbled "BID" and you’re guessing what it means. You’re not alone. Nearly 1 in 4 American adults takes three or more medications daily, and unclear directions are one of the top reasons people make dangerous mistakes.
Why Medication Instructions Get So Confusing
Medication instructions aren’t always written with patients in mind. Many still use outdated abbreviations that were common in medical notes decades ago. "q.d." for daily, "BID" for twice a day, "t.i.d." for three times a day - these are all shorthand that can be misread. The Institute for Safe Medication Practices (ISMP) has been warning for years that these abbreviations cause confusion. Even worse, "d" in a dose like "5 mg/kg/d" can be mistaken for "dose" instead of "day," leading to dangerous overdoses. Some prescriptions mix brand and generic names without clarifying which one you’re getting. Different manufacturers of the same drug - say, metformin or lisinopril - sometimes list slightly different dosing instructions on their packaging. One might say "take with food," another says "take on an empty stomach." That’s not a typo. It’s a real difference, and if you don’t know to check, you might be taking it wrong. The FDA requires Medication Guides for about 200 high-risk drugs - like opioids, isotretinoin, and birth control pills - but for most other prescriptions, there’s no standardized patient handout. That means you’re relying on what the pharmacist says, what the doctor wrote, and what’s printed on the bottle. And if any of those conflict? You’re left guessing.What to Do When Instructions Don’t Make Sense
The first rule is simple: never assume. If something is unclear, ask. Don’t wait until you feel sick or your symptoms don’t improve. Here’s exactly what to do:- Read the label out loud - say it word for word. If you stumble or feel unsure, that’s your cue to stop and ask.
- Check for abbreviations. If you see "q.d.," "BID," "t.i.d.," "QID," or "PRN," write them down and ask what they mean. These should never be used in patient-facing instructions. They should say "daily," "twice a day," "three times a day," or "as needed."
- Ask for the purpose. Don’t just ask how to take it - ask why. "What is this medicine supposed to do?" If it’s for blood pressure, you need to know if it’s meant to be taken in the morning or at night. Cholesterol meds, for example, work best at bedtime because your liver makes more cholesterol overnight.
- Clarify "as needed". This phrase is dangerously vague. Ask: "What’s the maximum number of doses I can take in a day? How long should I wait between doses?" For painkillers, it might be "one every 6 hours, no more than 4 in 24 hours." For anxiety meds, it might be "only if you feel a panic attack coming on, and no more than twice a day."
- Confirm timing. If it says "twice daily," ask: "Should I take it at 8 a.m. and 8 p.m., or can I take it at breakfast and dinner?" Some meds need to be spaced evenly - others don’t. Timing affects how well they work.
When You Should Talk to Your Pharmacist - Not Just Your Doctor
Your pharmacist is trained specifically to catch medication errors. They see hundreds of prescriptions a day and know which ones are commonly misunderstood. If you get a new prescription, ask: "Can you explain how to take this?" They’re required to review the instructions with you, even if you didn’t ask. In community pharmacies, pharmacists must give you a printed FDA-approved Medication Guide if your drug is on the list. If they don’t offer it, ask for it. These guides explain risks, side effects, and exactly how to take the medicine. You can also request a digital copy - many pharmacies now email or text them. If you’re on multiple meds, bring your list to the pharmacy every time you pick up a new one. Pharmacists can spot interactions you might miss. For example, taking a blood thinner with certain painkillers can raise your risk of bleeding. That’s not something your doctor always remembers to mention.
What to Do If Two Pills Look the Same But Have Different Instructions
Let’s say you’ve been taking a generic version of your blood pressure pill for months. You refill it, and this time the instructions say "take in the morning," but last time they said "take at night." That’s not a mistake - it’s a manufacturer difference. The active ingredient is the same, but the inactive fillers or release mechanisms can vary slightly, and some manufacturers test different timing. The National Institutes of Health (NIH) says doctors should compare instructions from different manufacturers when prescribing. But you shouldn’t wait for them to catch it. When you notice a change:- Compare the old and new bottle labels side by side.
- Call your pharmacist and say: "I noticed the instructions changed on this pill. Is this safe?"
