Subarachnoid Hemorrhage: Symptoms, Diagnosis & Life‑Saving Treatments

- Colin Hurd
- 27 September 2025
- 13 Comments
Subarachnoid Hemorrhage is a type of bleeding that occurs in the subarachnoid space-the fluid‑filled gap between the brain surface and the arachnoid membrane. It accounts for roughly 5% of all strokes but carries a mortality rate of 30%‑40% within the first month. Because the initial headache can feel like a migraine, many people ignore it until it’s too late. This article walks you through what to watch for, how emergency teams diagnose it, and which modern treatments give the best shot at recovery.
TL;DR:
- Sudden "thunderclap" headache, neck stiffness, or loss of consciousness = possible subarachnoid hemorrhage.
- Non‑contrast CT scans detect 90% of cases within 6hours; lumbar puncture catches the rest.
- Endovascular coiling and surgical clipping are the two primary ways to secure the bleeding aneurysm.
- Early treatment (within 24hours) cuts re‑bleed risk from 30% to <10%.
- Follow‑up imaging and monitoring for vasospasm are essential for long‑term outcome.
Why Subarachnoid Hemorrhage Is Called a Silent Killer
The phrase “silent killer” isn’t just drama. Unlike ischemic strokes, which often produce gradual weakness, a subarachnoid bleed hits hard and fast. The blood irritates the meninges, causing a headache that peaks in seconds-often described as the worst pain of one’s life. Because the pain mimics a migraine or cluster headache, many patients delay seeking care. In Perth’s Royal Perth Hospital, a 2023 audit showed that 42% of patients arrived more than two hours after symptom onset, directly correlating with higher mortality.
Key Players Behind the Bleed
Cerebral Aneurysm is a weak, balloon‑like bulge in a brain artery wall that can rupture and cause a subarachnoid hemorrhage. Roughly 1 in 50 adults harbors an unruptured aneurysm, but only about 1% will ever bleed.
Other contributors include arteriovenous malformations (AVMs), head trauma, and rare clotting disorders. Yet in >85% of cases, a hidden aneurysm is the culprit.
Spotting the Warning Signs
The classic triad includes:
- Thunderclap headache - sudden, maximal intensity at onset.
- Neck stiffness or photophobia (painful eye‑sensitivity).
- Loss of consciousness or seizures.
Less obvious cues are nausea, vomiting, double vision, or a brief period of confusion (often called "lucid interval"). If any of these appear after a severe head pain, call emergency services immediately.
