How Cephalexin Works to Fight Bacterial Infections: The Science Explained
- Colin Hurd
- 31 October 2025
- 12 Comments
Cephalexin doesn’t just kill bacteria-it disrupts their ability to survive and multiply. If you’ve been prescribed this antibiotic for a skin infection, sinus infection, or urinary tract infection, you might wonder how a simple pill can stop something as tiny as bacteria in its tracks. The answer lies in a precise biological trick that’s been refined over decades of medical research.
What Cephalexin Actually Is
Cephalexin is a first-generation cephalosporin antibiotic. That means it belongs to the same family as penicillin, sharing a similar structure and mechanism. Unlike painkillers or fever reducers, antibiotics like cephalexin don’t make you feel better directly-they target the root cause: the bacteria making you sick.
It’s not effective against viruses. That’s why it won’t help with colds, flu, or most sore throats caused by viruses. It only works on bacterial infections. When doctors prescribe it, they’re targeting specific types of bacteria that are known to respond to cephalosporins-like Staphylococcus aureus, Streptococcus pyogenes, and some strains of E. coli and Klebsiella.
How Cephalexin Attacks Bacteria
Bacteria don’t just float around freely. To survive and multiply, they need to build a strong outer shell called a cell wall. This wall isn’t just protection-it’s what keeps the bacteria from bursting under its own internal pressure. Think of it like a balloon filled with water. Without a strong rubber surface, it pops.
Cephalexin steps in by blocking the enzymes bacteria use to build and repair this wall. Specifically, it binds to proteins called penicillin-binding proteins (PBPs). These proteins are like construction workers assembling the wall’s bricks. When cephalexin latches onto them, the workers can’t do their job. The wall becomes weak, uneven, and full of gaps.
As the bacteria keep growing and dividing, the pressure inside builds. Without a solid wall, they literally explode. This process is called bactericidal action-meaning it kills bacteria, not just slows them down.
Why It Doesn’t Hurt Human Cells
You might wonder: if it breaks cell walls, why doesn’t it break your cells too? The answer is simple-human cells don’t have cell walls. We have cell membranes, which are flexible and made of lipids and proteins. Cephalexin only recognizes and attacks the specific chemical structure found in bacterial cell walls. That’s what makes it safe for human use.
This targeted approach is why antibiotics like cephalexin have been used safely for over 50 years. They exploit a biological difference between us and the bacteria we’re fighting. It’s not magic-it’s chemistry.
How Fast Does It Work?
Most people start feeling better within 24 to 48 hours of taking cephalexin. But that doesn’t mean the infection is gone. The bacteria may be dying off quickly, but some are still hanging on. Stopping the course early is the most common reason infections come back stronger.
Studies show that completing the full 7- to 10-day course reduces the chance of recurrence by over 60%. Even if your fever’s gone and the rash has faded, the remaining bacteria can develop resistance if they’re not fully wiped out. That’s why doctors insist on finishing the prescription-even if you feel fine.
Who Should Avoid Cephalexin
While cephalexin is generally safe, it’s not for everyone. If you’ve ever had a serious allergic reaction to penicillin or another cephalosporin, you should avoid it. About 5% to 10% of people with penicillin allergies also react to cephalosporins like cephalexin.
Signs of an allergic reaction include hives, swelling of the face or throat, trouble breathing, or a severe skin rash. If you experience any of these, stop taking it immediately and get medical help.
People with kidney problems may need a lower dose. Cephalexin is cleared from the body by the kidneys. If your kidneys aren’t working well, the drug can build up in your system and cause side effects like nausea, dizziness, or even seizures in rare cases.
Common Side Effects and What to Do
The most common side effects are mild and temporary: diarrhea, nausea, vomiting, or stomach upset. These happen because cephalexin doesn’t just kill the bad bacteria-it also affects some of the good ones in your gut.
For most people, these symptoms fade after a few days. Taking the pill with food can help reduce stomach upset. If diarrhea becomes severe, watery, or bloody, don’t ignore it. It could be a sign of Clostridioides difficile (C. diff) infection, a serious condition that can develop after antibiotic use. Contact your doctor right away if this happens.
Some people report a metallic taste or mild headache. These are rare and usually go away on their own. If side effects are persistent or worsening, talk to your doctor about switching to another antibiotic.

