Why Prescription Drug Prices Are So High in the United States
- Colin Hurd
- 20 January 2026
- 16 Comments
Why do Americans pay three times more for the same pills than people in Canada, Germany, or the UK? It’s not because our drugs are better. It’s not because they’re made here. It’s because the system is built to let drug companies charge whatever they want - and no one has the power to stop them.
The System Was Designed This Way
In 2003, Congress passed the Medicare Modernization Act. It created Medicare Part D, the prescription drug benefit for seniors. But there was a catch: the law forbade Medicare from negotiating drug prices directly with manufacturers. That made the U.S. the only developed country in the world where the government can’t bargain for lower drug costs. Other nations - like the UK, France, and Australia - use their buying power to set fair prices. The U.S. doesn’t. Instead, it lets drugmakers set list prices, then lets middlemen negotiate discounts behind closed doors.That’s not an accident. It was a deliberate choice. The pharmaceutical industry spent over $300 million lobbying Congress that year. Their argument? If the government negotiates prices, innovation will slow. But the data tells a different story. The U.S. accounts for less than 5% of the world’s population - yet generates 75% of global pharmaceutical profits. That means Americans are subsidizing drug research for the rest of the world.
Who’s Really in Charge? The Hidden Players
You might think your pharmacy, your insurer, or your doctor sets your drug price. But the real power lies with Pharmacy Benefit Managers - or PBMs. These are giant corporations like CVS Caremark, Express Scripts, and OptumRx. Originally, they were supposed to be middlemen who negotiated discounts for insurers. Now, they own pharmacies, insurance plans, and even drug manufacturers. Their business model? Maximize rebates, not lower prices.Here’s how it works: A drug company sets a list price of $1,000. The PBM demands a 40% rebate - so the company pays $400 back. But the list price stays at $1,000. That means your copay - often based on the list price - is still $100 or $200. Meanwhile, the PBM keeps part of that rebate. The patient pays more. The insurer pays more. The drugmaker still makes a profit. And no one sees the full picture.
This isn’t just theory. A 2025 analysis by Morgan Lewis showed that PBMs profit more when list prices go up. That’s why drugs like insulin, Ozempic, and Galzin keep rising in price - even when production costs don’t change.
The Galzin Example: A $88,800 Pill
One drug that shows the absurdity of this system is Galzin - a treatment for Wilson’s disease, a rare genetic disorder. In the U.S., it costs $88,800 a year. In the United Kingdom? $1,400. In Germany? $2,800. That’s not a difference in quality. It’s the same pill, made in the same factory, shipped in the same box. But in the U.S., there’s no price control. No negotiation. No limit.Patients on Galzin often ration their doses. Some skip days. Some sell their pills. Others go without. This isn’t rare. According to Senator Bernie Sanders’ 2025 report, 688 prescription drugs increased in price since 2017 - even as politicians promised to fix it. The White House claims progress. But the numbers don’t lie. In 2024, net drug prices rose 11.4% - up from 4.9% the year before. The biggest drivers? New obesity and diabetes drugs. Drugs like Wegovy and Ozempic. Drugs that cost $1,350 a month in the U.S., but $350 in other countries after recent deals.

The Inflation Reduction Act: A Start - But Not Enough
In 2022, Congress passed the Inflation Reduction Act. It was the first real attempt to bring down drug prices. Starting in 2026, Medicare can negotiate prices for 10 high-cost drugs. By 2029, that number will rise to 20. So far, it’s working. HHS announced in January 2025 that 64 drugs had lower prices because manufacturers had to pay rebates when they raised prices faster than inflation.But here’s the catch: Only 10 drugs are covered in 2026. That’s less than 0.1% of all prescription drugs on the market. And the 2025 budget reconciliation bill weakened the program, adding loopholes that could increase Medicare spending by $5 billion. Meanwhile, drugmakers are already preparing for the next round of price hikes. They’re pushing new drugs into the market - ones that cost $100,000 a year and aren’t yet eligible for negotiation.
Why Don’t Other Countries Have This Problem?