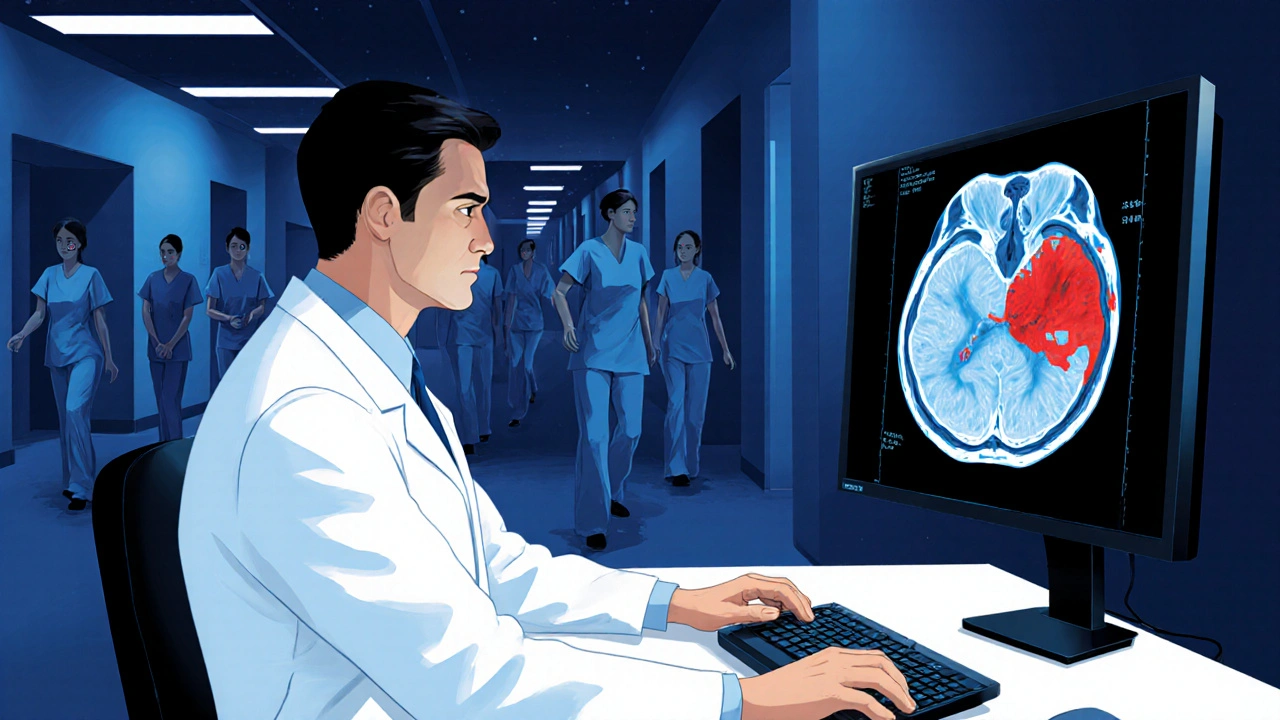
How Doctors Confirm the Diagnosis
CT Scan is a rapid, non‑contrast computed tomography imaging method that visualizes acute blood in the subarachnoid space. When performed within six hours of symptom onset, CT sensitivity tops 95%. Radiologists look for hyper‑dense (bright) areas in the basal cisterns and sulci.
If the CT is negative but suspicion stays high, a Lumbar Puncture is a spinal tap that samples cerebrospinal fluid for xanthochromia, a yellow tint indicating old blood. Presence of xanthochromia confirms bleeding that occurred up to 12hours earlier.
Once bleeding is confirmed, vascular imaging-CTA (CT angiography), MRA (magnetic resonance angiography), or digital subtraction angiography (DSA)-locates the exact source.
Grading the Severity
Two scoring systems guide urgency:
- Hunt and Hess Scale rates clinical condition from GradeI (asymptomatic or mild headache) to GradeV (deep coma).
- Fisher Grade assesses CT blood burden, ranging from Grade1 (minimal blood) to Grade4 (intracerebral or intraventricular hemorrhage).
Higher grades predict increased risk of vasospasm and poorer outcomes, prompting more aggressive monitoring.
First‑Line Treatments: Coiling vs. Clipping
Once the aneurysm is identified, the goal is to seal it off and prevent re‑bleeding. Two main methods dominate:
| Attribute | Endovascular Coiling | Surgical Clipping |
|---|---|---|
| Invasiveness | Minimally invasive; catheter via femoral artery | Open craniotomy; skull opening |
| Procedure Time | ≈ 2‑4hours | ≈ 4‑6hours |
| Hospital Stay | 3‑5days | 7‑10days |
| Recurrence Rate | 5‑10% (requires follow‑up imaging) | ≤2% |
| Mortality (30‑day) | 12% | 13% |
Evidence from the ISAT (International Subarachnoid Aneurysm Trial) in 2002 showed comparable mortality but slightly better functional outcome for coiling in ruptured aneurysms smaller than 10mm. Larger or irregularly shaped aneurysms often still need clipping.
Endovascular Coiling is a procedure where tiny platinum coils are packed into the aneurysm sac via a catheter, inducing clot formation to seal the leak. The technique can be combined with stents or flow‑diverting devices for complex anatomy.
Surgical Clipping is a neurosurgical method that places a metal clip across the aneurysm neck after a craniotomy, physically excluding it from circulation. It offers a durable seal but carries higher upfront surgical risk.