What to Avoid While Taking Cephalexin
There are no major food interactions with cephalexin. You can take it with or without food, though food helps reduce nausea. Alcohol doesn’t directly interfere with cephalexin, but drinking while sick can slow your recovery and worsen dehydration or stomach upset.
Some supplements, like probiotics, may help restore gut balance after antibiotic use. If you want to take them, wait at least two hours after taking cephalexin. That way, the antibiotic doesn’t kill off the beneficial bacteria in the probiotic before they can do their job.
Don’t take antacids or iron supplements at the same time. They can reduce how much cephalexin your body absorbs. Space them out by at least two hours.
When Cephalexin Isn’t the Right Choice
Not all infections respond to cephalexin. If you have a deep skin infection like cellulitis that’s spreading fast, or a bone infection (osteomyelitis), you might need something stronger-like an IV antibiotic.
Some bacteria have evolved to resist cephalexin. Methicillin-resistant Staphylococcus aureus (MRSA), for example, doesn’t respond to it. That’s why doctors sometimes do a culture test before prescribing. If your infection doesn’t improve after 2-3 days, your doctor may switch you to a different antibiotic.
For urinary tract infections caused by certain resistant strains, other drugs like nitrofurantoin or fosfomycin might be more effective. Cephalexin works best for uncomplicated cases.
Why This Matters for Everyday Health
Antibiotic resistance is one of the biggest public health threats today. Every time we misuse antibiotics-taking them for viral infections, skipping doses, or stopping early-we help bacteria learn how to survive them.
Cephalexin is a tool. Used correctly, it saves lives. Used carelessly, it becomes useless. That’s why understanding how it works isn’t just academic-it’s personal. When you finish your course, you’re not just protecting yourself. You’re helping protect your community.
Next time you’re prescribed cephalexin, remember: it’s not a quick fix. It’s a precise, science-backed attack on bacteria. Respect it. Follow the instructions. And let your body do the rest.
Can cephalexin treat a sinus infection?
Yes, cephalexin is commonly prescribed for bacterial sinus infections, especially when caused by Streptococcus pneumoniae or Haemophilus influenzae. But it won’t work if the infection is viral-which is true for most colds. Doctors usually wait a few days to see if symptoms improve on their own before prescribing antibiotics.
Is cephalexin safe during pregnancy?
Cephalexin is classified as Pregnancy Category B, meaning studies in animals haven’t shown harm to the fetus, and human studies haven’t found evidence of risk. It’s often used during pregnancy for infections like UTIs or skin infections when needed. Always consult your doctor before taking any medication while pregnant.
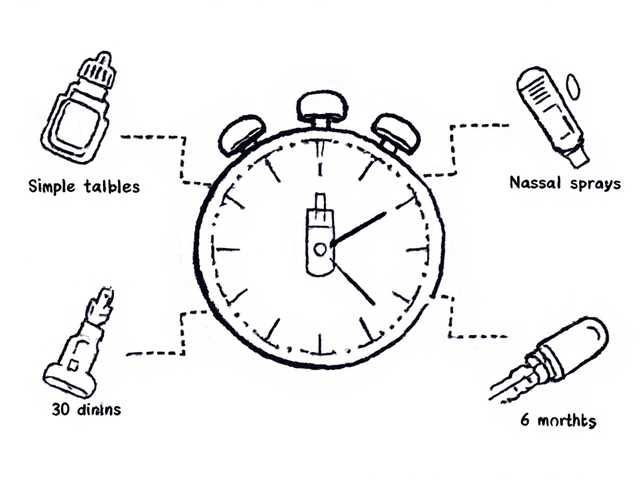
How long does cephalexin stay in your system?
Cephalexin has a half-life of about 1 hour in healthy adults. That means half the drug leaves your bloodstream in an hour. Most of it is cleared within 6 to 8 hours. But even after it’s gone from your blood, it continues to work at the infection site for up to 24 hours. That’s why dosing every 6 to 12 hours is effective.
Can you drink alcohol while taking cephalexin?
There’s no dangerous interaction between cephalexin and alcohol, unlike with some other antibiotics like metronidazole. However, alcohol can weaken your immune system and dehydrate you, which may slow your recovery. It’s best to avoid it while you’re sick and taking antibiotics.
Does cephalexin cause yeast infections?
Yes, it can. By killing off good bacteria in the gut and vagina, cephalexin can allow yeast (Candida) to overgrow. Women may notice itching, discharge, or discomfort. Over-the-counter antifungal treatments can help, but if symptoms persist, talk to your doctor. Taking probiotics may reduce the risk.