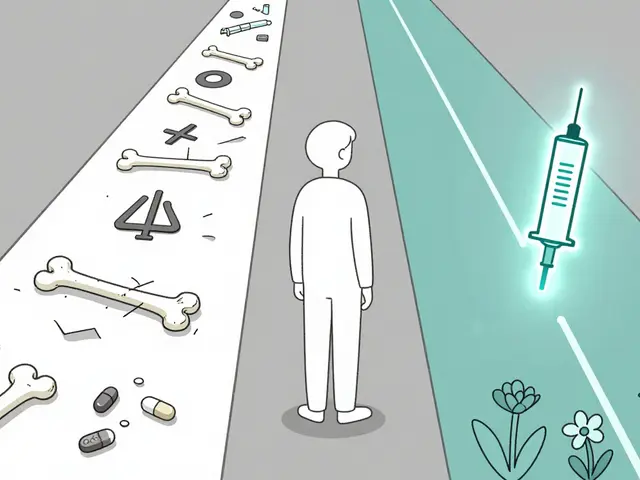
Countries like Canada and Germany use reference pricing. They look at what other nations pay for the same drug - and cap their own prices at that level. Japan negotiates prices annually. The UK’s National Health Service has a single buyer for all drugs. They don’t have PBMs. No rebates. No list prices. Just one fair price.The U.S. system is the outlier. It’s not broken - it’s working exactly as designed. The design? Profit over affordability. The result? One in four Americans says they’ve skipped a dose, cut a pill in half, or gone without a prescription because they couldn’t afford it. That’s not a personal failure. That’s a policy failure.
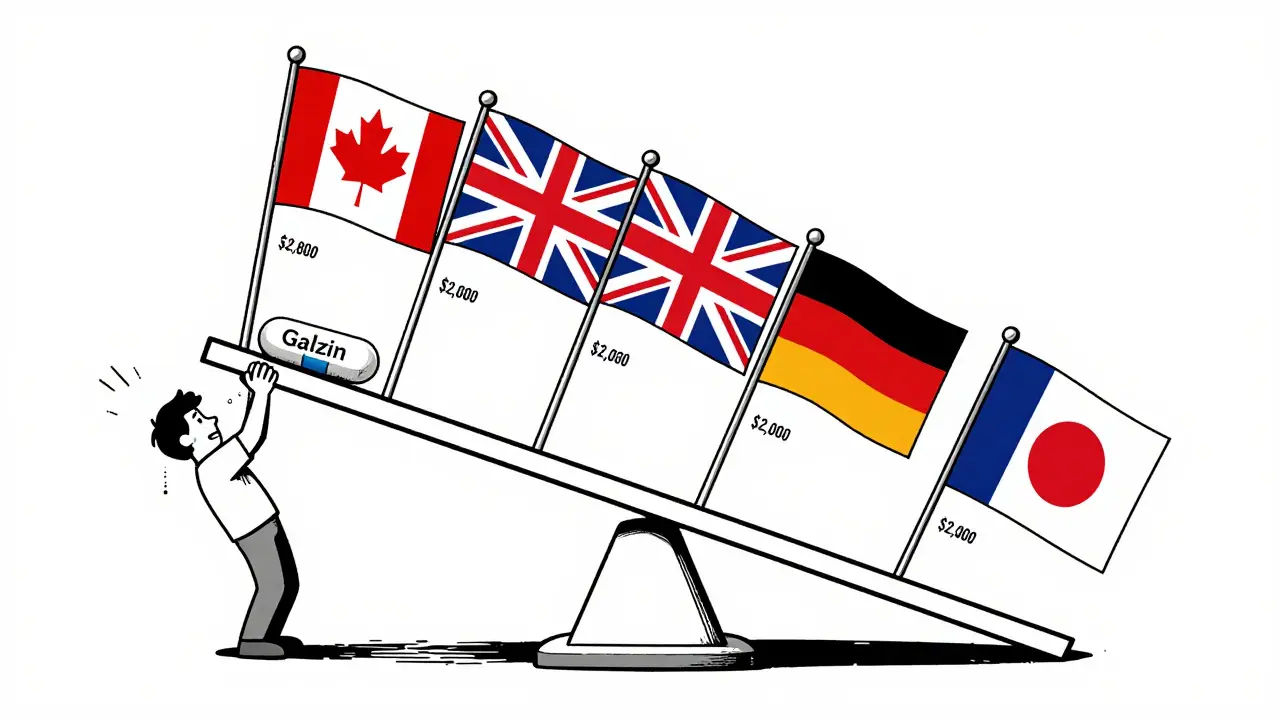
What’s Next? The Battle Over Project 2025
The fight isn’t over. The conservative Project 2025 plan proposes cutting Medicare drug benefits, eliminating the inflation rebate, and allowing PBMs to keep more of their rebates. According to the Center for American Progress, this would raise costs for 18.5 million seniors and people with disabilities.Meanwhile, Senator Sanders’ Prescription Drug Price Relief Act - introduced in May 2025 - would cap U.S. drug prices at the average of what they cost in Canada, the UK, Germany, France, and Japan. It’s simple. It’s fair. And it’s been blocked in Congress since day one.