- Ask if the new version is bioequivalent - meaning it works the same way in your body.
- If you’re unsure, ask your doctor to write "Dispense as written" on the prescription. That stops the pharmacy from switching brands without approval.
How to Avoid Mistakes at Home
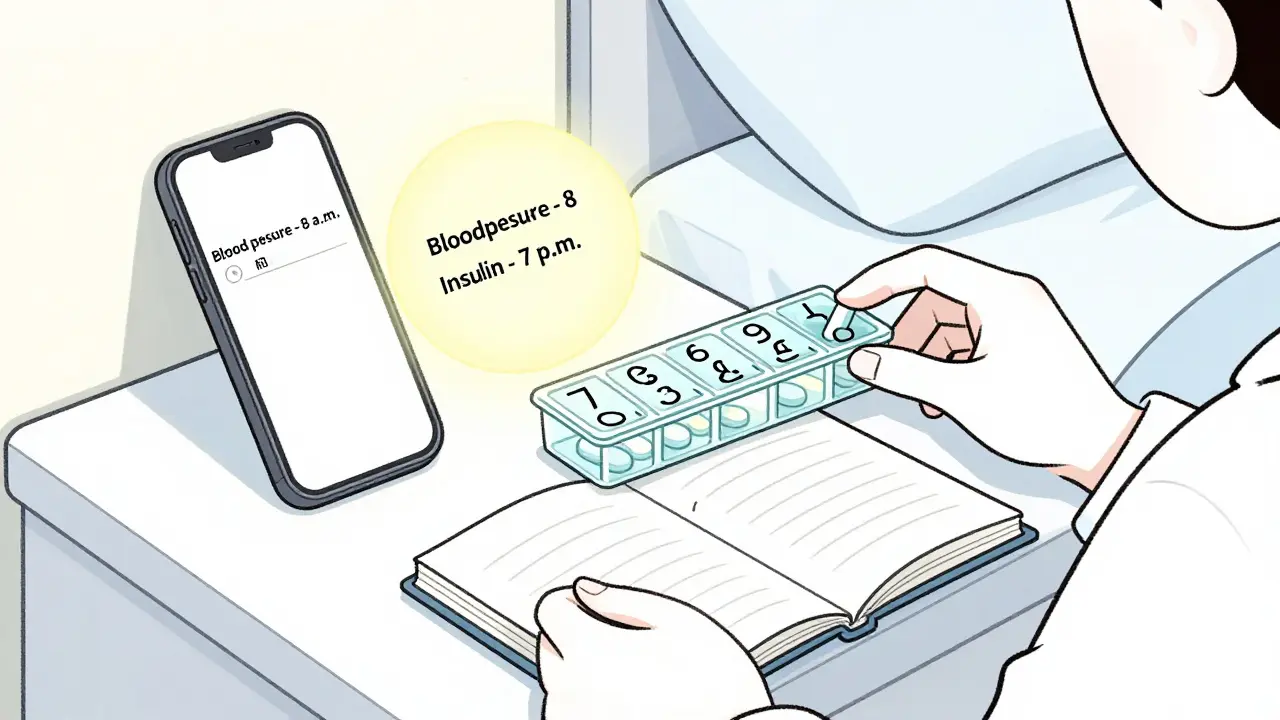
Once you’ve gotten clear instructions, make sure you follow them correctly. Here’s how:- Use a pill organizer. Buy one with compartments for morning, afternoon, evening, and bedtime. Fill it once a week. It’s easier to see if you’ve missed a dose.
- Set phone alarms. Label them clearly: "Blood pressure - 8 a.m." or "Insulin - 7 p.m."
- Keep a written log. Write down what you took and when. If you feel off, you’ll have a record to show your doctor.
- Don’t mix meds with alcohol. Even if the label doesn’t say so, many drugs interact with alcohol in ways that aren’t obvious - like causing dizziness or liver damage.
- Check expiration dates. Old meds can lose potency or become unsafe. If it’s been more than a year since you filled it, ask if you need a new prescription.
What to Do If You Already Took It Wrong
If you realize you took your medicine at the wrong time, doubled up, or skipped a dose - don’t panic. But don’t ignore it either.- For most routine meds (like blood pressure or cholesterol pills), just go back to your normal schedule. Don’t double the next dose.