What happens if I miss a dose of cephalexin?
If you miss a dose, take it as soon as you remember. But if it’s close to your next scheduled dose, skip the missed one and go back to your regular schedule. Don’t double up-it increases side effects without improving effectiveness. Consistent dosing keeps drug levels steady in your blood to fight the infection.


Comments
Dade Hughston
So cephalexin just makes bacteria explode like little soap bubbles huh
that’s wild i always thought antibiotics were like little soldiers shooting guns at germs
now i feel like i’m watching a sci fi movie where the aliens get popped by a laser pen
also why do doctors make us take it for 10 days if we feel better in 2
my uncle took it for 3 days and said he was fine
then he got sick again and blamed the pharmacy
he’s still mad they didn’t give him the ‘stronger version’
also i think my dog took cephalexin once and started dancing
not kidding he was doing the worm
maybe it’s a side effect
or maybe he was just happy to be alive
either way i’m not giving my cat this stuff
November 1, 2025 AT 02:55
Jim Peddle
Let’s be clear: this is textbook pharmaceutical propaganda dressed as science.
The ‘cell wall’ explanation is a sanitized version meant to soothe the public. The real mechanism involves disrupting peptidoglycan synthesis via transpeptidase inhibition - a detail the FDA quietly omits because most people can’t pronounce ‘transpeptidase’.
And don’t get me started on the ‘bactericidal’ claim. That’s just marketing speak for ‘we killed some bacteria but we don’t know which ones or why they came back’.
Studies show up to 40% of ‘resolved’ infections involve residual biofilm colonies that survive antibiotic exposure - yet we’re told to ‘finish the course’ like obedient children.
The truth? Antibiotics are a blunt instrument. We’re playing Russian roulette with our microbiome.
And yes - human cells don’t have walls. But they do have mitochondria. And guess what? Cephalexin can disrupt mitochondrial ribosomes at high doses. It’s just not listed on the label.
They don’t want you to know that.
November 2, 2025 AT 14:37
S Love
This is one of the clearest explanations of cephalexin I’ve ever read - thank you for taking the time to break it down like this.
So many people think antibiotics are ‘magic pills’ that just make you feel better, but understanding how they actually work helps you respect them - and use them responsibly.
The cell wall analogy with the balloon is brilliant. It’s simple, visual, and accurate.
And you’re absolutely right about finishing the course. It’s not about feeling better - it’s about making sure every last bacterium is gone before it has a chance to mutate and fight back.
Antibiotic resistance isn’t science fiction. It’s happening right now, in hospitals and homes, because people stop taking their meds when they ‘feel fine’.
If you’re prescribed this, take it. Don’t skip. Don’t share. Don’t save it for next time.
It’s not just your health - it’s everyone’s.
November 4, 2025 AT 07:44
Pritesh Mehta
Western medicine always talks about ‘killing bacteria’ like it’s a war - but in India we’ve known for centuries that balance is everything.
Antibiotics are like using a flamethrower to kill a single ant in your kitchen.
You’ll get rid of the ant - but burn down the house.
Our ancestors used turmeric, neem, and honey - natural antimicrobials that didn’t destroy the entire ecosystem inside you.
Why do we think poisoning our microbiome is the answer?
Cephalexin may work - but at what cost?
Your gut flora is your second brain. Your immune system lives there.
And now you’re told to take probiotics to ‘fix’ what the drug broke.
That’s not medicine. That’s damage control.
India has lower antibiotic resistance rates because we don’t overuse these drugs.
We wait. We observe. We heal with nature first.
Maybe the West should learn from the East - instead of exporting its chemical arrogance.
November 4, 2025 AT 14:25
Billy Tiger
Why do they keep saying it doesn't work on viruses when everyone knows colds are just bacteria in disguise
Doctors are just scared to admit they don't know what they're doing
I took cephalexin for my cold last winter and felt better in 12 hours
They just lie to sell more pills
And the whole 'finish the course' thing is a scam to make you buy more
My cousin took half and saved the rest for next time and it worked fine
Why are they so afraid of people being smart
Also why is it called cephalexin why not just call it killgerm
They want you confused
It's all corporate control
November 4, 2025 AT 17:38
Katie Ring
It’s not just about killing bacteria - it’s about power.
Who decides what’s ‘infection’ and what’s ‘normal flora’?