Drug companies argue that high prices fund innovation. But the numbers show otherwise. In 2024, the top 10 pharmaceutical companies spent $35 billion on R&D - and $58 billion on marketing and profits. That’s 66% more on advertising than on research. Meanwhile, patients are dying because they can’t afford their insulin.
The Human Cost
CMS Administrator Chiquita Brooks-LaSure said the $2,000 annual out-of-pocket cap for Medicare Part D - starting in 2025 - will be “life-changing.” But that cap doesn’t help people under 65. It doesn’t help the 40 million Americans without insurance. It doesn’t help those on high-deductible plans who pay full list price before their deductible is met.Real people are making real choices. A diabetic in Ohio chooses between insulin and her child’s school supplies. A cancer patient in Texas skips doses to stretch his supply. A veteran in Florida pays $1,200 for his thyroid medication - the same pill that costs $180 in Mexico.
This isn’t about politics. It’s about survival. And the system is rigged to make sure the companies that make the drugs - not the people who need them - come out ahead.


Comments
Coral Bosley
This system is a cancer. I watched my mother skip insulin doses because her copay jumped from $30 to $280 in two years. She wasn’t lazy. She wasn’t irresponsible. She was just out of options. And the people who profit from this? They’re on yachts while we’re choosing between meds and groceries.
They call it capitalism. I call it cruelty dressed in a suit.
No emoticons. No sugarcoating. This is real life.
January 21, 2026 AT 03:37
Steve Hesketh
From Lagos to the heart of America - I see the same pain. My cousin in Brooklyn couldn’t afford his asthma inhaler last winter. He used a neighbor’s old one until it ran out. That’s not healthcare. That’s survival theater.
But here’s the truth: change is coming. Not because politicians woke up - but because people like you and me are finally talking. Loud. Clear. Unafraid.
We are the tide. And the tide is rising.
January 22, 2026 AT 05:53
Philip Williams
While the emotional narratives are compelling, it is essential to contextualize the economic structure underpinning pharmaceutical innovation. The R&D cycle for a single drug averages 12 years and costs approximately $2.6 billion. Without the ability to recoup these investments through pricing flexibility, the incentive structure collapses.
Furthermore, the claim that U.S. patients subsidize global R&D is empirically supported by OECD data - which shows that lower-priced markets benefit from innovations initially funded by American consumers. This is not exploitation; it is an unintended consequence of market asymmetry.
January 22, 2026 AT 11:20
Barbara Mahone
The PBM model is a masterclass in obfuscation. List price. Rebate. Net price. Copay. Deductible. Out-of-pocket. Each term is a trapdoor.
My pharmacy told me my $1,200 insulin was covered - until I got the bill. Turns out, the ‘discount’ only applied after I paid the full list price. The PBM kept the rebate. The drugmaker got paid. I got the bill.
It’s not broken. It’s engineered.
January 24, 2026 AT 00:06
MARILYN ONEILL
Ugh. Another ‘poor me’ post. You think other countries have magic? They just ration care. Wait until you need a hip replacement there. No one’s stopping you from moving to Canada. Just don’t cry when your waitlist is 3 years long.
And PBMs? They save you money. You just don’t see it because you’re too busy blaming pharma for your bad choices.
January 24, 2026 AT 10:39
Alex Carletti Gouvea
Why do we even care what Germany pays? They don’t have the same innovation ecosystem. We build the drugs. They copy them. Then they act like they’re moral giants because they pay less.
Let’s stop pretending this is about fairness. It’s about envy dressed as justice.
And if you can’t afford your meds, get a better job. Stop blaming the people who made them.
January 25, 2026 AT 08:53
Dee Monroe
There’s a deeper truth here, one that doesn’t fit neatly into policy debates or lobbying graphs. We’ve turned medicine into a commodity - not a right, not a care, not a human act. We’ve replaced compassion with contracts, and dignity with deductibles.