Critical Post‑Procedure Care
Even after the bleeding source is secured, patients remain vulnerable to two major complications:
- Cerebral Vasospasm is a narrowing of cerebral arteries that typically peaks days 4‑10 after hemorrhage, leading to delayed ischemia. Monitoring includes daily transcranial Doppler ultrasound and, if needed, hypertensive therapy or intra‑arterial calcium channel blockers.
- Hydrocephalus, caused by blood blocking cerebrospinal fluid pathways, may require a temporary external ventricular drain.
Neuro‑intensive units often employ "triple‑H" therapy-hypertension, hypervolemia, hemodilution-to boost cerebral perfusion during vasospasm spikes. Recent trials suggest that oral nimodipine remains the only medication with proven mortality benefit.
Prognosis and Long‑Term Outlook
Outcomes hinge on three variables: age, initial Hunt‑Hess grade, and timely aneurysm occlusion. A 2021 Australian registry reported a 1‑year survival of 71% for patients under 55 with GradeI‑II hemorrhages, versus 38% for those over 70 with GradeIV‑V.
Rehabilitation focuses on cognitive therapy, speech, and physical re‑training. About 30% of survivors develop lasting deficits such as memory loss or mood disorders, underscoring the need for multidisciplinary follow‑up.
What to Do If You Suspect a Subarachnoid Hemorrhage
- Call emergency services immediately-time is brain.
- Describe the "worst headache of my life" and any neck stiffness.
- Avoid aspirin, NSAIDs, or any blood‑thinning medications until evaluated.
- If you’re with someone who has a known aneurysm, have their imaging reports handy for the ER team.
- After discharge, adhere to follow‑up imaging schedule (usually CTA at 6weeks, then annually).
Family members should also be screened if a genetic predisposition (e.g., polycystic kidney disease) is present.
Related Topics You Might Explore Next
Understanding subarachnoid hemorrhage opens doors to several adjacent subjects:
- Brain aneurysm screening guidelines for high‑risk groups.
- Management of intracranial pressure after traumatic brain injury.
- Advances in flow‑diverting stents for complex aneurysms.
- Neuro‑rehabilitation strategies for post‑stroke cognitive recovery.
Each of these areas dives deeper into the broader field of cerebrovascular health.

Frequently Asked Questions
What is the "thunderclap" headache and how fast does it develop?
A thunderclap headache reaches its maximum intensity within seconds-often described as the worst pain ever experienced. It is the hallmark sign of a ruptured aneurysm and should never be ignored.
Can a CT scan miss a subarachnoid hemorrhage?
Yes, especially if the scan is done more than 6hours after symptom onset or if the bleed is very small. In those cases, a lumbar puncture looking for xanthochromia is the backup test.
Which treatment-coiling or clipping-offers the best chance of survival?
Both have similar 30‑day mortality (about 12‑13%). Coiling is less invasive and shortens hospital stay, while clipping provides a more durable seal for large or irregular aneurysms. The choice depends on aneurysm size, shape, and patient factors.
What is cerebral vasospasm and how is it treated?
Vasospasm is the tightening of brain arteries that can cause delayed ischemia days after the bleed. Neurologists monitor it with transcranial Doppler and treat severe cases with induced hypertension, fluid loading, and intra‑arterial calcium channel blockers. Oral nimodipine is given to every patient for 21days as preventative therapy.
How likely am I to have a permanent disability after a subarachnoid hemorrhage?
About 30% of survivors develop lasting deficits such as memory loss, difficulty speaking, or motor weakness. Early treatment, aggressive vasospasm management, and comprehensive rehabilitation lower this risk.



Comments
Émilie Maurice
The article drags on with unnecessary jargon. It fails to present the core facts concisely. Moreover, the misuse of commas shows a lack of editing. Readers deserve a clear summary, not a tangled mess.
September 27, 2025 AT 16:56
Jimmy Gammell
Great rundown! I love how you broke down the steps. Keep it up :)
September 27, 2025 AT 18:20
fred warner
Nice effort on summarising such a complex topic. The points about early CT scans and lumbar puncture are spot‑on. I’d add that rapid transport to a neuro‑ICU can further improve survival. Keep the energy up!