Who profits when we’re told our bodies are ‘invaded’?
Why are we taught to fear microbes instead of coexist with them?
Cephalexin doesn’t ‘fix’ anything - it temporarily suppresses a symptom while ignoring the root: immune weakness, poor diet, chronic stress.
We treat the symptom like a villain - not a signal.
And then we’re surprised when the infection comes back - stronger - after we’ve wiped out half our microbiome.
This isn’t science. It’s colonial medicine - treating the body like a battlefield instead of a living system.
We need to stop glorifying destruction and start honoring balance.
Respect the bacteria. Respect your body.
Healing isn’t about erasing - it’s about restoring.
November 6, 2025 AT 03:59
Adarsha Foundation
Thank you for this thoughtful breakdown. I’ve been prescribed cephalexin twice and never fully understood how it worked.
Now I see it’s not about ‘fighting’ bacteria like enemies - but about interrupting a process that’s unique to them.
It’s elegant, really. Nature gave us a way to target what makes them different from us.
I also appreciate the note about probiotics - I started taking them after my last course and noticed less stomach upset.
And yes, finishing the full course matters. I once stopped early because I felt fine - and got sick again two weeks later.
It was worse the second time.
Learning from that changed how I approach health.
Thanks again for the clarity.
November 7, 2025 AT 20:52
Alex Sherman
Let’s be honest - this whole ‘antibiotic resistance’ narrative is just fearmongering to keep people obedient.
Who benefits from making you feel guilty for stopping early?
Pharma, obviously.
And the ‘science’ here? It’s just a story told to make you trust pills more than your own body.
I’ve never finished an antibiotic course - and I’ve never had a serious infection.
My immune system is stronger than theirs.
They want you dependent.
They want you afraid.
Don’t be fooled.
Listen to your body - not your doctor.
And if you feel better - stop.
November 9, 2025 AT 02:22
Oliver Myers
This is so well-written - thank you so much for taking the time to explain this in such a clear, kind way!
I’ve had cephalexin for a UTI last year and honestly, I didn’t know any of this - I just took the pills because the doctor said so.
Now I feel way more informed - and honestly, a little more responsible.
I did end up getting a yeast infection after, which was annoying - but I found out about probiotics and started taking them, and it made a huge difference.
Also, I totally agree about not skipping doses - I missed one once and felt weirdly off for a day, like my body was confused.
It’s wild how something so small can have such a big impact.
Thank you for helping people understand this - not just the ‘how’ but the ‘why’.
You made me feel like I can actually take care of myself - not just follow orders.
November 9, 2025 AT 07:44
John Concepcion
Lmao you really wrote a whole essay on how a pill makes bacteria pop like popcorn
congrats you just described the most basic biology class thing ever
and now you wanna make us feel guilty for not taking 10 pills we don’t need
bro i took this for a sinus infection and felt fine after 3 days
the rest were just extra money for big pharma
and the ‘yeast infection’ thing? that’s just your body saying ‘hey i’m not a petri dish’
stop drinking the kool-aid
your immune system doesn’t need a chemical vacation
just eat yogurt and chill
November 10, 2025 AT 00:27
Caitlin Stewart
I’ve been on cephalexin three times - for skin infections, UTIs, and after dental work.
Each time, I was surprised how quickly it worked - but also how much it messed with my digestion.
I started taking a high-quality probiotic 2 hours after each dose, and it made a world of difference.
Also, I never realized how important it was to finish the course until I got sick again after stopping early.
That second infection was way worse.
It’s not about fear - it’s about respect.
Respect for the medicine. Respect for your body. Respect for the bacteria that are trying to survive too.
This post helped me see it all more clearly.
Thank you.
November 11, 2025 AT 16:24
Emmalee Amthor
What if the real enemy isn’t the bacteria - but the idea that we need to ‘kill’ everything?
Maybe we’re not meant to eradicate - but to co-evolve.
Cephalexin is a tool - yes - but tools shape the user as much as the problem.
We’ve been trained to see illness as an invasion - not a conversation.
What if our bodies are trying to tell us something?
That we’re stressed?
That we’re tired?
That we’ve forgotten how to rest?
Antibiotics silence the symptom - but never ask why it showed up.
I don’t reject cephalexin - I reject the mindset that says ‘kill it and move on’.
True healing asks deeper questions.
And maybe… we’re not supposed to be so quick to fix.
November 11, 2025 AT 22:12