Generic Drug Approval: How Safe, Cheap Medicines Get the Green Light
When you see a generic drug approval, the official process that lets manufacturers sell chemically identical versions of brand-name drugs after patents expire. Also known as ANDA approval, it’s the backbone of affordable medicine in the U.S. and beyond. This isn’t just paperwork—it’s a system designed to save patients billions without cutting corners on safety.
The Hatch-Waxman Act, a 1984 law that balanced innovation with access by creating a fast-track path for generics changed everything. Before this, companies had to repeat full clinical trials just to prove a generic pill worked. Now, they only need to show their version delivers the same active ingredient at the same rate and strength. That’s why a 30-day supply of generic lisinopril costs $4 instead of $150. The FDA, the U.S. agency that enforces strict standards for drug quality, safety, and effectiveness doesn’t approve generics lightly. They inspect manufacturing plants, review bioequivalence data, and even check packaging to make sure nothing’s been swapped out.
What gets tested? The active ingredient, how fast it dissolves, how well your body absorbs it, and whether it causes the same side effects. But here’s the catch: generics don’t need to repeat animal or human trials for safety. Why? Because the original brand already proved that. The FDA treats generics like twins—same DNA, different label. And that’s exactly why over 90% of prescriptions in the U.S. are filled with generics today. You’re not getting a lesser drug—you’re getting the same drug, without the marketing bill.
Some people worry about quality because generics come from overseas factories. But the FDA inspects those same facilities—sometimes more often than brand-name sites. A 2022 FDA report found that over 50% of generic drug plants were located outside the U.S., and nearly all passed inspection. If a batch fails, it’s pulled. No exceptions.
And it’s not just about cost. drug safety, the ongoing monitoring of how medications perform in real-world use after approval applies equally to generics. If a generic version starts causing unexpected reactions, the FDA investigates just like it would with the brand. That’s why you’ll see posts here about how blockchain is now being used to track generic pills from factory to pharmacy, and why bringing your actual pill bottles to doctor visits matters more than ever.
What you’ll find below are real stories and clear breakdowns of how this system works—from the science behind bioequivalence to the legal loopholes that keep prices low. You’ll learn why some generics work better than others (yes, that happens), how patent tricks delay cheaper options, and what to do if your insurance won’t cover the generic you need. This isn’t theory. It’s what happens behind the counter every day, and you deserve to know how it all fits together.
- Colin Hurd
- Dec, 14 2025
- 9 Comments
How the FDA Ensures Generic Drug Quality During Manufacturing
The FDA ensures generic drug quality through strict cGMP standards, unannounced inspections, and rigorous testing of every manufacturing step-not just the final product. This system keeps 90% of U.S. prescriptions safe and effective.
- Colin Hurd
- Nov, 18 2025
- 12 Comments
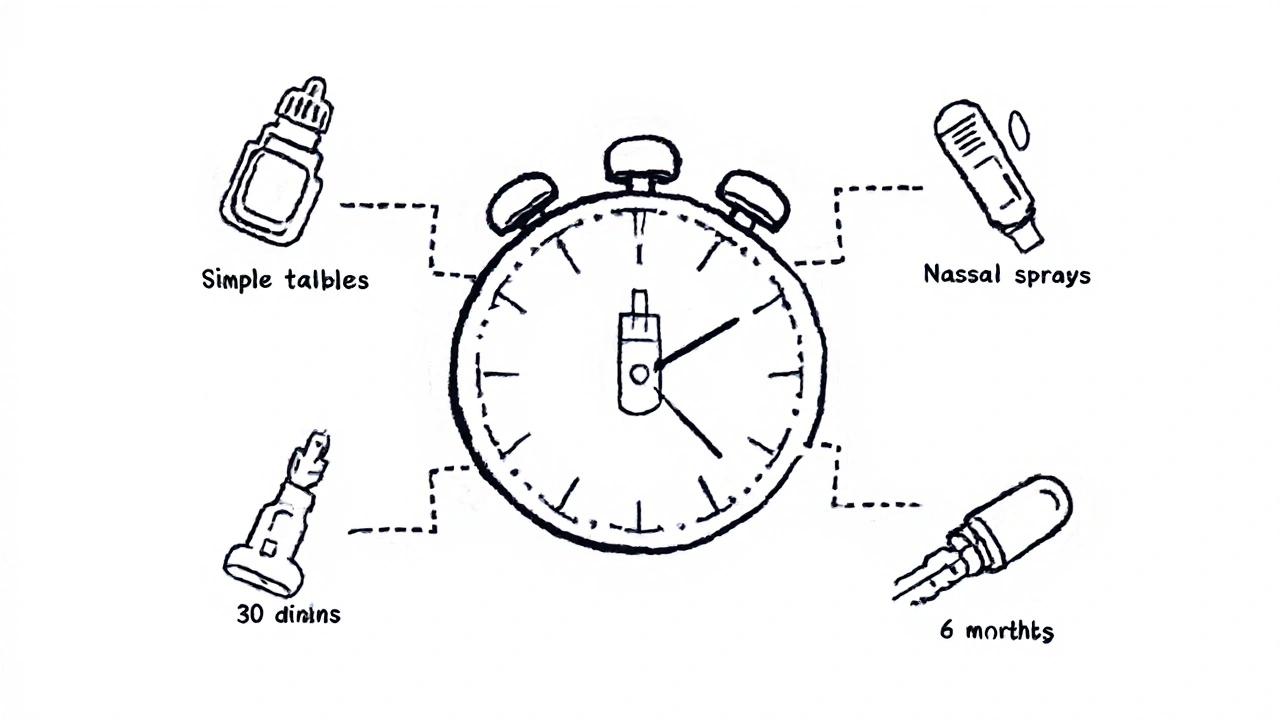
How Long Does the FDA Take to Approve Generic Drugs? 2025 Timelines Explained
Learn how long the FDA takes to approve generic drugs in 2025, from standard 10-month timelines to fast-tracked approvals for complex and shortage drugs. See real data, trends, and what's changing.