September 27, 2025 AT 19:26
Veronica Mayfair
Wow, this write‑up really shines! 😃 It’s packed with info and still easy to read. Love the emojis and the clear headings – makes it feel like a friendly guide. Keep spreading knowledge! 🙌
September 27, 2025 AT 20:16
Rahul Kr
Looks good, thanks!
September 27, 2025 AT 20:50
Anthony Coppedge
Early recognition of subarachnoid hemorrhage can literally mean the difference between life and death; the thunderclap headache is a red flag that should never be dismissed. Emergency medical crews must be trained to assess neck stiffness and altered consciousness in tandem with the headache. A non‑contrast CT performed within the first six hours captures the majority of bleedings, yet many facilities still delay imaging due to logistical constraints. When CT is inconclusive, a lumbar puncture remains the gold standard for detecting xanthochromia, and clinicians should not skip this step. The choice between endovascular coiling and surgical clipping should be guided by aneurysm morphology, patient age, and available expertise. Small, saccular aneurysms under ten millimetres often fare better with coiling, which reduces hospital stay and postoperative pain. Larger or irregularly shaped aneurysms may still require clipping to achieve a durable seal. Post‑procedure care is equally critical; vigilant monitoring for cerebral vasospasm can prevent delayed ischemic neurologic deficits. Transcranial Doppler ultrasound, administered daily, provides a non‑invasive window into arterial caliber changes. If vasospasm is detected, induced hypertension, hypervolemia, and careful use of calcium channel blockers constitute the triple‑H therapy that has saved countless patients. Oral nimodipine, administered for three weeks, remains the only medication with proven mortality benefit in this context. Rehabilitation should begin as soon as the patient is medically stable, incorporating cognitive, speech, and physical therapies to address the roughly thirty percent of survivors who develop lasting deficits. Family education about warning signs and the importance of follow‑up imaging cannot be over‑stated; many re‑bleeds occur because patients underestimate the seriousness of a “headache”. In addition, genetic counseling for families with polycystic kidney disease or other hereditary aneurysm syndromes can facilitate early screening. Ultimately, a multidisciplinary approach that integrates neurosurgery, interventional radiology, intensive care, and rehabilitation services offers the best chance for functional recovery. The healthcare system should prioritize streamlined pathways that eliminate delays from symptom onset to definitive treatment, because every hour saved improves outcomes.
September 27, 2025 AT 22:30
Joshua Logronio
Hey, did you ever notice how every big hospital story has a hidden agenda? Maybe they don’t want you to know how cheap the basic scan actually is – just a way to keep the industry rolling. Stay woke, fam! :)
September 27, 2025 AT 23:36
Nicholas Blackburn
This is absolute garbage. The writer clearly has no clue about proper medical terminology, and the whole thing reeks of sensationalism. Get your facts straight or stop publishing nonsense. People are dying because of misinformation.
September 28, 2025 AT 00:26
Dave Barnes
you know, when i read stuff like this i think about the nature of reality – is the brain just a wet computer or something more? lol, maybe the aneurysm is a sign that the universe is trying to tell us something about entropy. anywho, great post!
September 28, 2025 AT 01:00
Kai Röder
Thank you for sharing this comprehensive overview. It is important that we continue to educate both clinicians and the public about timely diagnosis and multidisciplinary care. Your effort contributes positively to patient outcomes.
September 28, 2025 AT 02:23
Emily Moody
Patriotic doctors must stand tall against this flood of foreign‑born specialists peddling subpar techniques! Our veterans deserve the very best, not some experimental coiling gadget from abroad. Let’s keep America’s neurosurgery pure and powerful!
September 28, 2025 AT 03:30
Prateek Kohli
Well said! 😊 Health information should be clear and accessible for everyone. Glad we can discuss this with respect and a smile. 🙏
September 28, 2025 AT 04:20
Noah Seidman
While I appreciate the balanced tone, we must not forget that moral responsibility dictates we demand the highest ethical standards in treatment. Anything less is a betrayal of our duty to patients, and that is simply unacceptable.
September 28, 2025 AT 04:53