- For insulin, blood thinners, or seizure meds, call your doctor or pharmacist immediately. These can be dangerous if dosed incorrectly.
- For pain meds, if you took more than the daily limit, watch for nausea, drowsiness, or confusion. Call poison control at 1-800-222-1222 if you’re worried.
When to Seek Help Right Away
Some mistakes can lead to serious harm. Call your doctor or go to urgent care if you:- Took a double dose of a blood thinner or diabetes medication
- Missed multiple doses of an antibiotic and now feel worse
- Started a new med and developed a rash, swelling, or trouble breathing
- Are confused, dizzy, or fainting after taking your medicine
What’s Changing in Medication Safety
The system is slowly improving. The FDA is pushing for electronic Medication Guides that patients can access through apps or portals. Some pharmacies now include QR codes on labels that link to video instructions in plain language. The NIH is working on a database that compares instructions across all manufacturers of the same drug - so doctors can pick the clearest version. But until those systems are universal, you’re still your own best safety net. No one cares more about your health than you do. If the instructions don’t make sense, you have every right to ask until they do.What should I do if my medication label uses "q.d." or "BID"?
Always ask your pharmacist or doctor to rewrite the instructions in plain language. "q.d." means "daily," and "BID" means "twice a day." These abbreviations are outdated and can be misread. You should never see them on a patient label - if you do, request a corrected version.
Can I switch between generic brands of the same drug?
Yes, but only if your doctor approves it. Different manufacturers can have slightly different instructions - like timing or whether to take with food. If you notice a change in how you feel after switching brands, tell your doctor. Ask them to write "Dispense as written" on your prescription to avoid automatic substitutions.
What does "take as needed" really mean?
It doesn’t mean "whenever you feel like it." You need to know the maximum number of doses allowed in a day and how far apart they should be. For example, "take one tablet as needed for pain, no more than 4 in 24 hours, at least 6 hours between doses." If your prescription doesn’t include those details, ask your pharmacist to clarify.
Why do some medications need to be taken at bedtime?
Some drugs work better at night because your body’s natural rhythms affect how they’re processed. Cholesterol-lowering statins, for example, are most effective when taken at bedtime because your liver produces more cholesterol overnight. Blood pressure meds may be timed to lower pressure during the early morning, when heart attacks are most common. Always ask why timing matters.
Should I keep a list of all my medications?
Yes - and update it every time you get a new prescription or stop one. Include the name, dose, purpose, and instructions. Bring it to every doctor’s visit and pharmacy trip. It helps prevent dangerous interactions and makes it easier to spot confusing instructions.



Comments
Emma #########
I used to panic every time I got a new script until I started asking pharmacists to explain everything in plain English. Turns out they’re way more patient than doctors and actually want you to understand it. Now I always say, 'Can you spell it out like I’m five?' and they do. No judgment, just help.
It’s crazy how much stress this one question removes.
January 19, 2026 AT 00:07
Andrew Qu
For anyone still seeing 'q.d.' or 'BID' on a label-that’s a red flag. Those abbreviations are banned in patient-facing materials by the ISMP. If your pharmacy is still using them, ask for a corrected label or go elsewhere. Most pharmacies now use electronic systems that auto-translate those into plain language. If yours doesn’t, they’re lagging behind by a decade.
Also, if you’re on more than three meds, get a free med sync service. They’ll bundle your refills and give you a printed schedule. It’s lifesaving for people with memory issues or chronic conditions.
And yes, pill organizers work. I used to forget half my pills. Now I take a photo of my organizer every Sunday. If I don’t see it in my gallery, I didn’t take it.
January 19, 2026 AT 08:03
Praseetha Pn
They don’t want you to understand your meds because if you did, you’d realize how many of them are just profit machines. The whole system is rigged-brand names, generic switches, timing changes-it’s all designed to keep you confused so you don’t question why you’re on five pills for high blood pressure when one could do it. The FDA? They’re paid off by Big Pharma. The QR codes? Just a distraction. The real solution is to stop taking everything they give you and go holistic. I cured my cholesterol with turmeric and fasting. No pills. No nonsense.