When a child’s life is measured in copay thresholds, we’ve lost something irreplaceable. Not just money. Not just policy. But soul.
It’s not about who pays more. It’s about who gets to live.
And maybe, just maybe, the real innovation we need isn’t in a lab - it’s in our collective conscience.
January 25, 2026 AT 09:21
Jerry Rodrigues
Galzin costs $88k here and $1.4k in the UK. Same pill. Same factory. Same box.
That’s not capitalism. That’s theft.
And the fact that we’re still arguing about it? That’s the real tragedy.
January 27, 2026 AT 08:12
Uju Megafu
Oh please. You think this is new? The pharma industry has been laughing at us since the 80s. And now you’re shocked? Wake up. This was planned. Every loophole. Every lobbyist. Every ‘bipartisan compromise’ that gutted price controls.
You think Sanders’ bill got blocked because of ‘process’? No. It got blocked because the CEOs own half the Congress.
And don’t even get me started on PBMs. They’re the real monsters. They’re the ones who make the system work - by making it worse.
January 27, 2026 AT 15:38
Jarrod Flesch
Just came back from Sydney - paid $25 AUD for my asthma inhaler. Same brand. Same dose. Same bottle.
Here? $400. And my insurance says it’s ‘covered.’ 😒
Fun fact: Australia caps prices based on what 5 other countries pay. We could do that tomorrow. But we won’t. Because profit > people. Again.
Still love this country. Just not this part of it.
January 28, 2026 AT 14:35
Stephen Rock
Let’s be real - no one gives a shit about Galzin. It’s a rare disease drug. The real outrage is Ozempic. People are mad because they can’t get fat drugs for free.
And the fact that you think $1,350/month is outrageous? Try paying for a kidney transplant. That’s where the real horror is.
Stop crying about pills. Start crying about the fact that your neighbor’s kid needs a liver and you’re too busy yelling about insulin.
January 30, 2026 AT 10:12
Glenda Marínez Granados
Oh wow. The government can’t negotiate prices? How novel.
Next you’ll tell me the sun rises in the east and the moon is made of cheese.
And yes, I know - the same pill costs $1,400 in the UK. But here’s the kicker: they also ration it. They don’t give it to everyone who asks. They wait. They assess. They decide.
So we’re supposed to be grateful for being the land of the free - where you can die on your own dime? Thanks, America.
😂
January 31, 2026 AT 18:11
Yuri Hyuga
The UK’s NHS negotiates every drug annually - and the result? Lower prices, wider access, and a system that doesn’t bankrupt families. We don’t have PBMs. We don’t have list prices. We have one simple rule: the drug must be clinically effective and cost-effective.
It’s not perfect. But it’s humane.
And yes - we still innovate. We just don’t charge $88,000 for a pill that costs $2 to make.
Maybe it’s time we stop pretending the U.S. model is a gold standard. It’s not. It’s a cautionary tale.
❤️
February 2, 2026 AT 09:45
Sangeeta Isaac
so like… pbms are just middlemen who make the price go up by pretending to lower it??
and we’re supposed to be surprised? lol
my grandma paid $1200 for her diabetes med last year. the pBM said ‘we saved you 40%’ - but she still paid $1200. because the list price was $2000. so they saved her… by making it worse.
so… who’s the real villain here? the pharma execs? or the guys who get rich off the confusion?
also why is this still a thing??
February 3, 2026 AT 21:49
Ben McKibbin
Let’s cut through the noise. The Inflation Reduction Act’s negotiation cap is a bandage on a gunshot wound. 20 drugs out of 10,000? That’s not reform - it’s theater.
But here’s what’s actually working: states like California and Colorado are now using reference pricing. They’re looking at international prices and capping their Medicaid payments. It’s working. Patients are saving 60-80%.
The federal government is dragging its feet. But the states? They’re stepping up.
This isn’t about politics. It’s about who’s willing to act - not just tweet.
February 5, 2026 AT 16:31
Coral Bosley
Ben - you’re right. States are doing what the feds won’t. But what happens when a diabetic in Texas needs a drug that’s capped in Colorado but not in her state? She still dies.
That’s the problem. We’re patching holes while the whole ship is sinking.
And now the GOP wants to kill the inflation rebate. They’re not just ignoring the problem.
They’re kicking the ladder away.
February 5, 2026 AT 18:44