They’ll never tell you that.
And don’t get me started on how they make you take statins at night because your liver ‘makes more cholesterol’-that’s a myth cooked up by a lab in 1987 and never updated. Your liver doesn’t care what time it is. It’s all about inflammation. You’re being manipulated.
January 19, 2026 AT 12:08
Andrew Short
People who don’t read the label properly are the reason ERs are full of overdoses. If you can’t tell the difference between 'BID' and 'TID', maybe you shouldn’t be managing your own meds. I’ve seen grandmas mix up insulin and metformin because they ‘assumed.’ Assumption kills. You want to live? Read. Write. Ask. Repeat.
And if you think your pharmacist is ‘required’ to explain it, you’re delusional. They’re overworked and underpaid. Don’t expect hand-holding. Take responsibility.
Also, ‘as needed’ doesn’t mean ‘whenever I feel like it.’ That’s not a question. That’s a warning. If you need to be told that, you’re not ready for prescription meds.
January 20, 2026 AT 19:00
Nishant Sonuley
Look, I’ve been on seven different meds for my autoimmune thing, and I’ve learned one thing: if you don’t write it down, it doesn’t exist. I keep a little notebook in my wallet-name, dose, time, why, side effects I noticed. I even color-code: red for ‘call if you feel weird,’ green for ‘just keep taking.’
And yeah, I’ve had the same generic blood pressure pill from two different manufacturers-same active ingredient, one said ‘take at night,’ the other said ‘take with breakfast.’ I called my pharmacist, she laughed and said, ‘Yeah, that’s common. The new one’s enteric-coated, so food slows absorption. Take it in the morning now.’
Turns out, the ‘why’ matters more than the ‘what.’ I asked my doc why it changed, and he said, ‘Because your liver enzymes are trending up, and we want to reduce overnight stress.’ I didn’t know that was even a thing. So now I ask ‘why’ every time. It’s saved me from two bad interactions already.
Also, don’t trust the bottle. Trust the Medication Guide. If they don’t hand it to you, ask for it. I keep mine in a folder. I’ve got 17 of them. It’s my health Bible.
And if you think ‘as needed’ means ‘whenever I feel like it,’ you’re one missed dose away from an ER trip. I had a buddy take his anxiety med ‘as needed’-and took six in one night because he was ‘stressed.’ He ended up in the hospital. Don’t be that guy.
Pharmacists aren’t just pill dispensers. They’re your last line of defense. Treat them like the experts they are. Ask questions. Be polite. Be persistent. Your life depends on it.
And yes, I’ve seen people try to take antibiotics with grapefruit juice. That’s not a joke. It’s a death sentence. Please stop.
January 22, 2026 AT 13:31
Chuck Dickson
You got this. Seriously. Asking questions isn’t being difficult-it’s being smart. I used to feel dumb asking about my meds until I realized: if I don’t understand it, I’m not the problem. The system is.
Now I walk into the pharmacy like I own the place. ‘Hey, can you walk me through this?’ And they do. Sometimes they’re surprised-but always grateful.
And if you’re on multiple meds? Get a free med review. Many pharmacies offer it. They’ll sit with you for 20 minutes and tell you what each pill does, what to watch for, and if anything clashes.
Don’t wait until you feel bad. Do it now. You’re worth the effort.
Also-pill organizer + phone alarms = life changed. I set mine to play a silly sound. ‘It’s time for your happy blood pressure pill!’ It makes me laugh. And I never miss one.
You’re not alone. We’re all figuring this out. Keep asking. Keep learning. You’re doing great.
January 23, 2026 AT 08:26
Naomi Keyes
It is, however, critically important to note that the use of Latin abbreviations such as 'q.d.', 'BID', 't.i.d.', and 'QID' is not merely outdated-it is, by current FDA guidelines and ISMP recommendations, categorically prohibited in direct patient-facing labeling. The fact that these still appear on some prescriptions is not a clerical oversight; it is a systemic failure of pharmacy management systems, compounded by inadequate staff training and a lack of enforcement mechanisms.
Furthermore, the assertion that ‘different manufacturers of the same drug sometimes list slightly different dosing instructions’ is not merely a ‘difference’-it is a potentially lethal inconsistency in bioequivalence documentation, which should be flagged by the prescriber prior to dispensing. The National Institutes of Health does not, in fact, maintain a public database comparing manufacturer instructions-this is a common misconception.
And while ‘Dispense as Written’ is a legitimate directive, it must be handwritten on the prescription by the prescriber-not electronically pre-checked by a computer system, which often defaults to ‘Dispense as Generic’ regardless of intent.
Moreover, the notion that ‘you’re your own best safety net’ is not only true, but legally and ethically imperative. Patients who do not actively engage in their medication reconciliation are, by default, relinquishing their right to safe care.
Finally, the use of ‘as needed’ without quantification is not ‘vague’-it is negligent. Every ‘as needed’ prescription must include: maximum daily dose, minimum interval between doses, and indication for use. If it does not, the prescription is incomplete-and legally unenforceable.
January 24, 2026 AT 00:26
christian Espinola
q.d. means daily. BID means twice a day. TID means three times. QID means four. If you don’t know this, you shouldn’t be taking prescription meds. You’re a liability.
And ‘as needed’? That’s not a suggestion. It’s a warning label. If you’re asking what it means, you’re the reason people die from accidental overdoses.
Also, pill organizers? Cute. But if you’re relying on a plastic box to remember your meds, you’ve already lost. Your brain is broken. Get help.
And don’t even get me started on the ‘pharmacist will explain it’ myth. They’re running on caffeine and 200 scripts an hour. They don’t have time for your confusion. You think they care? They care about the next person in line.
Stop blaming the system. Start being responsible. Or stop taking pills. Either way, don’t be the reason someone else gets hurt.
January 25, 2026 AT 16:00
Jay Clarke
Let me tell you about the time I took my blood pressure med at 3 a.m. because I thought ‘twice daily’ meant ‘when you wake up and when you go to bed’-but my body said ‘NOPE’ and I woke up feeling like I’d been hit by a truck.
Turns out, it’s not about sleep. It’s about circadian rhythms. And I didn’t know that because no one told me.
Now I have a whole spreadsheet. Color-coded. With emojis. 🌞💊🌙
And I call my pharmacist every time I get a refill. I even text them a picture of the label. They think I’m weird. I think they’re underpaid angels.
Also, I once switched generics and started having panic attacks. Turns out, the new one had a different filler. My body hates cornstarch. Who knew?
So yeah. Ask questions. Take notes. Don’t trust the bottle. The system is broken. But you? You’re the glitch in the matrix that fixes it.
Also, I’m not crazy. I just care too much.
And if you’re still using ‘q.d.’? You’re literally living in 1998. Time travel is real. You’re just not doing it right.
January 26, 2026 AT 09:05
Robert Cassidy
America’s healthcare system is a joke. We pay more than any country on Earth, and we still can’t get a label that says ‘take once a day’ instead of ‘q.d.’? This isn’t medicine. It’s corporate theater.
They want you confused. Confused people don’t ask questions. Confused people don’t fight back. Confused people just keep taking the pills.
And don’t even get me started on the ‘generic switch’ scam. Same drug, different manufacturer, different instructions-just to make you doubt yourself. That’s not science. That’s control.
They don’t want you to know your body. They want you dependent.
So yeah. Keep your notebook. Keep your alarms. Keep your questions. Because if you stop asking, you’re already dead.
And if you think this is normal? You’re not awake yet.
January 26, 2026 AT 11:01
kenneth pillet
Just ask. Seriously. I used to be too shy. Now I just say, 'Can you say that again like I'm dumb?' And they do. No big deal.
Also, pill organizer. Best thing ever.
And if the label says 'q.d.'? Call them. They messed up.
January 27, 2026 AT 05:08
Andrew Short
That’s exactly what I said. If you’re asking, you’re already behind. The system doesn’t care if you’re confused. It just wants you to keep taking the pills.
And don’t even get me started on the ‘pharmacist will help’ myth. They’re drowning. You’re not their priority.
Stop waiting for someone to save you. Save yourself. Or don’t take the meds. Either way, stop being passive.
January 27, 2026 AT 11:28